
Direct-acting antiviral treatment for hepatitis C in liver transplant candidates and recipients
Recurrent hepatitis C virus (HCV) infection is universal in liver transplantation (LT) recipients, and the natural course of it is accelerated when compared to non-transplant patients with 15% to 30% of patients progressing to cirrhosis in 5 years from LT and a half of them developing liver failure shortly. The management of recurrent hepatitis C has been challenging in the ear of interferon-based therapies because of limited efficacy and poor tolerability. Consequently the patient and graft survival among HCV positive recipients was impaired by 10% when compared to other indications for LT (1). With the advent of potent and well-tolerated direct-acting antivirals (DAAs), the landscape of HCV treatment has dramatically changed (2). The sustained viral response (SVR) rates of LT recipients have been reported to be over 90%, and the outcome of LT for HCV positive recipients is expected to improve. What is more, DAAs have been shown to be equally effective even for cirrhotic patients who are waitlisted for LT, which poses a new problem; the waitlisted patients should be treated with DAAs during pre-LT period or post-LT period.
Ahmed et al. (3) performed the detailed pharmacoeconomics cost-effectiveness investigation regarding the use of all-oral-DAAs among HCV positive patients waitlisted for LT, pre-LT vs. post-LT. They constructed decision-analytic Markov models of the natural disease progression of hepatitis C in decompensated cirrhosis (DCC) and hepatocellular carcinoma (HCC) patients waitlisted for LT, and estimated their health and cost outcomes based on pre- vs. post-LT treatment with an all-oral DAA regimen calculating the per-patient quality-adjusted life years (QALYs) and the incremental cost-effectiveness ratio (ICER). Following the present excellent simulation, they concluded that pre-LT treatment with an all-oral DAA regimen provides the best health outcomes and is the most cost-effective strategy for the treatment of HCV patients with HCC or DCC waitlisted for LT.
Given the high efficacy and safety of all-oral DAA between pre-LT and post-LT patients, the treatment pretransplant versus posttransplant has become a matter of debate (4-7). Since the outcome of the post-LT treatment with DAA has already been proved to be excellent, concerns regarding the graft loss due to recurrent HCV, which had been the serious problem in the era of interferon, are diminishing. Consequently, the indication of pre-LT DAA treatment for the waitlisted candidates solely for the purpose of preventing HCV recurrence after LT is less compelling, and the decision to treat waitlisted patients should be oriented by the potential advantages versus disadvantages of achieving SVR among the pre-LT status. The major concern is so-called “model for end-stage liver disease (MELD) purgatory”, which describes that achieving SVR will lead to improvement in MELD score and clinical features of decompensation but not enough to avoid the need for LT, making the chance to get the liver graft less likely. In contrast to the accumulating reports of the post-LT DAA treatment, the data of pre-LT strategy for waitlisted candidates are scarce at present, which makes it difficult to guide who benefits and who is harmed by the pre-LT treatment, and future longitudinal studies comparing the pre- vs. post-LT DAA treatment are mandatory. In this aspect, the present work by Ahmed and colleagues seems informative for the indication of DAA for those awaiting LT.
The postulated benefits of pre-LT treatment and post-LT treatment were summarized in Table 1. The pre-LT treatment may improve liver function, survival on the waitlist, and the quality of life, which even includes the possibility of the obviating the need for LT. However, in general, the liver function improvement after the eradication of HCV by DAA will lead to some improvement in MELD score but not enough to obviate the necessity of LT, which will impose the elongated wait-time for candidates. In addition, the eradication of HCV will deprive the access to the HCV positive donors. The post-LT treatment will achieve the higher SVR rates than pre-LT with more available DAA treatment regimes in terms of liver and renal function. However, care should be taken for the drug-drug interactions (DDI) with immunosuppressants, which sometimes restricts the choice of DAA regimen. Another issue is the timing to start DAA treatment both for pre- and post-LT strategy.
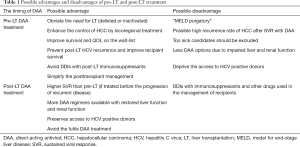
Full table
In the pre-LT strategy for the waitlisted patients, virological response after DAA therapy is very high in the order of 90% in those with compensated cirrhosis (Child-Pugh A) and high enough in the order of 80% even in those with DCC (Child-Pugh B-C). In terms of achieving SVR before LT, the duration of DAA treatment should be as short as possible. The prevention of HCV recurrence after LT is established if the SVR is achieved before LT, however, the HCV recurrence after LT among those on pre-LT DAA treatment at the time of LT seems to depend on the duration of HCV-RNA undetectability at the time of LT. So far the efficacy of DAA given pre-LT on the post-LT HCV recurrence was investigated in a single study by Curry et al. (8); 61 waitlisted patients with HCC and Child-Pugh A cirrhosis were treated with sofosbuvir and ribavirin and 43 had undergone LT with an HCV-RNA level less than 25 IU/mL at the time of LT. Overall, 70% of these 43 recipients were free from HCV recurrence post-LT, but among those who were HCV-RNA below quantitation levels for at least 30 days, 95% were free from HCV recurrence after LT. These results indicate that the achievement of SVR is not a mandatory end-point for all waitlisted patients with pre-LT treatment, but that HCV-RNA negative status for at least 1 month before LT seems to be a reliable virologic end-point if prevention of HCV recurrence is the main goal of pre-LT DAA.
Changes in liver function after DAA treatment for patients with DCC have been investigated in several landmark studies (9-14), which showed the possibility of decrease with a greater than 3 points in MELD score and 2 points in Child-Pugh score in 20% to 40% patients. The issue of delisting following the clinical improvement after per-LT DAA has been investigated in the European study (7,15), which suggest that DCC patients with a MELD score less than 20 on the waiting list should be considered for pre-LT DAA since around 20% of them can achieve enough improvement to be delisted. Despite these favorable results, in patients with high MELD scores (>20) and expected long waiting time, the risk of MELD purgatory should be balanced against the benefits of decreasing the risk of death on the list, when considering pre-LT DAA. For severe DCC patients with MELD score >25, pre-LT DAA treatment is not recommended since the possibility of death during the treatment, pre-LT, and post-LT is high with unknown probability of improvement. In contrast, patients with MELD <16 or Child Pugh B should be considered for pre-LT DAA, since they have a considerably high chance of being delisted (or inactivated). The waitlisted HCC patients with compensated cirrhosis may be the best candidate for the pre-LT DAA treatment because the majority of them have compensated cirrhosis and the time to LT is determined by wait-time rather than the severity of liver dysfunction. The pre-LT DAA for candidates with HCC should be indicated for those with a low-risk of post-LT HCC recurrence, no signs of HCC progression on the waiting list, and a waiting-time more than 3 months expected.
Studies with an all-oral DAA in post-LT have reported SVR rates of 84–100% with an excellent safety profile and a very low rate of treatment discontinuation (9,10,12,16-22). There are three issues to be considered when we plan the post-LT DAA: (I) the DDI with immunosuppressants, especially, calcineurin inhibitors (CNI), tacrolimus and cyclosporine; (II) the impaired renal function frequently encountered in post-LT recipients either due to postoperative complications or as a result of long-term exposure to calcineurin inhibitors, which limit the use of sofosbuvir; (III) the timing to start the post-LT DAA treatment. Sofosbuvir, a potent polymerase inhibitor, is the key DAA in post-LT recipients as with the case in non-transplant patients, and has a minimal interaction with CNI and other immunosuppressants. It requires dose adjustment or is contraindicated for those with estimated glomerular filtration rate (eGFR) less than 30 mL/min, which may be the major problem of post-LT DAA treatment, since the prevalence of the severe chronic kidney disease (eGFR <30 mL/min) is estimated to be 15–20%. DDIs of each DAA should be checked before starting the post-LT treatment in the association not only with immunosuppressants but with antifungal drugs, antibiotics, cardiovascular drugs, and central nervous system drugs. There are two different strategies regarding the post-LT DAA, preemptive therapy and clinically oriented treatment. The former mentions the very early or early initiation of DAA, before biochemical manifestations of HCV recurrence, and the latter means the later treatment initiated in response to biochemical or histopathological evidence of HCV recurrence as used to be done in the interferon era. Considering the viral kinetics after LT, preemptive approach may be an attractive option to manage HCV recurrence. However, currently no large data are available to recommend it on a routine basis. In the very early post-LT period, the optimal use of DAA may be hampered by the impaired graft liver function, impaired renal function, and DDIs. Accordingly, regarding the post-LT DAA treatment, the majority of patients in post-LT DAA treatment studies have been at least 6 months after LT before starting post-LT DAA. Given the efficacy and safety of DAAs, post-LT DAA treatment must be considered in any LT recipients as early as clinically feasible, irrespective of biochemical or histopathological evidence, to prevent the progression to cirrhosis and to maximize the SVR rates. The initiation of post-DAA therapy is recommended 3 to 6 months after LT (7).
Besides the clinical aspects of DAA treatment, the cost-effectiveness taking the long-term patient’s quality of life into account should also be considered in the discussion of pre-LT treatment vs. post-LT treatment, since the cost-effectiveness of the new drug is becoming important issue in the field of pharmacoeconomics. The present study is of note in this aspect, however we would like to address two important matters which should be further investigated in the future studies. The recent alert regarding the possible increased risk of HCC recurrence following resection, ablation or even LT among those undergoing DAA treatment (23,24) may complicate the indication of pre-LT DAA for waitlisted HCC patients. Since the data are conflicting at present, well-designed studies are warranted to address this issue, which could further be incorporated into the cost-effective analysis. Another important issue is the use of HCV-positive donors, which is not considered and is addressed as a limitation in this study. Considering that nearly 10% of donors were HCV positive among HCV positive recipients according to US registry, the pretransplant eradication of HCV depriving the access to HCV positive donor will certainly be disadvantageous for pre-LT DAA treated patients. Indeed, Salazar et al. (25) reported the conflicting results of the similar cost-effectiveness analysis very recently concluding that DAA treatment should be deferred until after LT taking into account the access to the expanded pool of HCV positive donors.
In conclusion, with all-oral DAA treatments, clinicians get the effective and safe therapeutic tools for the prevention and treatment of HCV both pre- and post-LT. Further longitudinal studies in the real-world cohorts will help the decision-making regarding the timing of DAA and the most cost-effective strategy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Xiu-Ping Zhang (Department of Hepatic Surgery VI, Eastern Hepatobiliary Surgery Hospital, Second Military Medical University, Shanghai, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.05.14). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Terrault NA, Berenguer M. Treating hepatitis C infection in liver transplant recipients. Liver Transpl 2006;12:1192-204. [Crossref] [PubMed]
- Chen T, Terrault NA. Perspectives on treating hepatitis C infection in the liver transplantation setting. Curr Opin Organ Transplant 2016;21:111-9. [Crossref] [PubMed]
- Ahmed A, Gonzalez SA, Cholankeril G, et al. Treatment of Patients Waitlisted for Liver Transplant with an All-Oral DAAs is a Cost-Effective Treatment Strategy in the United States. Hepatology 2017; [Epub ahead of print]. [Crossref] [PubMed]
- European Association for Study of Liver. EASL Recommendations on Treatment of Hepatitis C 2015. J Hepatol 2015;63:199-236. [Crossref] [PubMed]
- European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu. EASL Clinical Practice Guidelines: Liver transplantation. J Hepatol 2016;64:433-85. [Crossref] [PubMed]
- AASLD/IDSA HCV Guidance Panel. Hepatitis C guidance: AASLD-IDSA recommendations for testing, managing, and treating adults infected with hepatitis C virus. Hepatology 2015;62:932-54. [Crossref] [PubMed]
- Belli LS, Duvoux C, Berg T, et al. ELITA consensus statements on use of DAAs in liver transplant candidates and recipients. J Hepatol 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Curry MP, Forns X, Chung RT, et al. Sofosbuvir and ribavirin prevent recurrence of HCV infection after liver transplantation: an open-label study. Gastroenterology 2015;148:100-7.e101. [Crossref] [PubMed]
- Charlton M, Everson GT, Flamm SL, et al. Ledipasvir and Sofosbuvir Plus Ribavirin for Treatment of HCV Infection in Patients With Advanced Liver Disease. Gastroenterology 2015;149:649-59. [Crossref] [PubMed]
- Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis 2016;16:685-97. [Crossref] [PubMed]
- Foster GR, Irving WL, Cheung MC, et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol 2016;64:1224-31. [Crossref] [PubMed]
- Curry MP, O’Leary JG, Bzowej N, et al. Sofosbuvir and Velpatasvir for HCV in Patients with Decompensated Cirrhosis. N Engl J Med 2015;373:2618-28. [Crossref] [PubMed]
- Poordad F, Schiff ER, Vierling JM, et al. Daclatasvir with sofosbuvir and ribavirin for hepatitis C virus infection with advanced cirrhosis or post-liver transplantation recurrence. Hepatology 2016;63:1493-505. [Crossref] [PubMed]
- Saxena V, Nyberg L, Pauly M, et al. Safety and Efficacy of Simeprevir/Sofosbuvir in Hepatitis C-Infected Patients With Compensated and Decompensated Cirrhosis. Hepatology 2015;62:715-25. [Crossref] [PubMed]
- Belli LS, Berenguer M, Cortesi PA, et al. Delisting of liver transplant candidates with chronic hepatitis C after viral eradication: A European study. J Hepatol 2016;65:524-31. [Crossref] [PubMed]
- Charlton M, Gane E, Manns MP, et al. Sofosbuvir and ribavirin for treatment of compensated recurrent hepatitis C virus infection after liver transplantation. Gastroenterology 2015;148:108-17. [Crossref] [PubMed]
- Kwo PY, Mantry PS, Coakley E, et al. An interferon-free antiviral regimen for HCV after liver transplantation. N Engl J Med 2014;371:2375-82. [Crossref] [PubMed]
- Faisal N, Bilodeau M, Aljudaibi B, et al. Sofosbuvir-Based Antiviral Therapy Is Highly Effective In Recurrent Hepatitis C in Liver Transplant Recipients: Canadian Multicenter “Real-Life” Experience. Transplantation 2016;100:1059-65. [Crossref] [PubMed]
- Pungpapong S, Aqel B, Leise M, et al. Multicenter experience using simeprevir and sofosbuvir with or without ribavirin to treat hepatitis C genotype 1 after liver transplant. Hepatology 2015;61:1880-6. [Crossref] [PubMed]
- Forns X, Charlton M, Denning J, et al. Sofosbuvir compassionate use program for patients with severe recurrent hepatitis C after liver transplantation. Hepatology 2015;61:1485-94. [Crossref] [PubMed]
- Omichi K, Akamatsu N, Mori K, et al. Asunaprevir/daclatasvir and sofosbuvir/ledipasvir for recurrent hepatitis C following living donor liver transplantation. Hepatol Res 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Ciesek S, Proske V, Otto B, et al. Efficacy and safety of sofosbuvir/ledipasvir for the treatment of patients with hepatitis C virus re-infection after liver transplantation. Transpl Infect Dis 2016;18:326-32. [Crossref] [PubMed]
- Yang JD, Aqel BA, Pungpapong S, et al. Direct acting antiviral therapy and tumor recurrence after liver transplantation for hepatitis C-associated hepatocellular carcinoma. J Hepatol 2016;65:859-60. [Crossref] [PubMed]
- Reig M, Marino Z, Perello C, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol 2016;65:719-26. [Crossref] [PubMed]
- Salazar J, Saxena V, Kahn JG, et al. Cost-Effectiveness of Direct-Acting Antiviral Treatment in Hepatitis C-infected Liver Transplant Candidates with Compensated Cirrhosis and Hepatocellular Carcinoma. Transplantation 2017;101:1001-8. [Crossref] [PubMed]


