
Racial/ethnic disparities, body weight, and psychosocial antecedents that predict women’s failure to meet Pap test screening national recommendations
Introduction
Cervical cancer is the second most common cancer among women in developing countries with an estimated 445,000 new cases in 2012 and accounting for a 7.5% of female cancer mortality (1). During 2008–2012 the cervical cancer incidence rate was 7.7 per 100,000 women per year and mortality from the disease was 2.3 per 100,000 persons per year (2). By the American Cancer Society’s estimation, in 2016, 12,990 American women will be diagnosed with cervical cancer and 4,120 women will die from the disease (3). Further, certain racial and ethnic groups have experienced disproportionately higher rates of cervical cancer than Caucasians. The uncorrected rate for cervical cancer per 100,000 women by race/ethnicity is: 4.0 in African American, 2.5 in Hispanic and 2.1 in White (2).
Over the last 50 years the Papanicolaou (Pap) test has been considered an effective screening tool for early diagnosis of cervical cancer (4). The U.S. Preventive Service Task Force (USPSTF) recommends a Pap test every three years for women ages 21–65 (5). However, from 2008 to 2013 cervical cancer screening rates declined from 84.5% to 80.7% (6). Such a decrease in screening is concerning, particularly when the nation’s Healthy People 2020 cervical cancer screening target of 93% has yet to be met (7).
With the aims of reducing morbidity and mortality of cervical cancer, a considerable amount of research has focused on understanding the factors that predict Pap test screening behaviors (8-10). Researchers had utilized several theoretical frameworks, including the Health Belief Model (10-14), Transtheoretical (15), and Protection Motivation Theory (8) to explore factors that promote/prohibit receiving Pap test. These studies have identified several factors that are associated with cervical cancer screening: age—women ages 25–44 were more likely to receive a Pap test than those 45 years old or more (13); knowledge—knowing about Pap tests were positively associated with Pap test obtainment (16); education level—women with 12 years or more of education had higher likelihood of receiving a Pap (17); number of sex partners—women who had more than one sexual partners had a smaller likelihood of receiving a Pap test (9); use of contraceptives—women who used contraceptives were more likely to receive a Pap test (18); perceived severity—women who believed that had a higher perceived severity of getting cervical cancer had a higher likelihood of receiving a Pap test (11); perceived barriers—women who had higher perceived barriers to getting screened were less likely to receive a Pap test (11,13); and perceived risk—women who perceived themselves more at risk for developing cervical cancer were more likely to receive a Pap test (19). These findings demonstrated the multidimensional nature of Pap test screening behaviors.
Body mass index (BMI) has also been identified to be associated with low Pap test screening adherence (20-23). Research has shown that women with a BMI >30 kg/m2 were less likely to receive a Pap test than women who had a BMI <30 kg/m2 [odds ratio (OR) =0.67; 95% confidence interval (CI), 0.49–0.93] (20). Also, Ferrante and colleagues (21) have identified that women with a BMI >30 kg/m2 were less likely to follow through with a physician’s Pap test recommendation than women with a BMI 18.5 to <25 kg/m2. Compared with individuals BMI 18.5 to <25 kg/m2, women who had a BMI ≥40.0 kg/m2 were less likely to undergo Pap test screening (RR =0.94; 95% CI, 0.87–0.99). The majority of these studies examined the association of Pap test screening behavior in women with a BMI >30 kg/m2 in relation to women with a BMI 18.5 to <25 kg/m2 (20-22) or did not include those classified as underweight individuals in the analysis (21,22).
Recent research also suggests that worry, depression, and anxiety, may also affect an individual’s adoption of a health protective behavior (24,25). Findings by Kelly and colleagues (26) showed that increased worry about cancer was negatively associated with regular Pap test screening (OR =0.41; 95% CI, 0.19–0.88). Additionally, a few studies have examined the association of diagnosed psychological disorders on Pap test screening behavior. A systematic literature review indicated that women with mental illness were less likely to have had cervical cancer screenings than those without a mental health diagnoses (24). Research has shown that women with serious psychological distress (SPD) had significantly lower odds to obtain Pap smear than those without SPD (OR =0.59; 95% CI, 0.45–0.77) (25). Another study identified that schizophrenia was negatively associated with having a Pap test (OR =0.70; 95% CI, 0.65–0.75) (27). As part of their limitations, these studies have been criticized for using small sample sizes and including only participants with diagnosed mental disorders, thereby omitting individuals who are under or undiagnosed with mental illness (24,25,28).
The purpose of this study was to predict the behavioral and demographic factors associated with failure to meet Pap test screening national recommendations. To our knowledge, no study has examined factors in predicting women’s failure to meet Pap test screening national recommendations, especially when individuals with BMI classified as underweight and normal weight or with anxiety and depression. These two psychological states usually coexist and are the most common mental disorders present in the population (29).
Previous research has examined Pap test screening behaviors among African Americans and Hispanics (30). To our knowledge, there is a dearth of research exploring Pap test screening behaviors among Asian Americans. This is concerning as an analysis by Healthy People 2020 have indicated that, compared with other race/ethnicities including African American (82.3%), Asian American women are getting screened the least (70.5%) (7). Our study adds to current literature through the examination of four major race/ethnic groups, Asian American, African Americans, Hispanics, and Whites, on the proportion of failure to meet Pap test screening recommendations.
Methods
Since 2003, the National Cancer Institute’s (NCI) Health Information National Trends Survey (HINTS) has been gathering data for the usage of cancer-related information by the public. The survey has multiple roles including providing updates on trends in health needs and information opportunities, assessing cancer communication approach and use, and providing information about perceived cancer risk (31). During 2012 to 2014 HINTS has had four cycles.
We analyzed latest HINTS 4 Cycle 4 data, out of a nationally representative sample of U.S. adults (N=3,677). The HINTS 4 sample design consisted of a two-stage mail survey, using the Next Birthday Method for respondent selection (32). A total of four mailings were sent out as part of Cycle 4, with data collection beginning in August 2014 and ending in November 2014. Reminder postcards were sent after the first mailing, and only non-respondents received subsequent survey mailings. The detailed methodology was published elsewhere (32).
Measures
The outcome variable of this study is whether a woman failed to meet the national recommendations for Pap test screening. In HINTS 4 Cycle 4, Pap test screening behavior was measured by asking participants: “How long ago did you have your most recent Pap test to check for cervical cancer?” Possible responses for this question include: “A year ago or less”, “More than 1, up to 2 years ago”, “More than 2, up to 3 years ago”, “More than 3, up to 5 years ago”, “More than 5 years ago”, and “I have never had a Pap test”. This question was dichotomized to indicate whether women 21 to 65 years old met the Pap test recommendation of ≤3 years since the most recent screening (5) or failed to meet the national recommendation.
Through bivariate examination of the HINTS 4 Cycle 4 with consideration of health behavior theories such as Health Belief Model, Social Cognitive Theory, Integrated Behavioral Model, and Protection Motivation Theory, possible psychosocial and demographic correlates of meeting the Pap test national recommendation were identified and examined. These potential variables included questions from multiple sections in HINTS 4 Cycle 4: Looking for Health Information, Your Health Care, Medical Research, Your Overall Health, Women and Cancer, Screening for Cancer, Beliefs about Cancer, and demographics.
Three items from the section Looking for Health Information include—(I) “Based on the results of your most recent search for information about cancer, how much do you agree or disagree with each of the following statements?”: (i) it took a lot of effort to get the information you needed; (ii) you felt frustrated during your search for the information; (iii) you were concerned about the quality of the information; and (iv) the information you found was hard to understand (measured on a 4-point Likert scale from strongly agree to strongly disagree). (II) Confidence in getting advice or information about cancer (measured on a 5-point Likert scale from completely confident to not confident at all). (III) Trust information about cancer from each of the following: (i) from a doctor; (ii) from family; (iii) from newspapers or magazines; (iv) from the radio; (v) from the internet; (vi) from the television; (vii) form the government; (viii) from charities; and (ix) from religious organizations (measured on a 4-point Likert scale from not at all to a lot).
One item from the section on Your Health Care was analyzed. The questions asked women about the last time they visited a doctor for a routine checkup. The response options include within past year, within past 2 years, within past 5 years, 5 or more years ago, don’t know, and never. Responses were dichotomized as two years or less and more than two years.
Within the Medical Research section, two questions regarding if participants believe health behaviors (e.g., diet, exercise and smoking) and genetics determine if an individual develops cancer were examined. These items were measured on a 4-point Likert scale ranging from not at all to a lot.
Six items were evaluated from the Your Overall Health section, covering participant’s perceived general health (excellent to poor), confidence to take care of her own health (measured on a 5-point Likert scale from completely confident to not confident at all), height and weight, emotional support, social support, and anxiety and depression. Height and weight were used to calculate the BMI of women. These values were then used to classify respondents as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2) (33).
Anxiety and depression were measured via a four-item inventory called the Patient Health Questionnaire (PHQ-4). The PHQ-4 draws two items measuring anxiety from the Generalized Anxiety Disorder-2 scale (GAD-2) and two items measuring depression from the ‘Patient Health Questionnaire-2’ (PHQ-2) (29). HINTS 4 Cycle 4 asked participants to indicate on a 4-point scale: (I) nearly every day; (II) more than half the days; (III) several days; and (IV) not at all if they had been bothered by any of the following problems over the past two weeks—(I) to measure anxiety: (i) feeling nervous, anxious, or on edge; and (ii) not being able to stop or control worrying. And (II) to measure depression: (i) having little interest or pleasure in doing things; and (ii) feeling down, depressed, or hopeless. The PHQ-4 has a proper internal reliability higher than 0.80 (29). The PHQ-4 score was calculated as the sum of the depression and anxiety responses and used to classify the severity of participants’ anxiety and depression on a scale ranging from none, mild, moderate and severe.
Three items from Women and Cancer portion of the survey were examined. Participants were asked whether or not a doctor has told them they could choose to have a Pap test. Additionally, women were asked about their most recent mammography. This item was dichotomized to indicate whether women ≥50 years old met the U.S. Preventive Services Task Force mammography screening recommendation of ≤2 years since most recent screening (34) or failed to meet national recommendation of >2 years since most recent screening.
Only one question related to human papillomavirus (HPV) vaccine was evaluated from the Screening for Cancer section. This item asked women if they ever heard of the cervical cancer vaccine or HPV shot.
Within the Beliefs about Cancer section three questions were examined. The respondents were asked to indicate true or false if medical tests or exams (including Pap tests) can check for early signs of cancer. Other items of this section that were evaluated included: if women had ever been diagnosed with cancer (yes/no), perceived likelihood of getting cancer (measured on a 5-point Likert scale from very unlikely to very likely), and worry about getting cancer (measured on a 5-point Likert scale from not at all to extremely). Demographics variables examined in the study included age, marital status, income range, education level, and race/ethnicity.
Statistical procedure
Analyses were conducted using Statistical Package for the Social Sciences (SPSS), version 21.0. Cases were selected to include women ages 21–65 years old, who had no history of cervical cancer. All missing values were excluded from the analyses and a population weighting factor from the HINTS data set was applied.
Descriptive statistics were used to summarize demographic characteristics of survey respondents to include frequencies and percentages. Bivariate analyses including odds ratio (OR), Chi-square, and independent sample t-test were performed to evaluate the relationships between failing to meet Pap test screening national recommendations and the explanatory variables. Stepwise multiple binary logistic regression was conducted to identify the significant predictors of failing to meet Pap test screening national recommendations among women aged 21–65 who never had cervical cancer.
Results
Of the 3,677 individual respondents to HINTS 4 Cycle 4, 1,521 women were included in the study after excluding males, women who were younger than 21 or older than 65, and women who had cervical cancer. After applying the population weighting factor, the demographic information of the sample showed that Asian American (30.0%) and White women (20.9%) had higher proportions of failing to meet Pap test screening national recommendations compared to African American (15.8%) and Hispanic women (15.4%). Furthermore, analyses indicated that more women aged 50–65 failed to meet Pap test screening national recommendations (22.2%) when compared to women of 36–49 years (16.8%) and of 21–35 years (15.9%).
The majority of women were Caucasian (63.7%), married or living as married (56.9%), was ages 21–35 years old (36.2%), had some college level or more education (70.9%), and had an income of $35,000 or more (64.1%). The prevalence of women who failed to meet Pap test screening national recommendations was 20%.
Table 1 summarizes the bivariate OR and their 95% confidence intervals (CI) for the demographic characteristics associated with failing to meet the Pap test screening national recommendation. Analyses indicated that women who are classified as underweight are about 13 times more likely to have failed to meet the Pap test recommendation (OR =12.706; 95% CI, 12.648–12.764) than obese women. Additionally, bivariate results indicate that women who have never had cancer were about 1.5 times more likely to have failed to meet the Pap test recommendations (OR =1.481; 95% CI, 1.477–1.485) than those who had ever had cancer.

Full table
Women who had less than a high school education were approximately 3 times more likely to have failed to meet the Pap test recommendation (OR 3.44; 95% CI, 3.434–3.446) than those had a college degree or higher. Women who were widowed or single, never been married were about 2 times more likely to have failed to meet the Pap test screening national recommendations (OR =2.066; 95% CI, 2.060–2.072; OR =1.925; 95% CI, 1.923–1.927; respectively) than those who were married or living as married. Women aged 50–65 were about 1.5 times more likely to have failed to meet the Pap test screening national recommendation (OR =1.508; 95% CI, 1.506–1.510) than women aged 21–35.
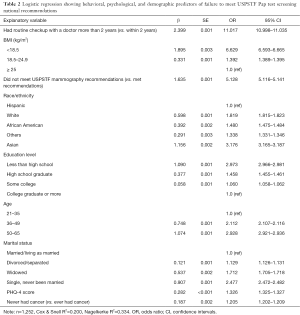
All variables that were significant in the bivariate analyses were included in the multivariate analyses. Table 2 showed the set of behavioral, demographic, and psychological predictors that are significantly correlated with women’s failure to meet the Pap test recommendation. When examining race/ethnicity, results showed that Asian women were about 3 times more likely to have failed to meet Pap test screening national recommendations (OR =3.176; 95% CI, 3.165–3.187) than Hispanic women. White women were around 2 times more likely to have failed to meet Pap test screening national recommendations (OR =1.819; 95% CI, 1.815–1.823) than Hispanic women.
Full table
Women who had a routine check up with their doctor more than two years were about 11 times more likely to fail to meet the Pap test screening national recommendations (OR =11.017; 95% CI, 10.998–11.035) than women who had a recent routine check-up within two years. Results also showed that women who were underweight were about 7 times more likely to fail to meet the Pap test screening national recommendations than women who were overweight/obese (OR =6.629; 95% CI, 6.593–6.665). Further, participants classified as normal weight were more likely to fail to meet the Pap test screening national recommendations than women who were overweight/obese (OR =1.392; 95% CI, 1.389–1.395).
Women who failed to meet USPSTF’s mammography recommendation were about 5 times more likely to fail to meet the Pap test screening national recommendations (OR =5.128; 95% CI, 5.116–5.141) than women who met the mammography screening recommendation. Additionally, women with higher PHQ-4 scores were more likely to have failed to meet the Pap test screening national recommendations (OR =1.326; 95% CI, 1.325–1.327) than women with lower scores.
Further, those who had less than high school education were about 3 times more likely to have failed to meet Pap test screening national recommendations than women who had a college or higher degree (OR =2.973; 95% CI, 2.966–2.981). Additionally, women whose age ranged in 50–65 were about three times (OR =2.928; 95% CI, 2.921–2.936) more likely to have failed to meet Pap test screening national recommendations than women aged 21–35. Also, women who were single, never married were about 2.5 times more likely to have failed to meet Pap test screening national recommendations (OR =2.477; 95% CI, 2.472–2.482) than women who were married or living as married. Results also showed that individuals who indicated that they never had cancer were more likely to have failed to meet Pap test screening national recommendations (OR =1.205; 95% CI, 1.202–1.209) than those who ever had cancer. The combination of the above-mentioned predictors can explain 20% (Cox & Snell R2) or 33.4% (Nagelkerke R2) of the variance when predicting adult woman’s failure to meet the Pap test screening national recommendations.
Conclusions/discussion
The purpose of this study was to identify behavioral, demographic, and psychological factors predicting adult women’s failure to meet Pap test screening national recommendation in a nationally representative sample. To our knowledge, this is the first study to look at the determinants of failing to meet the Pap test screening national recommendations. This study identified a 2% drop in self-reported Pap test screening rate from 2013 (6), highlighting the need for identifying factors that influence the adoption of this health screening behavior.
This current study identified racial/ethnic disparities in failing to meet Pap test screening recommendations. Both Whites and Asian Americans had a higher likelihood of failing to meet Pap test screening recommendations than Hispanic Americans. This is an interesting finding as, above any other race/ethnicity, White women are often seen to meet most screening recommendations. The majority of individuals in this study were White and married/living as married. Because having multiple sex partners is a risk for developing cervical cancer; one can assume that Whites who are married/living as married do not think it is necessary to have a Pap test since they are monogamous.
Prior studies have identified health care utilization barriers faced by Asian American women, including financial, cultural attitude, physical, and language (35). These barriers may play a significant role in Asian women’s failure to meet Pap test screening national recommendations. Future research is suggested to identify barriers faced by Asian Americans that lead to failure to meet Pap test screening recommendations. Additionally, since this group is one of the fastest growing populations in the United States, developing culturally competent interventions is imperative.
Among the behavioral predictors, this study examined associated factors in predicting women’s failure to meet the Pap test recommendation. Analyses revealed that women who were in the underweight and normal weight categories were more likely to have failed to meet Pap test screening national recommendations than those who are overweight/obese. Prior research used normal weight and/or underweight as reference groups (21,22,36). Some studies have also dichotomized body weight (20), combined underweight with normal weight individuals (36), and even excluded those who were underweight (21). In order to assess the proper associations of body weight on Pap test screening behavior caution should be exercised in combining BMI classifications. The current study suggests that proportions be examined before assigning reference groups and combining BMI groups.
In contrast, other studies identified that overweight/obese women had lower rates of Pap test screening (21,22). One can speculate that underweight women may perceive themselves as healthy and not being at risk for cervical cancer. Also, body image issues may hinder underweight individuals to seek a Pap test. Similarly, normal weight women may also consider themselves not susceptible to developing cervical cancer and therefore not seek Pap test screening.
This study also examined symptoms of depression and anxiety through a brief screening tool. Other studies examining Pap test screening behaviors had assessed only depression (20,37) without including anxiety measures. Results of this study indicated that women who had higher PHQ-4 scores were more likely to have failed to meet Pap test screening national recommendations. This finding is consistent with the previous studies on the negative association of symptoms of depression with cervical cancer screening (20,38) and highlights the need for intervention efforts to increase Pap test screening behaviors in this population.
Among the demographic predictors, this study showed a similar tendency in the association between women’s age and receiving Pap test from previous research which reported that women ages 25–44 were found more likely to receive a Pap test than those 45 years old or more (13). This current study showed women aged 50-65 tended to fail to meet Pap test screening national recommendations than the younger age groups.
As exhibited in prior research (39), women with 12 years or more of education had higher likelihood of receiving a Pap test. Similarly our study found women who had less than high school education tended to fail to meet the Pap test recommendations. Unlike previous studies that exhibited married women tend not to receive Pap test than unmarried women (17), our research showed that women who were single and widowed had a higher likelihood to fail to meet Pap test screening national recommendations than those who were currently married.
Another strength of this study is the assessment of the association between meeting the mammography screening recommendation and the Pap test recommendation. Findings indicated that women who failed to meet mammography-screening recommendation had a higher likelihood to fail to meet Pap test screening national recommendations. Moreover, the Healthy People 2020’s unmet goals of mammography (81.1%) (40) and Pap test (93%) (7) screening rates suggest the warranted needs to promote women receiving both types of cancer screenings. As our results show, women whose check up with a doctor were 2 years or longer had a higher likelihood of failure to meet Pap test screening national recommendations. If women are not going to the doctor then they are not getting screened. Identifying the barriers associated with women not visiting the doctor may be key in them not adopting health-screening behaviors. Research has identified that fear, worry, and other negative psychological states may prevent women from being screened (26,41,42). Our findings of the association of symptoms of depression and anxiety with failure to meet Pap test screening recommendations may also be a reason why women are failing to meet mammography-screening recommendations.
This study had notable limitations. This utilization of the secondary data from HINTS 4 Cycle 4 is delimited to the available variables. Important psychosocial variables such as attitudes, subjective norms, perceived control, self-efficacy and alike are not examined. In addition, self-reported data were collected and may have led respondents to under- and over-report, or experience imperfect recall of their Pap test screening date. Additionally, the social desirability bias associated with reporting depression and anxiety symptoms should be considered when interpreting the PHQ-4 results.
The present study makes significant contributions to understanding attributes in women’s failure to meet Pap test screening national recommendations, particularly the influences of racial/ethnic disparities and body weight. Future research is suggested to explore the relationships between other cancer screening behaviors and the factors in Looking for Health Information, Your Health Care, Medical Research, Your Overall Health, Women and Cancer, Screening for Cancer, Beliefs about Cancer, and demographics. Interventions to increase Pap test screening rates among Asian American women, women with a BMI <18.5 kg/m2 or 18.5 to <24.9 kg/m2, and women with symptoms of depression and anxiety would be valuable. Furthermore, the utilization of a health behavior theory such as the Integrated Behavioral Model in researcher-initiate study with original survey data is suggested.
Acknowledgments
The authors thank the National Cancer Institute’s Health Information National Trends Survey program for the study design and data collection.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Tung-Sung Tseng, Dung-Tsa Chen, Hui-Yi Lin) for the series “Social Behavioral and Genetic Risk factors for Cancer” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.10.76). The series “Social Behavioral and Genetic Risk factors for Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the University of Toledo Institutional Review Board (No. 200875) and consent was exempt due to secondary data analysis without any identifier.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Human papillomavirus (HPV) and cervical cancer. Available online: http://www.who.int/mediacentre/factsheets/fs380/en/
- Anderson ARCenters for Disease Control and Prevention (CDC). Top five chemicals resulting in injuries from acute chemical incidents—Hazardous Substances Emergency Events Surveillance, nine states, 1999-2008. MMWR Suppl 2015;64:39-46. [PubMed]
- What are the key statistics about cervical cancer? Available online: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-key-statistics
- Cervical cancer prevention and early detection. Available online: http://www.cancer.org/cancer/cervicalcancer/moreinformation/cervicalcancerpreventionandearlydetection/cervical-cancer-prevention-and-early-detection-cervical-cancer-screening-guidelines
- U.S. Preventive Services Task Force. Screening for cervical cancer: recommendation statement. Am Fam Physician 2012;86:555-9. [PubMed]
- Sabatino SA, White MC, Thompson TD, et al. Cancer screening test use - United States, 2013. MMWR Morb Mortal Wkly Rep 2015;64:464-8. [PubMed]
- Healthy People 2020. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/cancer
- Gu C. Mainland Chinese women's perception of risk of cervical cancer: A model to understand factors determining cervical screening behaviour. Hong Kong. ProQuest Dissertations Publishing: The Chinese University of Hong Kong, 2010.
- Tacken MA, Braspenning JC, Hermens RP, et al. Uptake of cervical cancer screening in The Netherlands is mainly influenced by women's beliefs about the screening and by the inviting organization. Eur J Public Health 2007;17:178-85. [Crossref] [PubMed]
- Kahn JA, Goodman E, Slap GB, et al. Intention to return for papanicolaou smears in adolescent girls and young women. Pediatrics 2001;108:333-41. [Crossref] [PubMed]
- Eaker S, Adami HO, Sparén P. Attitudes to screening for cervical cancer: a population-based study in Sweden. Cancer Causes Control 2001;12:519-28. [Crossref] [PubMed]
- Seow A, Wong ML, Smith WC, et al. Beliefs and attitudes as determinants of cervical cancer screening: a community-based study in Singapore. Prev Med 1995;24:134-41. [Crossref] [PubMed]
- Boonpongmanee C, Jittanoon P. Predictors of Papanicolaou testing in working women in Bangkok, Thailand. Cancer Nurs 2007;30:384-9. [Crossref] [PubMed]
- Byrd TL, Peterson SK, Chavez R, et al. Cervical cancer screening beliefs among young Hispanic women. Prev Med 2004;38:192-7. [Crossref] [PubMed]
- Tung WC, Smith-Gagen J, Lu M, et al. Application of the Transtheoretical Model to Cervical Cancer Screening in Latina Women. J Immigr Minor Health 2016;18:1168-74. [Crossref] [PubMed]
- Armstrong LL. Predicting cervical screening in college women: A test of the Theory of Reasoned Action [Ph.D.]. Missoula: University of Montana; 2001.
- Lee HY, Yang PN, Lee DK, et al. Cervical cancer screening behavior among Hmong-American immigrant women. Am J Health Behav 2015;39:301-7. [Crossref] [PubMed]
- Knops-Dullens T, de Vries N, de Vries H. Reasons for non-attendance in cervical cancer screening programmes: an application of the Integrated Model for Behavioural Change. Eur J Cancer Prev 2007;16:436-45. [Crossref] [PubMed]
- Kim SE, Pérez-Stable EJ, Wong S, et al. Association between cancer risk perception and screening behavior among diverse women. Arch Intern Med 2008;168:728-34. [Crossref] [PubMed]
- Ludman EJ, Ichikawa LE, Simon GE, et al. Breast and cervical cancer screening specific effects of depression and obesity. Am J Prev Med 2010;38:303-10. [Crossref] [PubMed]
- Ferrante JM, Chen PH, Crabtree BF, et al. Cancer screening in women: body mass index and adherence to physician recommendations. Am J Prev Med 2007;32:525-31. [Crossref] [PubMed]
- Wee CC, Phillips RS, McCarthy EP. BMI and cervical cancer screening among white, African-American, and Hispanic women in the United States. Obes Res 2005;13:1275-80. [Crossref] [PubMed]
- Fontaine KR, Heo M, Allison DB. Body weight and cancer screening among women. J Womens Health Gend Based Med 2001;10:463-70. [Crossref] [PubMed]
- Aggarwal A, Pandurangi A, Smith W. Disparities in breast and cervical cancer screening in women with mental illness: a systematic literature review. Am J Prev Med 2013;44:392-8. [Crossref] [PubMed]
- Xiang X. Serious psychological distress as a barrier to cancer screening among women. Womens Health Issues 2015;25:49-55. [Crossref] [PubMed]
- Kelly KM, Schoenberg N, Wilson TD, et al. Cervical cancer worry and screening among appalachian women. J Prim Prev 2015;36:79-92. [Crossref] [PubMed]
- Martens PJ, Chochinov HM, Prior HJ, et al. Are cervical cancer screening rates different for women with schizophrenia? A Manitoba population-based study. Schizophr Res 2009;113:101-6. [Crossref] [PubMed]
- Kessler RC, Berglund PA, Bruce ML, et al. The prevalence and correlates of untreated serious mental illness. Health Serv Res 2001;36:987-1007. [PubMed]
- Kroenke K, Spitzer RL, Williams JB, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009;50:613-21. [PubMed]
- Jennings-Dozier K. Predicting intentions to obtain a Pap smear among African American and Latina women: testing the theory of planned behavior. Nurs Res 1999;48:198-205. [Crossref] [PubMed]
About HINTS - Health Information National Trends Survey 4 (HINTS 4): Cycle 4 methodology report. Available online: http://hints.cancer.gov/docs/Instruments/HINTS_4_Cycle_4_Methodology_Report_Final.pdf
- American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Obesity Expert Panel, 2013. Executive summary: Guidelines (2013) for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society published by the Obesity Society and American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Based on a systematic review from the The Obesity Expert Panel, 2013. Obesity (Silver Spring) 2014;22:S5-39. [Crossref] [PubMed]
- Breast Cancer: Screening. Available online: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1
- Lee S, Martinez G, Ma GX, et al. Barriers to health care access in 13 Asian American communities. Am J Health Behav 2010;34:21-30. [Crossref] [PubMed]
- Hirth JM, Laz TH, Rahman M, et al. Racial/Ethnic Differences Affecting Adherence to Cancer Screening Guidelines Among Women. J Womens Health (Larchmt) 2016;25:371-80. [Crossref] [PubMed]
- Pirraglia PA, Sanyal P, Singer DE, et al. Depressive symptom burden as a barrier to screening for breast and cervical cancers. J Womens Health (Larchmt) 2004;13:731-8. [Crossref] [PubMed]
- Nelson W, Moser RP, Gaffey A, et al. Adherence to cervical cancer screening guidelines for U.S. women aged 25-64: data from the 2005 Health Information National Trends Survey (HINTS). J Womens Health (Larchmt) 2009;18:1759-68. [Crossref] [PubMed]
- Lee J, Seow A, Ling SL, et al. Improving adherence to regular pap smear screening among Asian women: a population-based study in Singapore. Health Educ Behav 2002;29:207-18. [Crossref] [PubMed]
- Cancer. Available online: https://www.healthypeople.gov/2020/data-search/Search-the-Data#objid=4055
- Ackerson K, Pohl J, Low LK. Personal influencing factors associated with pap smear testing and cervical cancer. Policy Polit Nurs Pract 2008;9:50-60. [Crossref] [PubMed]
- Ackerson K. Personal influences that affect motivation in pap smear testing among African American women. J Obstet Gynecol Neonatal Nurs 2010;39:136-46. [Crossref] [PubMed]


