
Poor survival with high-dose chemotherapy and autologous stem cell support in double-hit and double-expressor B-cell lymphomas
Diffuse large B-cell lymphoma (DLBCL) is a heterogeneous disease both in biology and clinical behavior. Approximately two thirds of patients achieve prolonged disease free survival and cure after induction with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) chemoimmunotherapy (1). Much of the research in the field has been devoted to characterizing the biology of those with progressive disease or who ultimately relapse. Aberrations of MYC, BCL2 and BCL6 have been implicated in a proportion of these cases and include both translocations involving these genes as well as abnormal protein expression of MYC and BCL2. In recognition of the unique clinical behavior of translocations involving MYC, BCL2 and BCL6, a provisional entity of high grade B-cell lymphoma (HGBL) with rearrangements of MYC and BCL2 and/or BCL6 has been included in the 2016 revision of the World Health Organization (WHO) classification of lymphoid neoplasms (2). These have been referred to as double-hit lymphomas (DHL), or in the case of DLBCL with co-expression of MYC and BCL2, double-expressor lymphomas (DEL).
In the chemoimmunotherapy era, rearrangements of MYC have been associated with poor survival, especially in the case of concomitant rearrangements of BLC2 or BCL6 (3-6). The presence of BCL2 or BCL6 translocations are not the only factors that influence the prognosis of patients with MYC rearrangements as it also appears that the translocation partner for MYC is of significant importance. Translocations involving a non-IG partner gene have not been associated with a poor prognosis (6,7). A complete response (CR) to induction therapy is associated with an improved prognosis as well, and there is an association between intensive induction regimens and improved prognosis in retrospective analyses (8,9). While there is consensus that R-CHOP is a poor induction regimen for DHL, much of the data supporting alternative regimens are from retrospective series or single arm phase II studies. Increased protein expression of MYC and BCL2 is associated with a poor prognosis and is a much more commonly encountered scenario with up to a third of DLBCL patients affected. While associated with an inferior prognosis, the effect on survival appears to be of a lesser magnitude relative to patients with rearrangements (10-13). The optimal treatment of either group of patients is unknown and the data regarding the efficacy of transplant in this group are scant.
Consolidation with autologous stem cell transplant (ASCT) after salvage chemotherapy has been considered the standard of care in relapsed aggressive lymphomas such as DLBCL for the past 20 years based on results from the Parma study (14). In the chemoimmunotherapy era induction is more successful, but a lower percentage of relapsed patients are salvaged with ASCT. A retrospective analysis was performed of subjects in the randomized Collaborative Trial in Relapsed Aggressive Lymphoma (CORAL) study to investigate the impact of MYC rearrangements on outcome after ASCT. This revealed that subjects with MYC rearrangement had significantly inferior 4-year progression-free survival (PFS) and overall survival (OS) when compared to those without rearrangements. Most of the MYC rearranged cases had an additional translocation and were considered DHLs. An important finding of this study is that the percentage of MYC rearranged patients who achieved a CR was much lower than the rest of the cohort and fewer patients went on to ASCT (15).
Herrera and colleagues present the results of a multicenter, retrospective analysis of all relapsed and refractory DLBCL patients who underwent ASCT and had adequate archival tissue available for IHC and FISH testing. Importantly, all of these patients received prior rituximab as well as anthracycline-based chemotherapy. None of the patients included in the analysis received transplant as consolidation after induction chemoimmunotherapy. DEL was relatively common (44%) in this cohort and was associated with inferior PFS, but not OS when compared to patients without expression of MYC and BCL2. DHL was less common with 10% of patients having rearrangements of MYC and BCL2, BCL6 or both, and 4-year PFS and OS were both inferior when compared to patients who did not have rearrangements. Direct comparison between DHL and DEL reveals statistically inferior PFS and OS in the DHL group of patients. In a Cox model for PFS and OS, DEL and DHL were significantly associated with an inferior PFS and DHL and remission prior to ASCT were associated with OS. While the numbers were small, exploratory analysis did not reveal any prolonged survival in patients with DHL who also had protein expression of MYC and BCL2 (16).
This study highlights several important issues. It demonstrates the inadequacy of salvage chemotherapy followed by ASCT in this population, particularly in DHL. This study also illustrates the importance of distinguishing DEL and DHL. These entities are distinct in biological and clinical behavior, and while DEL without rearrangement has a poor prognosis relative to non-DEL DLBCL, their prognosis is not as poor as those with DHL. Table 1 provides a summary of DEL and DHL. Patients with DEL had a 4-year PFS that was nearly double that of the DHL group. Another important finding in this study is that patients who were not DHL or DEL had favorable outcomes with ASCT. In those patients who do have a CR to salvage chemotherapy, consolidation with ASCT is a reasonable consideration outside of a clinical trial that is specifically designed for these groups, especially in those patients without risk factors and DEL. These findings are likely to be hypothesis generating and will need to be confirmed prospectively.
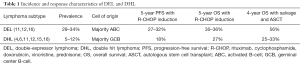
Full table
As the author’s acknowledge, this analysis does have some limitations. It is limited by the small sample size of the DHL population and the retrospective nature. The presence of adequate tissue was absolutely necessary to perform this analysis, however, and the patients without adequate tissue could not have been included. The authors also acknowledge the selection bias present in this study since all of the patients included responded to salvage chemotherapy. The analysis of the CORAL study previously mentioned would suggest that many of these patients do not respond adequately to salvage. A significant percentage of patients with DHL and DEL have refractory disease and would not benefit from transplantation.
Induction chemoimmunotherapy with R-CHOP and ASCT in relapsed and refractory patients are suboptimal treatments for the majority of patients with DEL and DHL. Improved induction and salvage strategies for these groups remain a significant unmet need in the field. Potential treatments to be evaluated in clinical trials include intensification of induction, consolidative transplant in first CR, incorporation of rational, targeted treatments and use of adoptive cellular therapy. Induction with dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide and doxorubicin with rituximab (DA EPOCH-R) has shown preliminary efficacy in a multicenter, single-arm study of patients with MYC rearranged DLBCL. This included all aggressive lymphomas with a MYC rearrangement and showed impressive PFS in patients with MYC rearrangement alone as well as patients with DHL (17). These results should however be taken with some caution given the relatively small sample size, the preliminary nature of the results with short follow-up, and the impact of MYC rearrangement in isolation of other factors. The recently presented results of the Alliance study of R-CHOP versus DA EPOCH-R should also temper enthusiasm for this regimen as well given that there was no difference between the regimens in an unselected group of patients with DLBCL (18). While the correlative biology including DHL and DEL status of patients is not yet available, it is unlikely that there will be large differences when looking at the subgroups provided the patients were well balanced between treatments. It remains somewhat unlikely that intensification of cytotoxic chemotherapy will yield markedly improved responses. Despite the quality of the data, given the poor outcome of patients with DHL, it has been our practice to offer DA EPOCH-R to DHL patients who are eligible for this more intensive therapy. We do not offer it to DEL patients.
Consolidation with ASCT in first CR is another potential treatment that warrants further study. In MYC rearranged patients, subset analysis of consolidative transplant after induction treatment in a retrospective multicenter study failed to show a benefit in terms of OS, although the sample size was small. This analysis also included some patients who underwent allogeneic stem cell transplant (9). Secondary analysis of S9704, which randomized patients to consolidative ASCT versus observation after R-CHOP treatment, did not reveal statistically improved survival with transplant in MYC rearranged patients. There were very few DHL patients who reached randomization and all of these patients fared poorly (19). The present data are insufficient to consider this outside of a clinical trial.
Future targeted treatment regimens are likely to include pathway inhibition as well as immune mediated therapy. BCL2 inhibition is a potentially attractive strategy and preclinical data in DHL cell lines and a murine model suggest efficacy as well as synergy with chemotherapy and other targeted agents (20,21). The National Clinical Trials Network is currently conducting a phase 1 trial combining venetoclax (a bcl-2 inhibitor) with DA R-EPOCH for patients with both DEL and DHL; a follow-up phase 2–3 trial evaluating venetoclax in this setting is planned. Another novel class of targeted agents that have demonstrated activity in MYC driven lymphoma models has been the bromodomain inhibitors (22). Further efficacy and safety data in relapsed and refractory disease are needed with this class of drugs however. Adoptive cellular therapy is another possible treatment modality of interest. Data were presented data at late-breaking abstract session of the American Society of Hematology (ASH) Annual Meeting from a trial of KTE-19 in relapsed and refractory aggressive B-cell lymphomas. A single infusion of autologous anti-CD19 chimeric antigen receptor (CAR) T-cells demonstrated substantial activity in heavily pretreated relapsed and refractory patients, including those who had prior ASCT (23). General concerns regarding CAR T-cells include the acute toxicity burden, potential delays with cellular manufacture, and the durability of response given the short follow up with many of these patients.
While the analysis conducted by Herrera and colleagues is limited by the relatively small sample size and retrospective nature, the uniformity and quality of the pathologic material enhance the impact of this paper in the field of lymphoma. It further highlights the unmet need of DHL and the inadequacy of current standard treatments. The inclusion of high grade lymphoma with rearrangements of MYC, BCL2 and/or BCL6 as a provisional entity in the WHO classification has the potential to foster more clinical and translational investigation in this disease. The study also provides further data to suggest that DEL is associated with a poor prognosis relative to those who lack expression of MYC and BCL2 in the transplant setting. The future may involve a more personalized approach to transplantation with clinical trials prioritized for the higher risk patients who have a lower probability of success with ASCT.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Yi Miao (Department of Hematology, The First Affiliated Hospital of Nanjing Medical University, Jiangsu Province Hospital, Nanjing, China).
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.03.33). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 2002;346:235-42. [Crossref] [PubMed]
- Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 2016;127:2375-90. [Crossref] [PubMed]
- Savage KJ, Johnson NA, Ben-Neriah S, et al. MYC gene rearrangements are associated with a poor prognosis in diffuse large B-cell lymphoma patients treated with R-CHOP chemotherapy. Blood 2009;114:3533-37. [Crossref] [PubMed]
- Barrans S, Crouch S, Smith A, et al. Rearrangement of MYC is associated with poor prognosis in patients with diffuse large B-cell lymphoma treated in the era of rituximab. J Clin Oncol 2010;28:3360-5. [Crossref] [PubMed]
- Horn H, Ziepert M, Becher C, et al. MYC status in concert with BCL2 and BCL6 expression predicts outcome in diffuse large B-cell lymphoma. Blood 2013;121:2253-63. [Crossref] [PubMed]
- Copie-Bergman C, Cuilliere-Dartigues P, Baia M, et al. MYC-IG rearrangements are negative predictors of survival in DLBCL patients treated with immunochemotherapy: a GELA/LYSA study. Blood 2015;126:2466-74. [Crossref] [PubMed]
- Johnson NA, Savage KJ, Ludkovski O, et al. Lymphomas with concurrent BCL2 and MYC translocations: the critical factors associated with survival. Blood 2009;114:2273-9. [Crossref] [PubMed]
- Cohen JB, Geyer SM, Lozanski G, et al. Complete response to induction therapy in patients with Myc-positive and double-hit non-Hodgkin lymphoma is associated with prolonged progression-free survival. Cancer 2014;120:1677-85. [Crossref] [PubMed]
- Petrich AM, Gandhi M, Jovanovic B, et al. Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis. Blood 2014;124:2354-61. [Crossref] [PubMed]
- Kluk MJ, Chapuy B, Sinha P, et al. Immunohistochemical detection of MYC-driven diffuse large B-cell lymphomas. PLoS One 2012;7:e33813 [Crossref] [PubMed]
- Green TM, Young KH, Visco C, et al. Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol 2012;30:3460-7. [Crossref] [PubMed]
- Johnson NA, Slack GW, Savage KJ, et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol 2012;30:3452-9. [Crossref] [PubMed]
- Hu S, Xu-Monette ZY, Tzankov A, et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: a report from The International DLBCL Rituximab-CHOP Consortium Program. Blood 2013;121:4021-31; quiz 4250. [Crossref] [PubMed]
- Philip T, Guglielmi C, Hagenbeek A, et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin's lymphoma. N Engl J Med 1995;333:1540-5. [Crossref] [PubMed]
- Cuccuini W, Briere J, Mounier N, et al. MYC+ diffuse large B-cell lymphoma is not salvaged by classical R-ICE or R-DHAP followed by BEAM plus autologous stem cell transplantation. Blood 2012;119:4619-24. [Crossref] [PubMed]
- Herrera AF, Mei M, Low L, et al. Relapsed or Refractory Double-Expressor and Double-Hit Lymphomas Have Inferior Progression-Free Survival After Autologous Stem-Cell Transplantation. J Clin Oncol 2017;35:24-31. [Crossref] [PubMed]
- Dunleavy K, Fanale M, LaCasce A, et al. Preliminary Report of a Multicenter Prospective Phase II Study of DA-EPOCH-R in MYC-Rearranged Aggressive B-cell Lymphoma. The 2014 American Society of Hematology Annual Meeting. San Francisco, CA; December 5-8, 2014.
- Wilson WH, sin-Ho J, Pitcher BN, et al. Phase III Randomized Study of R-CHOP Versus DA-EPOCH-R and Molecular Analysis of Untreated Diffuse Large B-Cell Lymphoma: CALGB/Alliance 50303. 58th American Society of Hematology Annual Meeting; San Diego, CA, Dec. 3–6, 2016.
- Puvvada SD, Stiff PJ, Leblanc M, et al. Outcomes of MYC-associated lymphomas after R-CHOP with and without consolidative autologous stem cell transplant: subset analysis of randomized trial intergroup SWOG S9704. Br J Haematol 2016;174:686-91. [Crossref] [PubMed]
- Johnson-Farley N, Veliz J, Bhagavathi S, et al. ABT-199, a BH3 mimetic that specifically targets Bcl-2, enhances the antitumor activity of chemotherapy, bortezomib and JQ1 in "double hit" lymphoma cells. Leuk Lymphoma 2015;56:2146-52. [Crossref] [PubMed]
- Vandenberg CJ, Cory S. ABT-199, a new Bcl-2-specific BH3 mimetic, has in vivo efficacy against aggressive Myc-driven mouse lymphomas without provoking thrombocytopenia. Blood 2013;121:2285-8. [Crossref] [PubMed]
- Hogg SJ, Newbold A, Vervoort SJ, et al. BET Inhibition Induces Apoptosis in Aggressive B-Cell Lymphoma via Epigenetic Regulation of BCL-2 Family Members. Mol Cancer Ther 2016;15:2030-41. [Crossref] [PubMed]
- Neelapu SS, Locke FL, Bartlett NL, et al. Kte-C19 (anti-CD19 CAR T Cells) Induces Complete Remissions in Patients with Refractory Diffuse Large B-Cell Lymphoma (DLBCL): Results from the Pivotal Phase 2 ZUMA-1. American Society of Hematology Annual Meeting; San Diego, CA, 2016.


