
Lessons from the NOVA trial: an editorial on results, biomarkers, and patient selection for PARP inhibition in recurrent ovarian cancer
BRCA1 and BRCA2 are key proteins in the repair of double-strand DNA breaks via homologous recombination (HR) repair. Ovarian carcinomas (OC) with BRCA1 and BRCA2 (BRCA) mutations have HR deficiency (HRD) and are characterized by increased platinum sensitivity and response to poly [adenosine diphosphate (ADP)-ribose] polymerase (PARP) inhibitors, resulting in improved overall survival (1-5). PARP inhibitors generate synthetic lethality in BRCA-mutated carcinomas (6-9), but OC without BRCA mutations can also respond to PARP inhibitors, likely secondary to other sources of HRD (10-13). While up to half of high-grade serous ovarian carcinomas may have a defect in HR, we have found that most histologic subtypes of OC also have a proportion of cases with HRD (1,14). The most common cause of HRD in OC is germline and somatic BRCA mutations, found in approximately 15% and 6%, but mutations or epigenetic silencing of other HR repair genes also contribute (10,14,15). Because cancers with defective HR rely on more error-prone DNA repair such as non-homologous end-joining (NHEJ) or alternative end-joining (alt-EJ), HRD can result in characteristic DNA errors and structural alterations. Thus, a BRCA-like genomic signature may serve as a downstream marker of HRD (16-19). However, finding the best means to identify women without BRCA mutations who are most likely to benefit from PARP inhibitor therapy remains a diagnostic challenge and therapeutic need.
In The New England Journal of Medicine, Mirza and colleagues recently presented the results of the ENGOT-OV-16/NOVA clinical trial, a randomized, double-blind phase 3 trial to evaluate the efficacy of the PARP inhibitor niraparib as maintenance therapy following platinum chemotherapy in patients with platinum-sensitive, high-grade serous or BRCA-mutated recurrent OC (20). Patients were characterized according to presence or absence of a germline BRCA mutation, and OC without a germline BRCA mutation was defined as HRD or not through tumor testing using the myChoice® HRD test (Myriad Genetics, Salt Lake City, UT, USA). The primary endpoint was progression-free survival (PFS), with planned efficacy analysis in three groups: patients with germline BRCA mutations, patients without germline BRCA mutations, and the subgroup of non-germline BRCA patients with a “positive” myChoice HRD test. Participants receiving niraparib had a significantly longer median PFS than those in the placebo group in all three pre-specified groups: 21 vs. 5.5 months [hazard ratio (HR) 0.27; 95% confidence interval (CI): 0.17 to 0.41] in the germline BRCA mutation cohort, 9.3 months vs. 3.9 months (HR 0.45; 95% CI: 0.34 to 0.61) in the overall non-germline BRCA mutation cohort, and 12.9 vs. 3.8 months (HR 0.38; 95% CI: 0.24 to 0.59) in the HRD identified subgroup of the non-germline BRCA cohort.
These data support the efficacy of niraparib as maintenance therapy in women with recurrent, platinum-sensitive high-grade serous or BRCA-mutated OC, and add to the body of literature supporting the activity of PARP inhibitors in recurrent OC with or without BRCA mutations. The NOVA trial results are consistent with the data from study 19, which demonstrated the efficacy of the PARP inhibitor olaparib as maintenance therapy following platinum treatment in women with recurrent, platinum-sensitive high-grade serous OC (12,21). The NOVA trial and study 19 shared similar inclusion criteria, but their populations were not identical. Patients in the earlier study 19 had a median of 3 previous chemotherapy regimens, (versus 2 in NOVA), and study 19 had a lower fraction of patients with a complete response to platinum prior to randomization (45% vs. 51%). While cross-trial comparisons of absolute gains are invalid, the hazard ratios achieved by the PARP inhibitor arm, which in each trial was calculated by comparing two arms balanced for prognostic factors, was similar between the trials and, as expected, was most favorable for BRCA-mutated OC (Study 19: HR 0.18; 95% CI: 0.10–0.31 and NOVA HR 0.27; 95% CI: 0.17 to 0.41).
Niraparib was more effective than placebo in prolonging PFS in patients with platinum-sensitive, recurrent high-grade serous OC, regardless of the presence or absence of germline BRCA mutations or HRD status as determined by the myChoice® HRD test. In other words, in patients without germline BRCA mutations, use of the myChoice® HRD did not discriminate responders from non-responders. In NOVA, somatic BRCA mutations were included in the non-germline HRD group and certainly contributed to the favorable response to niraparib in the non-germline patients with OC. To explore the role of HRD testing amongst OC without somatic or germline BRCA mutations, the authors looked at outcomes in BRCA-wildtype OC with and without HRD. Again, even in BRCA-wildtype OC, this HRD test did not differentiate responders from non-responders; niraparib remained more effective than placebo in cases without germline or somatic BRCA mutations and no HRD, with a hazard ratio of 0.58 (95% CI: 0.36 to 0.92), or a 42% risk reduction in disease progression. Similarly, the BRCA-wildtype HRD subgroup had a 62% risk reduction in disease progression (HR 0.38; 95% CI: 0.24 to 0.59). Although it is possible that niraparib could provide greater benefit to those with BRCA-wildtype OC with HRD compared to those without HRD, this study was not powered to compare these groups, and the confidence intervals of the hazard ratios of these exploratory analyses overlap.
So why was the myChoice® HRD test not a successful predictive biomarker in NOVA? The authors state that “a negative myChoice HRD test was indicative of competent homologous recombination”, but it is important to remember that the MyChoice® HRD test as well as the loss of heterozygosity (LOH)-based HRD test by Foundation Medicine tested in the ARIEL clinical trials of the PARP inhibitor rucaparib (10) are not directly measuring homologous recombination capacity but rather a downstream phenotype (allelic imbalance) that is impacted by a number of factors beyond homologous recombination. Consequently, these HRD tests are an indirect and imperfect way to measure actual DNA repair capacity. The most common cause of platinum and PARP inhibitor resistance in a BRCA-mutated cancer cell is restoration of homologous recombination capacity (22-25). Yet these resistant and HR proficient cells retain the genomic “scar” of their previous HR deficiency and will be classified as HRD by myChoice® or other tests that rely on a genomic signature. Therefore, the HRD test classification imperfectly aligns with actual DNA repair capacity and is likely to become increasingly discordant as cancers acquire resistance during the course of multiple therapies.
In contrast to the NOVA trial findings, HRD status as defined by fraction of genomic LOH by Foundation Medicine was a successful biomarker in the ARIEL2 trial, and separated responders from non-responders to the PARP inhibitor rucaparib in patients with recurrent, platinum-sensitive high-grade OC (10). We suggest two potential explanations for the conflicting results between the two HRD tests. First, the HRD test used in each trial was different. The myChoice® HRD test by Myriad quantitates genomic instability of the tumor using three algorithms: LOH profiles, telomeric allelic imbalance, and large-scale transitions; HRD “status” is based on the sum of these 3 measurements, with a score of ≥42 called HRD. The ARIEL2 trial used the Foundation Medicine T5 next-generation sequencing assay (Foundation Medicine, Cambridge, MA, USA) to calculate the percentage of genomic LOH in tumor biopsy, with a pre-specified cut-off of ≥14% to define “LOH high” or HRD. Both of these tests generate a continuous variable but are used to bin cases into two groups. It is possible that the Foundation Medicine test is superior to the Myriad test in methodology or uses a better cut-off for binning HRD into two categories. However, only a direct head-to-head comparison of the biomarkers would justify that conclusion.
Probably, a more compelling argument explaining differences in the performance of the HRD biomarkers in the NOVA and ARIEL2 PARP inhibitor trials arises from differences in the trial designs and patient selection. Both trials included women with platinum-sensitive recurrent high-grade OC, but in the NOVA trial, participants had just completed platinum therapy and had to have a complete or near-complete response to therapy (with normalization of CA125 tumor marker) before randomization. In contrast, ARIEL2 patients had to have measurable disease amenable to biopsy and a greater than 6 month interval since last platinum therapy. Therefore, NOVA patients were selected for actual excellent platinum response proven at the time of starting PARP inhibitor while ARIEL2 patients had the likelihood of platinum responsiveness determined by interval since last treatment. Experience tells us that only about half of these patients would actually respond well to subsequent platinum. Therefore, the NOVA patients were more highly selected for real-time and repetitive platinum sensitivity. An HRD test might be a more discriminating predictive biomarker in a population expected to be more heterogeneous for treatment response, such as in ARIEL2. In NOVA, selection for “extreme” or proven platinum sensitivity may have been the most important predictor of PARP inhibitor response, and that selection may have eliminated the opportunity for the HRD biomarker to identify non-responders. ARIEL3 (NCT01968213) has a similar trial design to NOVA but uses the Foundation Medicine HRD test with a cut-off refined by the results in ARIEL2. The performance of the Foundation Medicine HRD test in ARIEL3 will provide some insight into the role of patient versus test selection in regards to PARP inhibitor response prediction.
Many questions remain unanswered about the role of PARP inhibitors in the treatment of ovarian cancer, and additional studies are underway to further clarify optimal timing and the role of predictive biomarkers. ARIEL3 will further test and refine predictors of PARP inhibitor response in BRCA-wildtype recurrent OC. Two phase 3 placebo-controlled trials will evaluate the role of PARP inhibitors in the first-line treatment and/or maintenance setting: GOG3005 (NCT04270585) is comparing standard carboplatin and paclitaxel to carboplatin and paclitaxel with concurrent and continuation maintenance therapy with the PARP inhibitor veliparib, and the SOLO-1 trial (NCT01844986) is evaluating olaparib maintenance monotherapy immediately following first-line platinum therapy in BRCA-mutated high-grade serous and endometrioid OC. Other novel applications of PARP inhibitors, such as in combination with other biologic agents (anti-angiogenic agents, immune checkpoint inhibitors, and agents in the PI3K/AKT, WEE-1 and ATR pathways) or use as a radiation sensitizer, are also underway.
Based on the NOVA trial study findings, the U.S. Food & Drug Administration (FDA) has granted Fast Track designation to niraparib, and is evaluating the drug for the maintenance treatment of patients with platinum-sensitive recurrent high-grade serous OC who have responded to platinum-based chemotherapy. Olaparib and rucaparib are already FDA-approved for monotherapy in the United States (Table 1). If approved, niraparib will be the third PARP inhibitor to become available for clinical use, and the first for maintenance therapy following response to chemotherapy. The results of the NOVA trial provide compelling data supporting the use of niraparib as a maintenance therapy in women with recurrent, platinum-sensitive high-grade serous or BRCA-mutated OC.
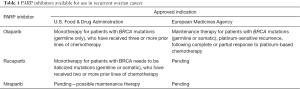
Full table
Acknowledgments
Funding: Stand Up To Cancer—Ovarian Cancer Research Fund Alliance—National Ovarian Cancer Coalition Dream Team Translational Research Grant (SU2C-AACR-DT16-15) (EMS, BN), V Foundation Translational Research Award (EMS) and U.S. Department of Defense Ovarian Cancer Research Program OC120506 (EMS). BN is supported by a Liz Tilberis Career Development Award from the Ovarian Cancer Research Fund Alliance.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Zheng Li (Department of Gynecologic Oncology, the Third Affiliated Hospital of Kunming Medical University (Yunnan Tumor Hospital), Kunming, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.03.60). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Norquist BM, Harrell MI, Brady MF, et al. Inherited Mutations in Women With Ovarian Carcinoma. JAMA Oncol 2016;2:482-90. [Crossref] [PubMed]
- Alsop K, Fereday S, Meldrum C, et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J Clin Oncol 2012;30:2654-63. [Crossref] [PubMed]
- Vencken PM, Kriege M, Hoogwerf D, et al. Chemosensitivity and outcome of BRCA1- and BRCA2-associated ovarian cancer patients after first-line chemotherapy compared with sporadic ovarian cancer patients. Ann Oncol 2011;22:1346-52. [Crossref] [PubMed]
- Yang D, Khan S, Sun Y, et al. Association of BRCA1 and BRCA2 mutations with survival, chemotherapy sensitivity, and gene mutator phenotype in patients with ovarian cancer. JAMA 2011;306:1557-65. [Crossref] [PubMed]
- Fong PC, Boss DS, Yap TA, et al. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med 2009;361:123-34. [Crossref] [PubMed]
- Bryant HE, Schultz N, Thomas HD, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 2005;434:913-7. [Crossref] [PubMed]
- Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 2005;434:917-21. [Crossref] [PubMed]
- Fong PC, Yap TA, Boss DS, et al. Poly(ADP)-ribose polymerase inhibition: frequent durable responses in BRCA carrier ovarian cancer correlating with platinum-free interval. J Clin Oncol 2010;28:2512-9. [Crossref] [PubMed]
- Kaufman B, Shapira-Frommer R, Schmutzler RK, et al. Olaparib monotherapy in patients with advanced cancer and a germline BRCA1/2 mutation. J Clin Oncol 2015;33:244-50. [Crossref] [PubMed]
- Swisher EM, Lin KK, Oza AM, et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trial. Lancet Oncol 2017;18:75-87. [Crossref] [PubMed]
- Gelmon KA, Tischkowitz M, Mackay H, et al. Olaparib in patients with recurrent high-grade serous or poorly differentiated ovarian carcinoma or triple-negative breast cancer: a phase 2, multicentre, open-label, non-randomised study. Lancet Oncol 2011;12:852-61. [Crossref] [PubMed]
- Ledermann J, Harter P, Gourley C, et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: a preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol 2014;15:852-61. [Crossref] [PubMed]
- McCabe N, Turner NC, Lord CJ, et al. Deficiency in the repair of DNA damage by homologous recombination and sensitivity to poly(ADP-ribose) polymerase inhibition. Cancer Res 2006;66:8109-15. [Crossref] [PubMed]
- Pennington KP, Walsh T, Harrell MI, et al. Germline and somatic mutations in homologous recombination genes predict platinum response and survival in ovarian, fallopian tube, and peritoneal carcinomas. Clin Cancer Res 2014;20:764-75. [Crossref] [PubMed]
- . Cancer Genome Atlas Research N. Integrated genomic analyses of ovarian carcinoma. Nature 2011;474:609-15. [Crossref] [PubMed]
- Abkevich V, Timms KM, Hennessy BT, et al. Patterns of genomic loss of heterozygosity predict homologous recombination repair defects in epithelial ovarian cancer. Br J Cancer 2012;107:1776-82. [Crossref] [PubMed]
- Wang ZC, Birkbak NJ, Culhane AC, et al. Profiles of genomic instability in high-grade serous ovarian cancer predict treatment outcome. Clin Cancer Res 2012;18:5806-15. [Crossref] [PubMed]
- Nik-Zainal S, Alexandrov LB, Wedge DC, et al. Mutational processes molding the genomes of 21 breast cancers. Cell 2012;149:979-93. [Crossref] [PubMed]
- Nik-Zainal S, Davies H, Staaf J, et al. Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature 2016;534:47-54. [Crossref] [PubMed]
- Mirza MR, Monk BJ, Herrstedt J, et al. Niraparib Maintenance Therapy in Platinum-Sensitive, Recurrent Ovarian Cancer. N Engl J Med 2016;375:2154-64. [Crossref] [PubMed]
- Ledermann JA, Harter P, Gourley C, et al. Overall survival in patients with platinum-sensitive recurrent serous ovarian cancer receiving olaparib maintenance monotherapy: an updated analysis from a randomised, placebo-controlled, double-blind, phase 2 trial. Lancet Oncol 2016;17:1579-89. [Crossref] [PubMed]
- Bouwman P, Jonkers J. Molecular pathways: how can BRCA-mutated tumors become resistant to PARP inhibitors? Clin Cancer Res 2014;20:540-7. [Crossref] [PubMed]
- Edwards SL, Brough R, Lord CJ, et al. Resistance to therapy caused by intragenic deletion in BRCA2. Nature 2008;451:1111-5. [Crossref] [PubMed]
- Norquist B, Wurz KA, Pennil CC, et al. Secondary somatic mutations restoring BRCA1/2 predict chemotherapy resistance in hereditary ovarian carcinomas. J Clin Oncol 2011;29:3008-15. [Crossref] [PubMed]
- Sakai W, Swisher EM, Karlan BY, et al. Secondary mutations as a mechanism of cisplatin resistance in BRCA2-mutated cancers. Nature 2008;451:1116-20. [Crossref] [PubMed]


