
Neutrophil to lymphocyte ratio but not ring enhancement could predict treatment response and new lesion occurrence in patients with hepatocellular carcinoma by drug eluting beads transarterial chemoembolization
Introduction
Hepatocellular carcinoma (HCC), mostly diagnosed in men and developed in low-income countries, is now the second leading cause of cancer deaths worldwide (1). Treatment options have been standardized by several guidelines, most of which state that for patients with intermediate HCC, who cannot be treated by potential curative treatments including resection and transplantation, transarterial chemoembolization (TACE) is a recommended therapy (2-4). Drug eluting beads transarterial chemoembolization (DEB-TACE) is an advanced type of TACE that delivers the chemotherapy drugs using microbeads, optimizing the efficiency of drug delivering and eliminating the systemic toxicity (5). Accumulating clinical trials and cohort studies have illuminated good efficacy and tolerance of DEB-TACE treatment for HCC patients. Nonetheless, prognostic factors are still demanded to fill the need in the management of HCC patients treated by DEB-TACE (6-8).
In imageology, ring enhancement that is discovered by contrast-enhanced computerized tomography (CT) or magnetic resonance image (MRI) could represent the existence of a tumor, liver abscess, neuromyelitis optica or atypical demyelination (9-12). In patients suspected of HCC, ring enhancements might indicate tumors or liver abscess, and the latter is a liver disease characterized by inflammation. However, whether ring enhancement is associated with inflammation of HCC patients or not is still obscure. Inflammatory responses require for the involvement of multiple inflammatory cells. Neutrophils and lymphocytes (LYM) are crucial in the immune responses to various stimuli, playing defensive roles in immune system, while, they can be inflammatory cells when attacked by virus or bacteria. Moreover, neutrophil to lymphocyte ratio (NLR) is indicated in multiple diseases as a marker for prognosis, for example, in patients with acute cerebral hemorrhage NLR could predict a neurological deterioration within 24 hours after the onset (13). While more importantly, NLR is well established as a marker for inflammation, which is also indicated in the pathology of cancers, and in several studies NLR is reported to be correlated with poor prognosis in various cancers (14-16). However, the prognostic role of NLR in HCC patients post DEB-TACE treatment remains to be unclear.
Therefore, this study aimed to investigate the association of ring enhancement with NLR, and to determinate the predicting values of ring enhancement and NLR for treatment response and occurrence of new lesions in patients with HCC post DEB-TACE treatment.
Methods
Patients
Sixty-five consecutive patients with HCC were enrolled at Department of Radiology, The First Affiliated Hospital, College of Medicine, Zhejiang University during 13th December, 2015 and 10th October, 2016. Inclusion criteria consisted of: (I) patients diagnosed as HCC confirming to the American Association for the Study of the Liver Diseases (AASLD) criteria (17); (II) age >18 years; (III) about to receive DEB-TACE treatment on-demand. And the exclusion criteria included: (I) patients with contraindications of DEB-TACE treatment or allergic to the chemoembolization drugs; (II) uncontrolled infection; (III) liver or renal failure; (IV) patients with other primary malignancies; (V) women in pregnancy or lactation period; (VI) history or presence of hepatic encephalopathy.
This study was conducted according to the basic principles of Declaration of Helsinki. Ethical approval (No. 2015447) was obtained from the Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University and all patients provided written informed consents.
Procedure of DEB-TACE
Each DEB-TACE procedure was conducted on-demand, which was determined by the multidisciplinary group in our hospital. CalliSpheres® beads (CB) were loaded with irinotecan (100 mg) or epirubicin (60 mg), the diameters of beads were between 100 and 300 µm. The beads were loaded as follows: firstly, chemoembolization reagents were mixed with water for injection and dissolved into solution at the concentration of 20 mg/mL, which was subsequently extracted by an injector; the solution was then mixed with CalliSpheres® beads by a tee joint and stored in a 20 mL injector; afterwards, the injector with mixed solution of chemoembolization reagents and CalliSpheres® beads was shaken every 5–10 minutes and was then stood at room temperature for 30 minutes. Lastly, non-ionic contrast agent was added in the mixed solution with the ratio of 1:1 and put for 5 minutes at room temperature.
Hepatic angiography was performed by computerized tomography (CT) for detection of tumor supplying vascular. Embolization of tumor supplying vascular was carried out using 2.4F microcatheter (Merit Maestro, Merit Medical System, Inc., Utah, USA), and the mixture of loaded CalliSpheres® beads and non-ionic contrast agent was injected at the speed of 1 mL/min. Afterwards, the embolization lasted until contrast agent flow stagnated. The second time of angiography was conducted to detect if there was remaining blushed nodules or not, after which the embolization will be performed until no more blushed tumor occurred. One bottle of blank microspheres (Merit Maestro, Merit Medical System, Inc., Utah, USA) with diameter ranged from 300 to 500 µm was used if one bottle of CalliSpheres® beads was emptied and the embolization point was still not reached.
Assessment
Clinical response after treatment was assessed by CT or MRI, following the modified Response Evaluation Criteria in Solid Tumors (mRECIST) criterion (18). A complete response (CR) was defined as the disappearance of any intratumoral arterial enhancement in all target nodules; partial response (PR) was at least a 30% decline in the sum of diameters of viable (enhancement in the arterial phase) target nodules, taking as reference the baseline sum of the diameters of target nodules; stable disease (SD) was any cases that do not qualify for either PR or progressive disease (PD) was an increase of at least 20% in the sum of the diameters of viable (enhancing) target nodules, taking as reference the smallest sum of the diameters of viable (enhancing) target nodules recorded since treatment initiated. In addition, the ORR was calculated as the percentage of the patients achieved CR and PR. Indexes related to liver function and renal function, as well as the tumor markers of laboratory examination were documented. All patients received contrast-enhanced MRI at 4 to 6 weeks post treatment to confirm the existence of ring enhancement. Gadopentetate dimeglumine (Magnevist; Schering, Berlin, Germany) was used as contrast agent in contrast-enhanced MRI, and iopromide (Ultravist, 300 mgI/mL, Bayer Healthcare, Berlin, Germany) was used in the contrast-enhanced CT in our study. In addition, the sequence utilized in the contrast-enhanced MRI was T1. The absolute neutrophil count (ANC) and LYM were examined through blood test within 24 hours post treatment, and the NLR was the ratio of ANC to LYM. The signal enhancement under MRI or the density strengthen under CT that presented as circle or ring-like shape on the photograms was defined as a ring enhancement. The occurrence of new lesions was assessed by MRI at last follow up of each patient. The median follow-up time was 201.0 days (range, 137.5–259.0 days), and the last follow up was on 10th December, 2016.
Statistical analysis
SPSS 22.0 software (IBM, USA) and Office 2016 software (Microsoft, USA) were utilized for statistical analysis. Data was presented as count, count (%), mean ± standard deviation or median (25th–75th). Comparison between two groups was determined by t-test, Chi-square test or Wilcoxon rank sum test. P<0.05 was considered significant.
Results
Participants
As presented in Table 1, there were 53 males and 12 females, among which the mean age in patients was 57.46±12.05 years. The number of patients with hepatitis B virus (HBV) and hepatitis C virus (HCV) were 51 (78.5%) and 3 (4.6%), respectively. In addition, 35 (53.8%) were with drink history and 52 (80.0%) patients had cirrhosis history. The tumor location was unilobar in 33 (50.8%) patients and bilobar in 32 (49.2%) patients, while the median value of largest nodule size was 5.50 cm (range, 3.75–9.90 cm). In terms of the stages of patients, the number of patients in Barcelona Clinic Liver Cancer (BCLC) stage A, B and C were 22 (33.8%), 21 (32.3%) and 22 (33.8%), respectively. And 64 patients (98.5%) were at Eastern Cooperative Oncology Group (ECOG) performance stage 0 while 1 patient (1.5%) was at stage 1. The other information on clinicopathological features, laboratory indexes and chemoembolization reagents were listed in Table 1.
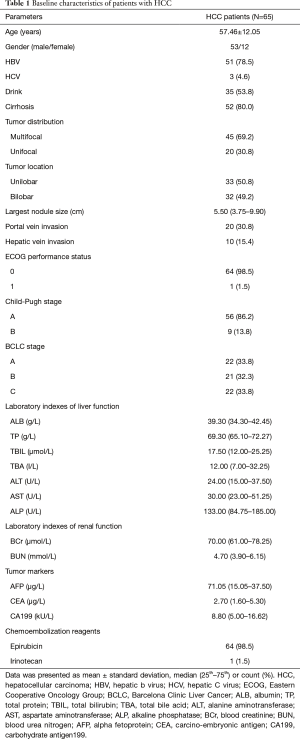
Full table
Treatment response of DEB-TACE
The CR and PR rates of patients were 18.5% and 69.2%, the ORR was 87.7% after DEB-TACE treatment (Figure 1A). In view of the treated nodules, 27.2% nodules achieved CR and 55.1% nodules achieved PR, the ORR was 82.3% (Figure 1B). Additionally, as shown in Figure 1C, among the 81 (55.1%) nodules reached PR, the percentage of nodules reached necrosis rate >80%, 50–80% and <50% were 54.3%, 37.0% and 8.6%, respectively.

Ring enhancement in patients with HCC
As listed in Table 2, at 4 to 6 weeks post treatment, ring enhancements were observed in 40 (62.0%) patients and the last 25 (38.0%) were not observed of ring enhancements.
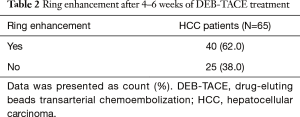
Full table
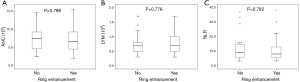
Correlation of ring enhancement with inflammation
Post treatment, ring enhancements were not correlated with ANC (P=0.798), LYM (P=0.776) or NLR (P=0.782) as exhibited in Figure 2A-C. The results indicated that the existence of ring enhancement was not associated with inflammation post treatment.
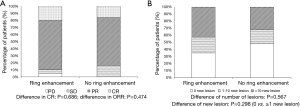
Correlations of ring enhancements with efficacy and new lesion occurrence
As displayed in Figure 3A, the CR (P=0.686) and ORR (P=0.474) of DEB-TACE treatments in patients with or without ring enhancements were similar. And as presented in Figure 3B, between patients with or without ring enhancements, no difference was found concerning the number of new lesions (P=0.567) or appearance of new lesions (P=0.298).
Associations of NLR with efficacy and new lesion occurrence
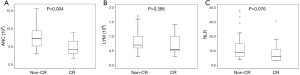
While Patients were divided into CR group and non-CR group, the ANC of patients in CR group was markedly lower than that of patients in non-CR group (P=0.004) (Figure 4A). However, no difference was found of LYM between patients in CR and non-CR groups (P=0.395) (Figure 4B). And there was a trend of a decrease in NLR of patients in CR group compared to that of patients in non-CR group (P=0.076) (Figure 4C). Whereas, no correlation of ANC (P=0.952), LYM (P=0.771) or NLR (P=0.873) with ORR was found (Figure 5A-C).

While as shown in Figure 6A,B, the ANC (P=0.804) and LYM (P=0.164) were not correlated with new lesion occurrence in patient. Moreover, the NLR was intended to be higher in patients presented with new lesion (P=0.094) (Figure 6C).

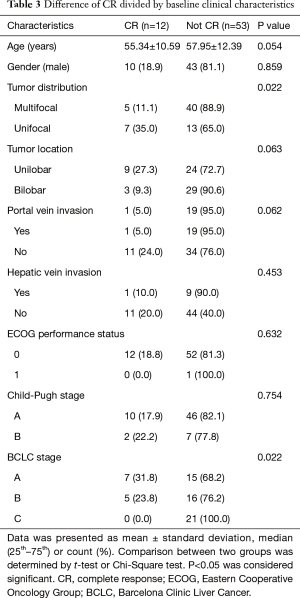
Subgroup analysis of factors at baseline for predicting CR
Patients were categorized by baseline characteristics to evaluate the influence of factors on CR achievement, as listed in Table 3, patients with multifocal disease disclosed decreased CR compared to patients with unifocal disease (P=0.022). Moreover, patients in higher BCLC stages had worse CR (P=0.022) as well.
Full table
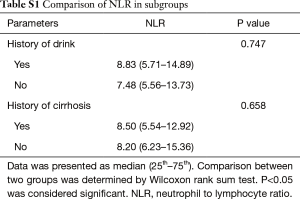
The difference of NLR between patients with or without drink history as well as in cirrhotic and non-cirrhotic patients
As listed in Table S1, the NLRs between patients with or without drink history were similar (P=0.747). In addition, there was no difference of NLR between patients with or without cirrhosis (P=0.658).
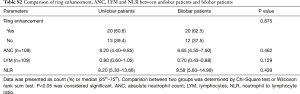
Differences regarding ring enhancement, ANC, LYM and NLR between patients with unilobar and bilobar diseases
The incidence of ring enhancement (P=0.875), ANC value (P=0.462), LYM value (P=0.129) and NLR value (P=0.439) were of no difference between patients with unilobar and bilobar diseases (Table S2).
Discussion
Over the last decade, management of HCC has been improved enormously by upgrading the supervision of high-risk population and optimizing treatment modalities. Furthermore, TACE techniques have been advanced over years, leading to the existence of DEB-TACE, which allows for a more sustained drug delivery and more constant drug concentration compared to conventional TACE (cTACE), which usually leads to more severe systemic toxicity in clinical practice (5). Most observational studies and meta-analysis illustrate superiority of DEB-TACE over cTACE regarding efficacy and tolerance, only a few studies report equivalence between DEB-TACE and cTACE (19-21). Even though the stratification for therapeutic choices has been well developed and staging systems are sound, for patients with HCC post DEB-TACE treatment, the attempts and evidence for the prognostic factors are still insufficient.
Emerging studies reveal that treatment response of DEB-TACE for HCC patients is relatively satisfactory, a prospective cohort study reports a CR rate of 36.8% and an overall response rate (ORR) of 60.0% in 57 patients with inoperable HCC treated with DEB-TACE (22). While in a retrospective cohort study with a smaller sample size, the CR rate was 42.4% and the ORR was 84.8% (23). And DEB-TACE is used as bridge therapy for patients with HCC undergoing transplantation in another retrospective cohort study, and a CR rate of 40.0% as well as an ORR of 73.0% were observed (24). The studies above revealed a relatively good efficacy of DEB-TACE, nonetheless, treatment response varies among studies, and compared to ours, the CR rates in previous studies are numerically higher but the ORR are similar. In our study, the CR rate was 18.5% and the ORR was 87.7%. The difference might result from: (I) the various patient eligibility among studies, a larger percentage of early HCC patients in the study cohort might contribute to a better treatment response; (II) the assorted sample sizes among studies.
Ring enhancement is a radiological feature that is decisive in diagnosing tumor or infection and is reported to be crucial in identifying stroke and pseudotumoral multiple sclerosis (25,26). For the identification of adenosquamous carcinoma of the pancreas (ASC), a study illuminates that ring enhancement on the contrast-enhanced CT is the most advantageous radiological feature (11). Apart from the diagnostic value, a prior study elucidates that ring enhancement is strongly associated with high 4-year recurrence rate and poor recurrence free survival of patients with oligodendroglial tumor, suggesting that ring enhancement might also have a prognostic value (27). For patients with HCC, ring enhancement is correlated with the increased density of peritumoral Kupffer cell, which is one type of macrophages situated in liver that playing defensive roles (28). Studies on the predictive value of ring enhancement for the efficacy of DEB-TACE are rare. One study evaluates the prognostic value of ring enhancement in a prospective historical cohort of HCC patients received DEB-TACE, and find no correlation of ring enhancement with treatment response (29). These evidences indicate that ring enhancement is critical in identifying neurological diseases and tumors, and is found to be associated with poor prognosis in certain tumors, however, no correlation of ring enhancement with treatment responses or survival in HCC patients treated by DEB-TACE has been reported until now. In consistent with the previous studies, we found no correlation of ring enhancement at 4 to 6 months post DEB-TACE with treatment response or new lesion occurrence in treated patients, which indicates that there might be no association of ring enhancement with prognosis. Meanwhile, ring enhancement was not correlated with ANC, LYM or NLR, either, which revealed that ring enhancement is not associated with inflammatory responses in HCC patients. Additionally, the three-dimensional response assessment tools, which are emerging assessment tools in recent years and might provide more vivid images and accurate results, were not used for the assessment of tumor response in our study. Future studies could introduce those tools to improve the treatment response evaluation.
Enormous effort has been made to explore the etiology of cancers, one of the most founded result illustrate that inflammation is one of the mechanisms that contribute to the malignant progressions (30,31). Leukocytes are involved in both immune and inflammatory responses, neutrophils belong to the large family of leukocytes and neutrophilia is a pathological progress that inhibits the immune system in various diseases (32,33). As another imperative type of leukocytes, LYM participate in the inflammatory responses of multiple types of tumors, producing inflammatory cytokines that promote malignant progression of tumors (34,35). Although LYM has not been considered as parameter for evaluating inflammation, due to its close correlation with inflammation, the potential of LYM becoming a parameter for inflammation is considerable. T LYM participate in the hypertensive inflammation, and it is reported that Connexin 43 in splenic LYM regulates CD4+CD25+ T LYM proliferation and cytokine production (36). In addition, as a part of the adaptive immune populations, T LYM are involved in mediating the pro-inflammatory atherogenic responses (37). In previous studies, the value of NLR for the prognosis of patients with HCC has been demonstrated by numerical studies. For HCC patients received radiotherapy, lower NLR pre treatment is associated with better PFS and OS post radiotherapy (38). In respect to the prognosis value of NLR in patients treated by TACE, there is still a large need in the investigations focused on this issue. A study assesses the prognostic value of NLR for non-viral HCC patients after TACE treatment and presents that patients with higher NLR at baseline have obviously poorer survival compared to those had lower NLR (39). Huang et al. also reports that for unresectable HCC patients, a higher NLR is an independent factor for a much worse OS post TACE treatment (40). While no previous study has reported the value of NLR in predicting prognosis of HCC patients treated by DEB-TACE. In order to evaluate the predicting value of NLR for the treatment responses, the ANC and LYM were assessed through blood tests within 24 h post DEB-TACE. In our study, we found that a decreased ANC post treatment was strongly correlated with a better CR, and that reduced NLR post treatment was likely to be associated with CR and no occurrence of new lesions as well. A higher NLR means higher neutrophil levels and lower LYM levels. Neutrophils are indicated in several tumors as prognostic factors. A previous retrospective study illustrates that elevated number of tumor-associated neutrophils is strongly correlated with poorer progression free survival (PFS) in uterine cervical cancer patients treated by radiotherapy (41). The prognostic effect of neutrophils might derive from its pathogenic role in tumors. Cedervall et al. reveals that circulating neutrophil extracellular traps (NET) increases in mice carrying tumors, leading to inflammation as well as vascular dysfunction (42). While LYM has an anti-tumor effect as reported by previous studies. In esophageal cancer and gastric cancers, the tumor-infiltrating T LYM interact with B LYM or plasma cells to function as anti-tumor cells (43). The mechanism of high NLR deteriorating the prognosis of patients with HCC is still not clear, but the results in our study might be derived from that: (I) the high NLR is correlated with more severe inflammation, which is also a promoter of tumor progression (30,31,38,44); (II) neutrophils and LYM are involved in the pathogenesis of tumors (41-43). Despite that there is only non-statistically significant trend of reduced CR rate and increase incidence of new lesions in HCC patients with higher NLR, the results still indicate NLR might play a role in the prognosis of patients treated by DEB-TACE, which could be a study direction in the future. In addition, the results may be influenced by the relatively low statistical power caused by the relatively small sample size.
A prior study reveals that HCC patients in higher BCLC stage illuminate poorer prognosis compared to patients in lower BCLC stage (45). And another study elucidates multifocal disease correlates with unfavorable survival in HCC patients treated by cTACE or DEB-TACE (46). In line with previous studies, in our study, the analysis of baseline characteristics for predicting the efficacy elucidated that patients with higher BCLC stage and multifocal lesions were of poorer CR.
Several limitations couldn’t be ignored in this present study: (I) 65 patients was a relatively small sample size, leading to a lack of statistical power and increase individual effect on the result; (II) the follow-up time in our study was short, and thus the long-term efficacy could not be assessed in our study; (III) only one patients at 1 or above ECOG performance status were enrolled, thus the results were relatively limited to ECOG 0 HCC patients. Therefore, further study including a larger sample size and longer follow-up period is needed.
In conclusion, NLR but not ring enhancement post treatment could predict the treatment response and new lesion occurrence in patients with HCC treated by DEB-TACE.
Full table
Full table
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.12.24). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All the participants signed the informed consents. This study was approved by the Ethics Committee of The First Affiliated Hospital, College of Medicine, Zhejiang University (2015447).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Granito A, Bolondi L. Non-transplant therapies for patients with hepatocellular carcinoma and Child-Pugh-Turcotte class B cirrhosis. Lancet Oncol 2017;18:e101-12. [Crossref] [PubMed]
- Facciorusso A, Licinio R, Muscatiello N, et al. Transarterial chemoembolization: Evidences from the literature and applications in hepatocellular carcinoma patients. World J Hepatol 2015;7:2009-19. [Crossref] [PubMed]
- Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 1999;19:329-38. [Crossref] [PubMed]
- Imai N, Ishigami M, Ishizu Y, et al. Transarterial chemoembolization for hepatocellular carcinoma: A review of techniques. World J Hepatol 2014;6:844-50. [Crossref] [PubMed]
- Rostas J, Tam A, Sato T, et al. Image-Guided Transarterial Chemoembolization With Drug-Eluting Beads Loaded with Doxorubicin (DEBDOX) for Unresectable Hepatic Metastases from Melanoma: Technique and Outcomes. Cardiovasc Intervent Radiol 2017;40:1392-400. [Crossref] [PubMed]
- Rahman FA, Naidu J, Ngiu CS, et al. Conventional versus Doxorubicin-Eluting Beads Transarterial Chemoembolization for Unresectable Hepatocellular Carcinoma: a Tertiary Medical Centre Experience in Malaysia. Asian Pac J Cancer Prev 2016;17:4037-41. [PubMed]
- Arabi M, BenMousa A, Bzeizi K, et al. Doxorubicin-loaded drug-eluting beads versus conventional transarterial chemoembolization for nonresectable hepatocellular carcinoma. Saudi J Gastroenterol 2015;21:175-80. [Crossref] [PubMed]
- Fujiwara Y, Shiba H, Nakabayashi Y, et al. Hepatic abscess in the Spiegel lobe caused by foreign body penetration: report of a case report. Surg Case Rep 2017;3:24. [Crossref] [PubMed]
- Yokote H, Nose Y, Ishibashi S, et al. Spinal cord ring enhancement in patients with neuromyelitis optica. Acta Neurol Scand 2015;132:37-41. [Crossref] [PubMed]
- Imaoka H, Shimizu Y, Mizuno N, et al. Ring-enhancement pattern on contrast-enhanced CT predicts adenosquamous carcinoma of the pancreas: a matched case-control study. Pancreatology 2014;14:221-6. [Crossref] [PubMed]
- Javalkar V, Manix M, Wilson J, et al. Open ring enhancement in atypical brain demyelination. J Clin Neurosci 2012;19:910-2. [Crossref] [PubMed]
- Lattanzi S, Cagnetti C, Provinciali L, et al. Neutrophil-to-lymphocyte ratio and neurological deterioration following acute cerebral hemorrhage. Oncotarget 2017;8:57489-94. [Crossref] [PubMed]
- Templeton AJ, McNamara MG, Seruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst 2014;106:dju124 [Crossref] [PubMed]
- Pedrazzani C, Mantovani G, Fernandes E, et al. Assessment of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and platelet count as predictors of long-term outcome after R0 resection for colorectal cancer. Sci Rep 2017;7:1494. [Crossref] [PubMed]
- Bowen RC, Little NAB, Harmer JR, et al. Neutrophil-to-lymphocyte ratio as prognostic indicator in gastrointestinal cancers: a systematic review and meta-analysis. Oncotarget 2017;8:32171-89. [Crossref] [PubMed]
- Lammer J, Malagari K, Vogl T, et al. Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION V study. Cardiovasc Intervent Radiol 2010;33:41-52. [Crossref] [PubMed]
- Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 2010;30:52-60. [Crossref] [PubMed]
- Facciorusso A, Di Maso M, Muscatiello N. Drug-eluting beads versus conventional chemoembolization for the treatment of unresectable hepatocellular carcinoma: A meta-analysis. Dig Liver Dis 2016;48:571-7. [Crossref] [PubMed]
- Huang K, Zhou Q, Wang R, et al. Doxorubicin-eluting beads versus conventional transarterial chemoembolization for the treatment of hepatocellular carcinoma. J Gastroenterol Hepatol 2014;29:920-5. [Crossref] [PubMed]
- Xie ZB, Wang XB, Peng YC, et al. Systematic review comparing the safety and efficacy of conventional and drug-eluting bead transarterial chemoembolization for inoperable hepatocellular carcinoma. Hepatol Res 2015;45:190-200. [Crossref] [PubMed]
- Kokabi N, Ludwig JM, Camacho JC, et al. Baseline and Early MR Apparent Diffusion Coefficient Quantification as a Predictor of Response of Unresectable Hepatocellular Carcinoma to Doxorubicin Drug-Eluting Bead Chemoembolization. J Vasc Interv Radiol 2015;26:1777-86. [Crossref] [PubMed]
- Reis SP, Sutphin PD, Singal AG, et al. Tumor Enhancement and Heterogeneity Are Associated With Treatment Response to Drug-Eluting Bead Chemoembolization for Hepatocellular Carcinoma. J Comput Assist Tomogr 2017;41:289-93. [Crossref] [PubMed]
- Yu CY, Ou HY, Weng CC, et al. Drug-Eluting Bead Transarterial Chemoembolization as Bridge Therapy for Hepatocellular Carcinoma Before Living-Donor Liver Transplantation. Transplant Proc 2016;48:1045-8. [Crossref] [PubMed]
- de Medeiros FC, de Albuquerque LA, Pittella JE, et al. Open-ring enhancement in pseudotumoral multiple sclerosis: important radiological aspect. Case Rep Neurol Med 2014;2014:951690 [Crossref] [PubMed]
- Wong AA, Henderson RD, O'Sullivan JD, et al. Ring enhancement after hemorrhagic stroke. Arch Neurol 2004;61:1790. [Crossref] [PubMed]
- Choi KY, Jung TY, Jung S, et al. Prognosis of oligodendroglial tumor with ring enhancement showing central necrotic portion. J Neurooncol 2011;103:103-10. [Crossref] [PubMed]
- Tanimoto A, Wakabayashi G, Shinmoto H, et al. The mechanism of ring enhancement in hepatocellular carcinoma on superparamagnetic iron oxide-enhanced T1-weighted images: an investigation into peritumoral Kupffer cells. J Magn Reson Imaging 2005;21:230-6. [Crossref] [PubMed]
- Vesselle G, Quirier-Leleu C, Velasco S, et al. Predictive factors for complete response of chemoembolization with drug-eluting beads (DEB-TACE) for hepatocellular carcinoma. Eur Radiol 2016;26:1640-8. [Crossref] [PubMed]
- Pollard J. Bacteria, inflammation and cancer. Nat Rev Immunol 2015;15:528. [Crossref] [PubMed]
- Coffelt SB, de Visser KE. Cancer: Inflammation lights the way to metastasis. Nature 2014;507:48-9. [Crossref] [PubMed]
- Roos AB, Sethi S, Nikota J, et al. IL-17A and the Promotion of Neutrophilia in Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 2015;192:428-37. [Crossref] [PubMed]
- Schernberg A, Moureau-Zabotto L, Rivin Del Campo E, et al. Leukocytosis and neutrophilia predict outcome in locally advanced esophageal cancer treated with definitive chemoradiation. Oncotarget 2017;8:11579-88. [Crossref] [PubMed]
- Denkert C, Loibl S, Noske A, et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol 2010;28:105-13. [Crossref] [PubMed]
- Buisseret L, Garaud S, de Wind A, et al. Tumor-infiltrating lymphocyte composition, organization and PD-1/ PD-L1 expression are linked in breast cancer. Oncoimmunology 2016;6:e1257452 [Crossref] [PubMed]
- Zhang HC, Zhang ZS, Zhang L, et al. Connexin 43 in splenic lymphocytes is involved in the regulation of CD4+CD25+ T lymphocyte proliferation and cytokine production in hypertensive inflammation. Int J Mol Med 2018;41:13-24. [PubMed]
- Hansson GK, Holm J, Jonasson L. Detection of activated T lymphocytes in the human atherosclerotic plaque. Am J Pathol 1989;135:169-75. [PubMed]
- Son SH, Park EY, Park HH, et al. Pre-radiotherapy neutrophil-to-lymphocyte ratio as an independent prognostic factor in patients with locally advanced hepatocellular carcinoma treated with radiotherapy. Oncotarget 2017;8:16964-71. [Crossref] [PubMed]
- Zhang J, Gong F, Li L, et al. Diabetes mellitus and the neutrophil to lymphocyte ratio predict overall survival in non-viral hepatocellular carcinoma treated with transarterial chemoembolization. Oncol Lett 2014;7:1704-10. [Crossref] [PubMed]
- Huang ZL, Luo J, Chen MS, et al. Blood neutrophil-to-lymphocyte ratio predicts survival in patients with unresectable hepatocellular carcinoma undergoing transarterial chemoembolization. J Vasc Interv Radiol 2011;22:702-9. [Crossref] [PubMed]
- Matsumoto Y, Mabuchi S, Kozasa K, et al. The significance of tumor-associated neutrophil density in uterine cervical cancer treated with definitive radiotherapy. Gynecol Oncol 2017;145:469-75. [Crossref] [PubMed]
- Cedervall J, Dimberg A, Olsson AK. Tumor-induced neutrophil extracellular traps-drivers of systemic inflammation and vascular dysfunction. Oncoimmunology 2015;5:e1098803 [Crossref] [PubMed]
- Svensson MC, Warfvinge CF, Fristedt R, et al. The integrative clinical impact of tumor-infiltrating T lymphocytes and NK cells in relation to B lymphocyte and plasma cell density in esophageal and gastric adenocarcinoma. Oncotarget 2017;8:72108-26. [Crossref] [PubMed]
- Viers BR, Boorjian SA, Frank I, et al. Pretreatment neutrophil-to-lymphocyte ratio is associated with advanced pathologic tumor stage and increased cancer-specific mortality among patients with urothelial carcinoma of the bladder undergoing radical cystectomy. Eur Urol 2014;66:1157-64. [Crossref] [PubMed]
- Kao WY, Chao Y, Chang CC, et al. Prognosis of Early-Stage Hepatocellular Carcinoma: The Clinical Implications of Substages of Barcelona Clinic Liver Cancer System Based on a Cohort of 1265 Patients. Medicine (Baltimore) 2015;94:e1929 [Crossref] [PubMed]
- Golfieri R, Giampalma E, Renzulli M, et al. Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer 2014;111:255-64. [Crossref] [PubMed]


