
Prevalence and prognostic impact of synchronous distant metastases in patients with oral tongue squamous cell carcinoma: a SEER-based study
Introduction
Oral carcinomas are the sixth most common cancers in the world, after cancers of the lung, breast, colorectal, prostate and gastric (1). Oral tongue squamous cell carcinoma (OTSCC) is the most common type of the oral cancer, accounting for about 40% of the cases (2), most of which occurs on the lateral border and ventral surface (3).
Treatment algorithms for OTSCC have been based on a multitude of factors including tumor characteristics (histology, biology and stage) and patient characteristics (co-morbidity and performance status). For medically operable non metastatic patients, surgical resection is the mainstay of treatment. More recently, a positive role for adjuvant systemic therapy has also been shown (4). For advanced/unresectable disease, the primary treatment is radiotherapy (RT). Despite evolution in management, the overall survival (OS) of patients has not improved significantly during the past 20 years, especially those with distant metastases (5).
Site and burden of distant metastatic disease are interesting, easy to assess clinical markers that can help triage patients into good and poor prognosis categories. Moreover, specific clinical patterns of distant metastasis can be linked to some baseline epidemiological and clinical factors as well as biologic and molecular factors. Population based databases can be utilized to answer many of the above questions. As far as we know, studies describing the clinical correlates and prognostic value of distant metastases in OTSCC systematically are few and we sought to explore prevalence and prognostic impact of synchronous distant metastases among patients with OTSCC in this study.
Methods
Ethical approval and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of Fudan University Shanghai Cancer Center Ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The experimental protocols were also approved by Fudan University Shanghai Cancer Center Ethics committee (reference number 1 410 140-8). Written informed consent was obtained from all individual participants included in the study.
Cohort population
The SEER program is the largest publicly available cancer dataset, which contains data on patient demographics, tumor characteristics, first course of treatment, and follow-up information (6). However, SEER does not currently include any information on location of metastases in the standard research data until 2010. Using this dataset, data from non-selected histologically proven OTSCC patients between 2010 and 2014 were collected and 439 patients with ‘blanks’ metastatic site were excluded. A total of 5,730 OTSCC patients were included.
Statistical analysis
The patients’ demographic and tumor characteristics were summarized with descriptive statistics. We examined the relationship between these factors and distant metastases using Chi-squared tests.
Survival was defined as the number of months between the date of diagnosis and the date of death of any causes (OS) or of their cancer (CSS). For analysis of OS, the time from diagnosis until the end of the follow-up was used together with the information whether a patient died or not. For cancer-specific survival (CSS), CSS was calculated from the date of diagnosis to the date of cancer specific death whereas other deaths unrelated to OTSCC were censored. The censoring was based on the coding of these endpoints in the SEER database (alive, cancer-associated death, other death). We evaluated the association between survival and different variables using the methods of Kaplan-Meier. Univariate analysis was performed using the log-rank test. Multivariate analyses with the Cox proportional hazards model were used to test the independent significance of the predictors.
Two-sided P value <0.05 was considered statistically significant and confidence intervals (CIs) were set as 95%. All of statistical analyses were performed using SPSS 19.0 (SPSS, Chicago, IL, USA).
Results
Clinical characteristics of all patients
Among the 5,730 patients, there were 3,366 males (58.7%) and 2,364 females (41.3%). Median age was 62, with a range of 12–102. About 25.7% tumors were well differentiated (grade 1), while 56.1% were moderately differentiated (grade 2) and 18.2% were poorly differentiated or undifferentiated (grade 3). According to the 7th edition of UICC/AJCC Staging System, 2,895 patients (50.5%) were T1, 1,650 patients (28.8%) were T2, 612 patients (10.7%) were T3, and 573 patients (10.0%) were T4. With regard to N classifications, 3,841 patients (67.0%) were N0, 763 patients (13.3%) were N1, 1,081 patients (18.9%) were N2, and 45 patients (0.8%) were N3. Patients’ characteristics are listed in Table 1.
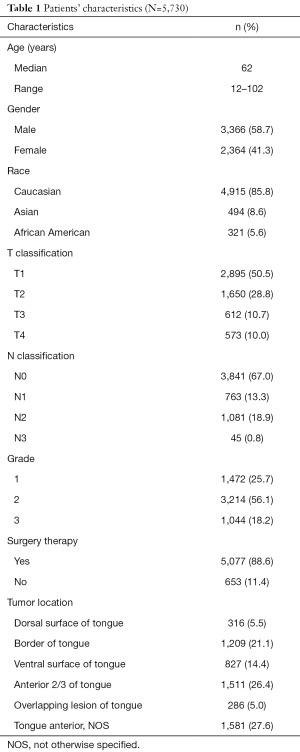
Full table
Metastasis pattern
The database only had metastatic information related to liver, lung, bone and brain metastasis. In the patients of all-stage OTSCC, the most frequent site of synchronous distant metastases at initial diagnosis was lung (n=32), followed by bone (n=16). There is no liver or brain metastasis.
As shown in Table 2, histological grade of tumor was found to be independently associated with lung and bone metastases (P=0.048 and P<0.001, respectively). Poorer differentiation was an independent prognostic parameter for higher incidence of metastasis. In addition, we found that T classification was also an independent parameter for metastatic diseases. A higher T category was associated with higher incidence of metastasis (P<0.001). The same results were found in N category (P<0.001).

Full table
What’s more, lung metastatic diseases were associated with younger age and male gender (P=0.009 and P=0.010, respectively).
Survival
The median follow-up time was 17.0 months, with a range from 0 to 59 months. For patients alive at the end of follow-up, the median follow-up time was 24.0 months, with a range from 0 to 59 months. The survival differences associated with distant metastatic sites were illustrated by Figure 1. Since the time of follow-up is short in current study, we only estimated the 1-year OS and CSS for patients with different metastases. The 1-year OS was 26.7% and 7.3% for patients with lung and bone metastasis, respectively. The 1-year CSS was 44.3% and 0 for patients with lung and bone metastasis, respectively. There was significant difference in OS and CSS between lung and bone metastases (P<0.001).
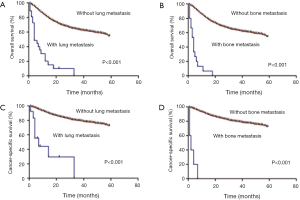
CSS was evaluated according to whether or not surgical treatment to the primary tumor was performed among different categories of patients. There was evidence of benefit for patients with lung metastases (P<0.001) and for patients with bone metastases (P<0.001) (figures not shown).
On univariate analysis, age, race, gender, tumor location, histological grade, T classification, N classification, distant metastases and surgery therapies to the primary tumor could influence OS and CSS among patients with OTSCC (P<0.001) (Table 3).
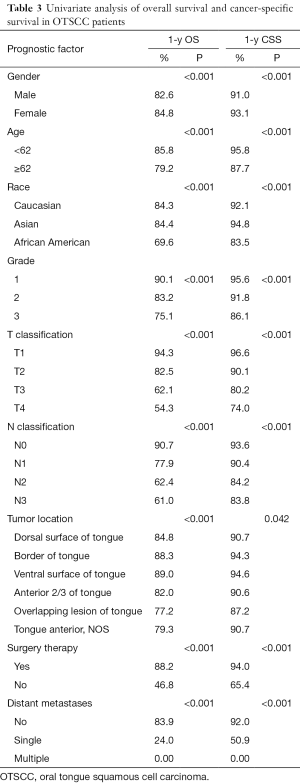
Full table
Multivariate models controlling for different variables demonstrated that age, histological grade, T classification, N classification, number of metastatic sites and therapies to the primary tumor were independent prognostic factors of OS and CSS (Table 4). Elderly patients with higher T category, higher N category, multiple sites of metastases and no surgery therapies to the primary tumor were more likely to reduce life expectancy.
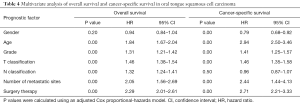
Full table
In our study, 5-year OS are 58.7% and 38.1% for localized and regional OTSCC patients, respectively, which are much higher than metastatic OTSCC patients (20.6%). The same results were found in CSS (Figure 2).

Discussion
The current analysis has pointed out some interesting correlations between some baseline criteria and the patterns of distant metastases. For example, lung metastatic diseases were associated with younger age and male gender and maybe the lifestyles (smoking and alcohol drinking) could partly explain the observed sex-based differences. Higher T categories are observed in patients presenting with M+ disease as opposed to M0. For N Classification, Ebrahimi (7) analysed the data of 3,704 patients with oral cancer undergoing surgery with curative intent. The median number of metastatic lymph nodes was significantly higher in patients with N2c disease compared to those with N2b disease (P<0.001). In multivariable analyses stratified by study center, the addition of the number of metastatic lymph nodes improved model fit beyond existing N classification. Next, the authors confirmed significant heterogeneity in prognosis based on the number of metastatic lymph nodes (≤2, 3–4, and ≥5) in patients with both N2b and N2c disease (P<0.001). It is important to note that once the number of metastatic lymph nodes was adequately accounted for, the presence of contralateral or bilateral neck disease appeared to provide no additional prognostic value. In our study, the N2 classification seems the most affected than N3 classification this because of N2c being more dangerous disease than N3 ipsilateral lymph node disease. Future studies are needed to determine whether the results are applicable to clinical staging. Moreover, in current study, histological grade is another risk factor for distant metastatic diseases and poorer differentiation was associated with higher incidence of metastasis, which were consistent with many other studies (8,9). We found higher rates of synchronous distant metastases due to the development of diagnostic techniques. In autopsy findings, lung and bone were the most frequent sites of distant metastases and no brain and liver metastasis was found, which were consistent with our study (10). What is different is that distant metastases were much more common when autopsy due to the inclusion of metastases after treatment, but the patterns of metastases were similar.
Compared with colorectal cancer (11) and breast cancer (12), prognosis of metastatic OTSCC is always dismal (13), which is not so much due to malignant biological behaviors of OTSCC as to lack of effective systemic treatment. What's worse, for metastatic OTSCC patients, this a bit less definitively since often treated with combination chemotherapy, evidence for survival benefit cetuximab, advent of nivolumab 2nd line.
In our study, number of metastatic sites was an independent prognostic parameter both for OS and CSS. Many studies have indicated that patients with oligometastases may benefit from local aggressive therapy and increase their life expectancy (14). However, absence of information about performance status of the patients in the current analysis should be taken into account when interpreting these findings as differences in baseline performance may have led to selection bias in the choice of local treatments (i.e., patients with better performance status are being referred to surgery more likely than patients with unfavorable performance status). What’s more, there is a selection bias of oligometastatic disease, which indeed surgeons have been operating primaries in patients with low M+ burden, versus extensive metastatic disease, and this bias is hard to filter out. In addition, benefits of surgery of the primary tumor in cases of a metastatic solid tumor have been suggested for a number of solid tumors including metastatic pancreatic adenocarcinoma and neuroendocrine tumors (15-17) and metastatic hepatocellular carcinoma (18). This strategy is currently being evaluated in a number of ongoing studies for metastatic breast cancer (19,20).
Furthermore, early diagnosis and treatment is of particular importance. In our study, 5-year OS are 58.7% and 38.1% for localized and regional OTSCC patients, respectively, which are much higher than metastatic OTSCC patients (20.6%). The same results were found in CSS (Figure 2).
Better understanding of clinical correlates and prognostic value of distant metastases is helpful in the clinical decision-making process. Since lung is the most frequent site of distant metastases, contrast enhancement computed tomography (CT) on chest should be maintained according to NCCN guideline (21). And for patients with high risk factors of specific site of metastasis, imaging of other sites should be applied. Diagnosis of metastasis is essential not only for staging, but also for further systematic treatment. With the development of medical technology, quantities of therapy methods, including surgery and stereotactic body radiotherapy (SBRT), have been applied to clinical practice for metastases sites and proved to be effective (14).
As far as we know, this is the first SEER analysis assessing clinical correlates and prognostic value of distant metastases in a large cohort of patients with OTSCC. However, there are still some limitations. Firstly, the details about metastases, such as sizes and exact metastatic lesion quantity in specific organ, were not included. Secondly, it is lack of information about systemic therapy options the patients have received. Thirdly, all information on metastases is from their first diagnosis and lack of following information, including treatment modalities of the patients which may confound the assessment of OS analysis. Thus, CSS has been evaluated as a primary outcome in this study to avoid the confounding effect of non-cancer deaths.
Conclusions
In the patients of OTSCC, lung was the most frequent site of distant metastases. The prognosis of OTSCC patients differs considerably according to the age, sex, race, T classification, N classification and histological grade. Poorer prognosis was associated with poorer differentiation and more metastatic sites.
Acknowledgments
We acknowledge the support of the Department of Radiation Oncology.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2018.05.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of Fudan University Shanghai Cancer Center Ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional ethical approval and informed consent were waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Krishnatreya M, Nandy P, Rahman T, et al. Characteristics of oral tongue and base of the tongue cancer: A hospital cancer registry based analysis. Asian Pac J Cancer Prev 2015;16:1371-4. [Crossref] [PubMed]
- Goodman M, Liu L, Ward K, et al. Invasion characteristics of oral tongue cancer. Cancer 2009;115:4010-20. [Crossref] [PubMed]
- Shibahara T. Oral cancer -diagnosis and therapy-. Clin Calcium 2017;27:1427-33. [PubMed]
- Zhang L, Zhou X, Yao X, et al. Oral tongue cancer patients show a better overall survival than base of tongue cancer patients. J Cancer Res Clin Oncol 2012;138:341-6. [Crossref] [PubMed]
- Surveillance, Epidemiology and End Results Program. About the SEER Program. Available online: http://seer.cancer.gov/about, accessed June 25, 2016.
- Ebrahimi A, Gil Z, Amit M, et al. The prognosis of N2b and N2c lymph node disease in oral squamous cell carcinoma is determined by the number of metastatic lymph nodes rather than laterality: evidence to support a revision of the American Joint Committee on Cancer staging system. Cancer 2014;120:1968-74. [Crossref] [PubMed]
- Dickson GH, Singh KK, Escofet X, et al. Validation of a modified GTNM classification in peri-junctional oesophago-gastric carcinoma and its use as a prognostic indicator. Eur J Surg Oncol 2001;27:641-4. [Crossref] [PubMed]
- Rice TW, Rusch VW, Apperson-Hansen C, et al. Worldwide esophageal cancer collaboration. Dis Esophagus 2009;22:1-8. [Crossref] [PubMed]
- Barz H, Barz D. Age dependence of metastases. A study of more than 5000 cases of death from cancer. Arch Geschwulstforsch 1984;54:77-83. [PubMed]
- Institute NC. SEER Stat Fact Sheets: Colon and Rectum Cancer 2016 (cited 2016 09.04). Available online: http://seer.cancer.gov/statfacts/html/colorect.html. 2017.
- Institute NC. SEER Stat Fact Sheets: Female Breast Cancer http://seer.cancer.gov/statfacts/html/breast.html2016 (cited 2016 09.04). SEER 18 2006-12, All Races, Females by SEER Summary Stage 0). Available online: http://seer.cancer.gov/statfacts/html/breast.html. 2017.
- Institute NC. SEER Stat Fact Sheets: Oral Cavity and Pharynx Cancer http://seer.cancer.gov/statfacts/html/oralcav.html2016 (cited 2016 09.04). SEER 18 2006-12, All Races, Females by SEER Summary Stage 0). Available online: http://seer.cancer.gov/statfacts/html/oralcav.html. 2017.
- Lo SS, Moffatt-Bruce SD, Dawson LA, et al. The role of local therapy in the management of lung and liver oligometastases. Nat Rev Clin Oncol 2011;8:405-16. [Crossref] [PubMed]
- Keutgen XM, Nilubol N, Glanville J, et al. Resection of primary tumor site is associated with prolonged survival in metastatic nonfunctioning pancreatic neuroendocrine tumors. Surgery 2016;159:311-8. [Crossref] [PubMed]
- Hüttner FJ, Schneider L, Tarantino I, et al. Palliative resection of the primary tumor in 442 metastasized neuroendocrine tumors of the pancreas: A population-based, propensity score-matched survival analysis. Langenbecks Arch Surg 2015;400:715-23. [Crossref] [PubMed]
- Oweira H, Petrausch U, Helbling D, et al. Prognostic value of site-specific metastases in pancreatic adenocarcinoma: A Surveillance Epidemiology and End Results database analysis. World J Gastroenterol 2017;23:1872-80. [Crossref] [PubMed]
- Abdel-Rahman O. Role of liver-directed local tumor therapy in the management of hepatocellular carcinoma with extrahepatic metastases: A SEER database analysis. Expert Rev Gastroenterol Hepatol 2017;11:183-9. [Crossref] [PubMed]
- Shien T, Nakamura K, Shibata T, et al. A randomized controlled trial comparing primary tumour resection plus systemic therapy with systemic therapy alone in metastatic breast cancer (PRIM-BC): Japan Clinical Oncology Group Study JCOG1017. Jpn J Clin Oncol 2012;42:970-3. [Crossref] [PubMed]
- Ruiterkamp J, Voogd AC, Tjan-Heijnen VC, et al. SUBMIT: Systemic therapy with or without up front surgery of the primary tumor in breast cancer patients with distant metastases at initial presentation. BMC Surg 2012;12:5. [Crossref] [PubMed]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) 2016 (cited 2016 09.14). Version 1.2016. Available online: https://www.nccn.org/professionals/physician_gls/default.aspx#site


