
Primary thyroid lymphoma: CT findings of a rare malignant tumor with pathologic correlations
Introduction
Primary thyroid lymphoma (PTL) is a rare malignant tumor, accounting for 5% of all thyroid malignancies (1,2). The annual incidence of PTL reported to be two cases per million (3). Despite its rarity, PTL should be promptly differentiated from other malignant lesions, because its management is quite different from other neoplasms of the thyroid gland (4-8). PTL was once considered a surgical disease, but the introduction of effective chemotherapeutic regimens has significantly changed the treatment paradigm (5). Current evidence suggests that combined chemoradiation therapy is effective in achieving disease control, and improving long term outcomes (4). Surgery might be performed in some cases when the diagnosis is unclear. Moreover, palliative surgery may be required to relieve pressure symptoms and airway obstruction, especially in patients who do not respond rapidly to non-surgical treatment (4).
Fine needle aspiration (FNA) is an excellent diagnostic tool for thyroid lesions because it is minimally invasive. However, results of FNA for the diagnosis of PTL are inconsistent, and its diagnostic accuracy rate varies from 25% to 90% (6,7). Cytologic results of FNA frequently reveal lymphocytes that are often erroneously diagnosed as thyroiditis. Therefore, in general, FNA is not often considered to be an adequate procedure for the diagnosis of thyroid lymphoma (8).
Ultrasound (US) is often the initial imaging study in patients with thyroid mass, because of its easy accessibility, low cost, noninvasiveness, and the capability of guiding the biopsy (8-17). However, PTL can present as a pseudo cystic hypoechoic region that can be mistaken for a benign cyst on US examination (11). Meanwhile, US examination has limitations when used to evaluate the extent of the lesion. PTL can extend to the deeper neck structure or the upper mediastinum, in such cases US is unable to depict tumors completely. Both CT and MRI demonstrate the extent of PTL well, and are useful to evaluate the invasion of adjacent structures by PTL. MRI has been shown to be more accurate than CT when evaluation the extent and staging of (12), but CT is more commonly used in the diagnosis and staging of PLT.
Due to the low prevalence of PTL, only a few studies describing the CT features of PTL have been published and mostly containing small series (12-16). The two largest series so far were reported by Takashima et al. and Li et al., with 16 and 27 cases respectively (15,16). Classical CT features of PTL, which contribute to the diagnosis, are described in those studies. In order to further understand imaging features of PTL (12-20), we studied the CT characteristics of 35 PTL cases.
Methods
The institutional review board of our hospitals approved this retrospective study, which through the PACS records, histopathology, pathologic gross records and operative notes in two tertiary hospitals dedicated for tumor diagnosis and treatment revealed 35 histopathologically confirmed cases of PTL from January 2002 to February 2012.
The clinical, surgical and pathological data were reviewed. This series was composed of 24 females (68.6%) and 11 males (31.4%), representing a female to male ratio of 2.2:1. The patients ranged in age from 23 to 84 years (median 65 years). Nine cases underwent FNA pre-operation. All cases underwent surgery, including total or partial thyroidectomy (n=26) and open biopsy (n=9). Histology and immunohistochemistry analysis were reviewed again by two pathologists, and the consensus was confirmed. Operative notes and pathologic gross records were reviewed in order to confirm the invasive extent of the tumor.
PTL was staged based on the Ann Arbor staging criteria (2). Stage I E (extranodal) is defined as the lymphoma limited to the confines of the thyroid gland, stage II E denotes the tumor spread beyond the thyroid to regional lymph nodes. Stage III E the tumor involves lymph nodes on both sides of the diaphragm, and stage IV E indicates systemic dissemination of the tumor. Because of the concern that stage III E or IV E tumors are most likely to involve the thyroid gland secondarily, we have only included patients diagnosed with Ann Arbor Stage I E and II E primary lymphoma involving the thyroid gland in this study.
All cases underwent preoperative CT, 22 out of 35 cases had both plain CT and contrast enhanced CT, in the remaining cases only the contrast enhanced CT was performed. CT was performed using a 16-slice scanner (Sensation, Siemens Medical solutions, Erlangen, Germany), or an 8-slice scanner (LightSpeed, General Electric Medical system, Milwaukee, USA). On the former scanner, images were acquired with 4 mm contiguous slices thickness (FOV =230×230, matrix =512×512). On the latter, images were obtained with 5 mm contiguous slices thickness (FOV =240×240, matrix =512×512). Routine scan coverage included the external auditory canal to the manubrium. If the tumor extended to the mediastinum, the scan coverage would be extended in order to cover the whole mass. For contrast-enhanced images, a bolus intravenous dose of 80 mL of non-ionic iodinated contrast agent (Ultravist, 300 mg I/mL) was given to all patients at the rate of 3 mL per second. The scan was initiated 45 seconds with the 16-slice scanner or 47 seconds with the 8-slice scanner after the onset of contrast injection. A delayed scan was not performed.
All images were reviewed in consensus by two radiologists (Lin Li and Lei Shi). The histopathological assessment was blinded to the radiologists. The patterns of the lesions were classified into two types based on CT findings as follows: type-1 PTL is the nodule type, the lesion is not bigger than 2 cm and surrounded by normal thyroid tissue. Type-1 PTL can be divided into two subtypes: type-1A, solitary nodule; type-1B, multiple individual nodules. Type-2 PTL presents one diffused lesion or multiple diffused lesions, which involve at least one lobe of the thyroid or even the whole thyroid. PTL were assessed in regards to enhancement attenuation, necrosis, calcification, and invasion of adjacent structures. The attenuation of the lesion on contrast-enhanced CT was recorded in relation to that of the sternocleidomastoid muscle (slightly low attenuation, iso-attenuation, or slightly high attenuation). The incidence rate of necrosis and calcification were recorded. Tumor necrosis was identified as the area of significantly lower attenuation than that of the skeletal muscle and solid part of the tumor after contrast enhancement. The cases with the irregular thickened wall of the trachea were diagnosed as invasion of the trachea. Invasion of the common carotid artery and the internal jugular vein was diagnosed if the tumor was in contact with one half or more of the circumference of these vessels, and if the fat plane between them was lost, or a filling defect appeared shown within the vessel. Invasion of the esophagus was diagnosed if the tumor was in contact with one half or more of the circumference of the esophagus, and the fat plane between them was lost (15). Invasion of the thyroid cartilage was diagnosed if the PTL was in contact with the thyroid cartilage and showed heterogeneous density with an irregular margin. The nodule or mass was diagnosed as the nodal lymphoma if the lesion is separate from PTL and showed similar density and enhancement feature with PTL. It was difficult to assess the lymph nodes in the retrospective research, because we couldn’t exactly compare the lymph node’s CT features with pathological findings one-by-one, therefore the lymph nodes were not assessed in this study.
For statistical analysis, the cases were divided into two groups. The group-1 tumors invaded adjacent structures. The group-1 tumors did not adjacent structures. Mann-Whitney U test was used to compare the mean size of tumors between two groups, with significant level being P value <0.05.
Results
Thirty one patients complained of a neck mass. Out of 31 cases, 21 cases presented with a rapidly enlarged neck mass that had been present for three weeks to three months. Tumor were found incidental healthy during examinations in four patients. Some symptoms were present due to compression of the neck organs. Fourteen cases (40%) had dyspnea, 17 cases had dysphagia (48.5%), two cases experienced with choking (n=2, 5.7%) and required a tracheotomy. Other symptoms included hoarseness (n=6, 17.1%), coughing (n=6, 17.1%) and hemoptysis (n=3, 8.6%).
In 29 cases, the exact diagnosis of PTL was not made prior to surgery. PTL was noted as one of differential diagnoses in six cases’ imaging reports. Out of 9 cases performed with FNA, 5 cases and 3 cases suggested the possibility of lymphoma and carcinoma respectively, and 1 case was diagnosed with a small-round cell malignant tumor.
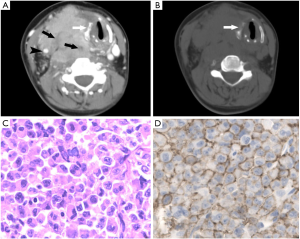
According to the histology and immunohistochemistry analysis, these cases were Non-Hodgkin lymphoma (NHL) of B-cell lineage. There were 31 cases of diffuse large B-cell lymphomas (DLBCL) and 4 cases of extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT). The lymphoma was staged as I E in 19 cases and as II E in 16 cases. The pathology results suggested Hashimoto’s thyroiditis existed in 23 patients (23/35, 65.7%).
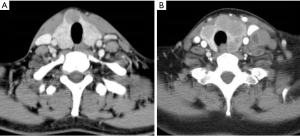
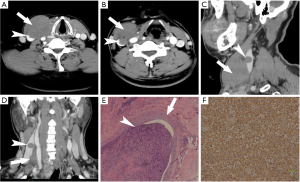
The clinical and CT characteristics of 35 PTL patients were summarized in Table 1. Two cases showed type-1A lesions (Figure 1A), 2 cases showed type-1B lesions (Figure 1B), and 31 cases showed type-2 lesions. Type-1 PTL presented as one or multiple nodules with well defined borders and a homogeneous density on non-contrast enhanced CT. Three tumors demonstrated iso-attenuation relative to the sternocleidomastoid muscle and one tumor showed slightly low attenuation on contrast enhanced CT. The type-1 lesion did not show calcification, necrosis or any invasive features. Type-2 PTL presented as diffused lesions, showed homogeneous density mass on non-contrast enhanced CT, and was enhanced moderately on contrast-enhanced CT. On contrast enhanced CT, the solid regions of tumor demonstrated slightly low attenuation relative to the sternocleidomastoid muscle in 3 cases, iso-attenuation in 23 cases, and slightly high attenuation in 5 cases. Calcification and necrosis were detected in 4 and 5 patients, respectively. All calcifications were single and small in size. The necrotic region showed irregular low density with a blurred boundary. In 4 cases, the necrotic region’s size was small in proportion to the overall tumor size. The remaining case of necrosis displayed an extensive low density region.
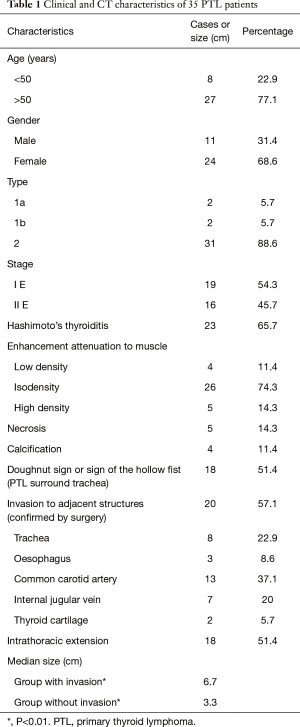
Full table
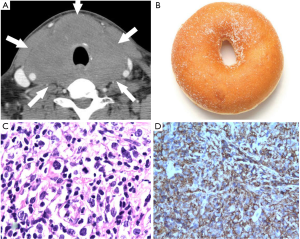
Based on CT features, type-2 PTL in this series tended to spread along the fat space to surround the adjacent organs. It tended to spread to the trachea esophagus groove, so the most common organ surrounded by PTL is the trachea (n=18), this pattern of spread accounted for 58.1% of type-2 cases and 51.4% of all cases respectively. When PTL completely surrounds the trachea, the feature can be described as the “doughnut sign” (Figure 2). When PTL partially surrounds trachea, the tumor looks like a hand that is holding the trachea. We suggest this feature can be called the “sign of the hollow fist” (Figure 3). The common carotid artery (n=13), Internal jugular vein (n=8), and esophagus (n=6) were also surrounded by the tumor. PTL involved the superior mediastinum in 18 cases (51.4%) on CT. The median size of cases with invasive signs is 6.7 cm, and that of the cases without invasive features 3.3 cm (P<0.01).
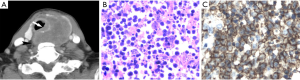
Out of 26 cases who underwent thyroidectomy, the features that suggest invasion were also confirmed in the surgical notes and pathologic records. In fourteen (53.8%) cases there was invasion of the surrounding organs. Five cases were diagnosed with invasion of the trachea, which showed an irregularly thickened wall of the trachea on CT (Figure 3). The common carotid artery and the internal jugular vein were invaded by PTL in 8 cases and 6 cases, respectively. In addition, other invasive signs were also confirmed. Tumor embolus in two cases was detected (Figure 4). The esophagus in two cases and the thyroid cartilage in two cases were destroyed by the tumor (Figure 5), and Intrathoracic extension of the thyroid tumor was detected in 12 patients.
Discussion
Previous studies have shown that autoimmune thyroiditis such as Hashimoto’ thyroiditis is associated with PTL (21,22). The relative risk of a patient with Hashimoto’ thyroiditis developing lymphoma has been estimated to be 40 to 80 times greater than that in the general population (23). Hashimoto’s thyroiditis is also common in our current study. Most of PTL are NHL of B-cell origin. DLBCL and MALT lymphoma are the most common subtypes of NHL. Follicular lymphoma is a very rare variant of PTL. In our current study, DLBCL is the most common subtypes, and only 4 cases are MALT lymphoma. DLBCL has the most aggressive clinical course, while MALT usually has a relatively benign biological behavior. Primary HL of the thyroid is exceedingly rare (24). No other subtypes of NHL were found in this series.
PTL occurs more commonly in women than men (23,24). In general, PTL typically presents clinically as a rapidly growing thyroid mass. The rate of thyroid enlargement tends to be more rapid in patients with PTL than in those with other thyroid malignancies except anaplastic thyroid carcinoma (ATC) (3,25). PTL may cause obstructive symptoms, such as dysphagia, dyspnea, and hoarseness (14,26). In our current study, the predominance of older age and female gender, and symptoms were similar to those found in previous studies (11,14,15,25). Meanwhile, in this series, our results confirmed the low diagnostic accuracy rate of FNA in PLT. We notice that FNA was unable to offer more information in other studies (7). Surgery was performed to provide a more precise diagnosis and/or relieve airways obstruction or as a curative resection. If the diagnostic accuracy rate of PLT was effectively improved, unnecessary surgery could be avoided.
In the previously published literature, PTL has been classified into three types (13,14,27). Type-1 refers singular nodular type, type-2 refers to multiple nodular type, type-3 refers to diffused mass. However, it has not been clearly documented where type-2 also include multiple nodular lesion merged together, while the merge of multiple nodular lesions would increase the possibility of encasing bronchus, and demonstrates biological behavior similar to type-3. We classify PTL into only two types. Type-1 refers to nodular PTL, being singular or multiple, they have similar clinical course, and do not demonstrate encasement or invasion of surrounding tissues. Type-2 refers to diffuse PTL; being due to singularly diffused mass, or due to a merge of multiple nodular PTL which would be classified type-2 according to previous literature (14). The new classification offers better explanation of the clinical presentations, and also contributing to differential diagnosis.
Besides the classic imaging feature of PTL, we also found some important features that were not reported or specifically mentioned in previous studies. Type-1 PTL present as a shows focal lesion. The tumor is usually iso- or low-attenuation relative to the sternocleidomastoid muscle, well defined, and mild enhanced on contrast enhanced CT. Because the lesion is smaller than 2 cm and surrounded by normal thyroid tissue, it cannot surround the adjacent organ, and doesn’t show aggressive features. Calcification and necrosis are not found. These features differ from medullary thyroid carcinoma and papillary thyroid carcinoma.
Type-2 PTL is the most common type in this series and shows diffuse lesions, which revealed mainly a homogeneous soft-tissue mass which was moderately enhanced on contrast CT. Calcification and necrosis are rare in this type. Type-2 PTL showed a higher probability of aggressive performance that has not been described in previous studies. The lesions tended to surround or invade the trachea and the trachea esophagus groove, we suggest it might be related to the anatomical structure of the thyroid gland. The thyroid gland is covered by two capsules (25). On the outside, the middle layer of deep cervical fascia not only covers the thyroid gland, but also covers the trachea and the esophagus in the same limited space. The fascia can limit the spread of PTL to a certain degree. Under the middle layer of deep cervical fascia, the thyroid has an inner true capsule, which is thin and adheres closely to the gland. The inner true capsule is a thin fibrous sheath, which is the only poor barrier between the thyroid gland and the trachea. When PTL breaks through the thyroid capsule, it can initially spread to the trachea and the tracheal esophagus groove with easy because there is no barrier between the thyroid capsule and the tracheal esophagus groove. This explains the high probability that the trachea and the esophagus may be invaded by PTL, and also explains the common clinical symptoms that occur, such as dysphagia, dyspnea, and hoarseness. We describe the feature when the trachea is surrounded by PTL as the “doughnut sign” and “the hollow fist sign”, which are the suggestive features of PTL. An Irregularly thickened tracheal wall is the characteristic feature of tracheal invasion.
Although the invasion of blood vessel has been reported in a previous imaging study of PTL (14), invasion of the blood vessel wall was more common in this series. In our study, PTL tend to encroach and surround the common carotid artery and the internal jugular vein. Furthermore, PTL was observed to break through the space formed by the middle lager of deep cervical fascia, especially if the tumor was larger or invasive. Moreover, our results suggest venous emboli of the internal jugular vein can be seen in PTL patients. When invaded by PTL, the common carotid artery did not display lumen deformation but only slight lumen narrowing. On the other hand, when invaded by PTL, the internal jugular vein showed severe lumen narrowing or occlusion, which might be due to the fact the wall of the common carotid artery is firmer and its intraluminal pressure is higher than that of the internal jugular vein. Venous emboli of the internal jugular vein in PTL patients were also observed in this series, this feature suggests invasion of the internal jugular vein (15). However, it can be difficult to diagnose emboli in the internal jugular vein in some cases because the attenuation of PTL is close to that of venous embolus. The invasion of thyroid cartilage was also detected in our study. This finding has not been reported in previous studies.
These features demonstrate that the ability of PTL for invade the trachea might have been underrated in previous studies. Previously PTL has been described as a non-invasive or poorly invasive tumor compared with thyroid carcinoma that shows invasive features (4). Our result help to further recognize the invasive characteristic of PTL on CT, and also suggest that it is unreliable to exclude PLT based on the invasive feature in the differential diagnosis between PTL and thyroid carcinoma.
The main differential diagnosis with PTL, especially type-2, based on CT features is ATC. The clinical features and CT attenuation of PTL are similar to ATC. The rate and characteristic of calcification or necrosis may help in the differential diagnosis between PTL and ATC. It has been reported that calcification and necrosis are usually present in patients with ATC (19). On the contrary, calcification and necrosis are rare in PTL (13,14). Although the rate of calcification in our study is higher than that in previous studies, there is the possibility that the calcification was due to Hashimoto’s thyroiditis which is often accompanied by calcification (26). Moreover, thyroid carcinoma lesions can show a large necrotic region with a clear wall on CT scan (17), but the necrotic region in PTL tends to be small in proportion to tumor size, irregular in shape, and with ill-defined margins as shown in our study. Similar CT findings have been reported in previous studies (13,14).
There were some limitations in this study. First, twelve cases didn’t have plain CT. Although PTL has been considered to be a homogeneous thyroidal mass with a low frequency of calcification (12,13), we could not rule out the possibility that the detection of calcification was underrated on contrast CT in this study. Second, since it was a retrospective study, the extent of lesion only could be confirmed by operative notes. Some invasive features described in the operative notes might not be as detailed as one would observe in a prospective study. Furthermore more advanced advantage techniques may allow for better tissue characterization (8,16,17,28-31).
In conclusion, PTL can present as two types based on CT feature. Type-1 appear as a nodule or multiple nodules with homogeneous isodensity to muscle, type-2 tend to be a mass with homogeneous isodensity to muscle, which is likely to appear invasive feature. CT imaging is able to provide important diagnostic and prognostic information for PTL clinical management.
Acknowledgments
Funding: This study was partially supported by Beijing Hope Run Special Fund (LC2008B62), a direct grant for research of The Chinese University of Hong Kong (2041501) and the Major Training Personnel from Zhejiang Provincial Program for the Training and Development Project for 151 talents (L Shi).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.03.84). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The institutional review board of our hospitals approved this retrospective study (IRB-2016-120). Informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Burke JS, Butler JJ, Fuller LM. Malignant lymphomas of the thyroid: a clinical pathologic study of 35 patients including ultrastructural observations. Cancer 1977;39:1587-602. [Crossref] [PubMed]
- Ansell SM, Grant CS, Habermann TM. Primary thyroid lymphoma. Semin Oncol 1999;26:316-23. [PubMed]
- Graff-Baker A, Roman SA, Thomas DC, et al. Prognosis of primary thyroid lymphoma: demographic, clinical, and pathologic predictors of survival in 1,408 cases. Surgery 2009;146:1105-15. [Crossref] [PubMed]
- Sakorafas GH, Kokkoris P, Farley DR. Primary thyroid lymphoma (correction of lympoma): diagnostic and therapeutic dilemmas. Surg Oncol 2010;19:e124-9. [Crossref] [PubMed]
- Graff-Baker A, Sosa JA, Roman SA. Primary thyroid lymphoma: a review of recent developments in diagnosis and histology-driven treatment. Curr Opin Oncol 2010;22:17-22. [Crossref] [PubMed]
- Sakorafas GH. What's the role of surgery in the management of primary thyroid lymphoma? Acta Oncol 2011;50:319-20. [Crossref] [PubMed]
- Hwang YC, Kim TY, Kim WB, et al. Clinical characteristics of primary thyroid lymphoma in Koreans. Endocr J 2009;56:399-405. [Crossref] [PubMed]
- Wang Y, Zhao H, Wang YX, et al. Improvement in the Detection of Cystic Metastatic Papillary Thyroid Carcinoma by Measurement of Thyroglobulin in Aspirated Fluid. Biomed Res Int 2016;2016:8905916.
- Wang Y, Li L, Wang YX, et al. Ultrasound findings of papillary thyroid microcarcinoma: a review of 113 consecutive cases with histopathologic correlation. Ultrasound Med Biol 2012;38:1681-8. [Crossref] [PubMed]
- Sun TQ, Zhu XL, Wang ZY, et al. Characteristics and prognosis of primary thyroid non-Hodgkin's lymphoma in Chinese patients. J Surg Oncol 2010;101:545-50. [Crossref] [PubMed]
- Kwak JY, Kim EK, Ko KH, et al. Primary thyroid lymphoma: role of ultrasound-guided needle biopsy. J Ultrasound Med 2007;26:1761-5. [Crossref] [PubMed]
- Takashima S, Nomura N, Noguchi Y, et al. Primary thyroid lymphoma: evaluation with US, CT, and MRI. J Comput Assist Tomogr 1995;19:282-8. [Crossref] [PubMed]
- Kim HC, Han MH, Kim KH, et al. Primary thyroid lymphoma: CT findings. Eur J Radiol 2003;46:233-9. [Crossref] [PubMed]
- Takashima S, Ikezoe J, Morimoto S, et al. Primary thyroid lymphoma: evaluation with CT. Radiology 1988;168:765-8. [Crossref] [PubMed]
- Takashima S, Morimoto S, Ikezoe J, et al. Primary thyroid lymphoma: comparison of CT and US assessment. Radiology 1989;171:439-43. [Crossref] [PubMed]
- Li XB, Ye ZX. Primary thyroid lymphoma: multi-slice computed tomography findings. Asian Pac J Cancer Prev 2015;16:1135-8. [Crossref] [PubMed]
- Wáng YX. Advance modern medicine with clinical case reports. Quant Imaging Med Surg 2014;4:439-43. [PubMed]
- Ha CS, Shadle KM, Medeiros LJ, et al. Localized non-Hodgkin lymphoma involving the thyroid gland. Cancer 2001;91:629-35. [Crossref] [PubMed]
- Takashima S, Morimoto S, Ikezoe J, et al. CT evaluation of anaplastic thyroid carcinoma. AJR Am J Roentgenol 1990;154:1079-85. [Crossref] [PubMed]
- Kossev P, Livolsi V. Lymphoid lesions of the thyroid: review in light of the revised European-American lymphoma classification and upcoming World Health Organization classification. Thyroid 1999;9:1273-80. [Crossref] [PubMed]
- Ceylan I, Yener S, Bayraktar F, et al. Roles of ultrasound and power Doppler ultrasound for diagnosis of Hashimoto thyroiditis in anti-thyroid marker-positive euthyroid subjects. Quant Imaging Med Surg 2014;4:232-8. [PubMed]
- Tam AA, Kaya C, Üçler R, et al. Correlation of normal thyroid ultrasonography with thyroid tests. Quant Imaging Med Surg 2015;5:569-74. [PubMed]
- Pedersen RK, Pedersen NT. Primary non-Hodgkin's lymphoma of the thyroid gland: a population based study. Histopathology 1996;28:25-32. [Crossref] [PubMed]
- Wang SA, Rahemtullah A, Faquin WC, et al. Hodgkin's lymphoma of the thyroid: a clinicopathologic study of five cases and review of the literature. Mod Pathol 2005;18:1577-84. [PubMed]
- Green LD, Mack L, Pasieka JL. Anaplastic thyroid cancer and primary thyroid lymphoma: a review of these rare thyroid malignancies. J Surg Oncol 2006;94:725-36. [Crossref] [PubMed]
- Ruggiero FP, Frauenhoffer E, Stack BC Jr. Thyroid lymphoma: a single institution's experience. Otolaryngol Head Neck Surg 2005;133:888-96. [Crossref] [PubMed]
- Standring S. Gray's anatomy: the anatomical basis of clinical practice (40th ed). London: Churchill Livingstone, 2008.
- Cai YF, Wang QX, Ni CJ, et al. The Clinical Relevance of Psammoma Body and Hashimoto Thyroiditis in Papillary Thyroid Carcinoma: A Large Case-control Study. Medicine (Baltimore) 2015;94:e1881 [Crossref] [PubMed]
- Yuan J, Chow SK, Yeung DK, et al. Quantitative evaluation of dual-flip-angle T1 mapping on DCE-MRI kinetic parameter estimation in head and neck. Quant Imaging Med Surg 2012;2:245-53. [PubMed]
- Yuan J, Lo G, King AD. Functional magnetic resonance imaging techniques and their development for radiation therapy planning and monitoring in the head and neck cancers. Quant Imaging Med Surg 2016;6:430-48. [Crossref] [PubMed]
- Cosgrove D, Barr R, Bojunga J, et al. WFUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography: Part 4. Thyroid. Ultrasound Med Biol 2017;43:4-26. [Crossref] [PubMed]


