Laparoscopic radical treatment with preservation of left colon artery and superior rectal artery for sigmoid colon cancer
Introduction
During the classical radical treatment for sigmoid colon cancer, especially in patients with advanced diseases, ligation of the inferior mesenteric artery (IMA) at its root is typically performed to achieve better dissection of central and intermediate lymph node groups and improve the surgical outcomes. However, the blood supply to the left colon artery (LCA), sigmoid artery, and superior rectal artery (SRA) is blocked after the ligation at the root of the IMA. While the healing of the anastomosis is the most important factor affecting the success of the surgery, blood supply is one of the key factors affecting the anastomotic healing (1,2). The blood supply to the proximal resection margin of the descending colon and the distal resection margin of the rectum tends to be poor in patient with abnormal vascular anatomy; therefore, the operator has to mobilize the splenic flexure to search for a well-supplied segment of the intestine to establish anastomosis with the rectum, which often requires the mobilization of splenic flexure or even the removal of part of the descending colon. Therefore, laparoscopic radical treatment with preservation of the LCA and SRA for sigmoid colon cancer is particularly meaningful for the preservation of blood supply to the anastomosis.
Indications
It is indicated to treat cancer at the middle portion of sigmoid colon. Generally, cancers near the sigmoid-descending colon junction are treated as descending colon cancer, and those near the sigmoid colon-rectum junction as rectal cancer.
Contraindications
Tumor-related contraindications: (I) tumor >10 cm in diameter and/or with extensive invasion into surrounding tissues and organs; and (II) accompanied by acute intestinal obstruction, perforation, and/or other conditions.
Patient-related contraindications: (I) poor general condition; (II) accompanied with severe heart, liver, lung and kidney diseases and therefore cannot tolerate anesthesia or surgery; (III) extensive abdominal adhesions; (IV) severe obesity; and (V) with underlying diseases that can easily cause bleeding.
Preoperative preparations
- Preoperative examinations are performed to learn the functions of the whole body and the potential lymph node metastasis in liver, lungs, retroperitoneum, and/or mesentery;
- Diseases (e.g., hypertension, diabetes, and coronary heart disease) that may affect the surgery should be controlled;
- Anaemia and hypoproteinemia should be corrected; if necessary, enteral nutrition is added one week before surgery;
- For patients with chronic bronchitis, obstructive emphysema and other respiratory complications before surgery, the respiratory function should be assessed before surgery, along with breathing exercises; if necessary, nebulizers may be applied to facilitate expectoration;
- If the patients have urinary symptoms, cystoscopy or urography should be performed before surgery to exclude the possibility of tumor invasion of the urinary tract; if necessary, ureteral catheter may be indwelled before surgery to facilitate identification of the ureter during surgery;
- Bowel preparation liquid diets are given one day prior to surgery, and laxatives are administered the night before surgery.
Anesthesia
Tracheal intubation under general anesthesia is performed, and continuous epidural anesthesia may be added if necessary.
Body position
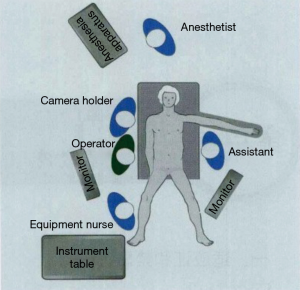
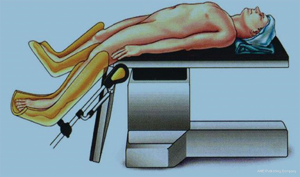
The patient is place on a lithotripsy position, with bilateral hip joint held at 45° of flexion and abduction and knee joint at 30° of flexion. The lower limbs are lower than or flush with the abdomen, the hips are raised, and the right upper limb is adducted (so that the operator and the camera holder can stand at right positions). The left upper limb is adducted or abducted as needed, and the feet are raised 30° over head after the surgery begins (Figure 1). The operator’s standing position is shown in Figure 2.
Operator’s standing position, trocar placement, and main surgical steps
Operator’s standing position
The operator and the camera holder stand at the patient’s right side, and the first assistant at the opposite side of the operator.
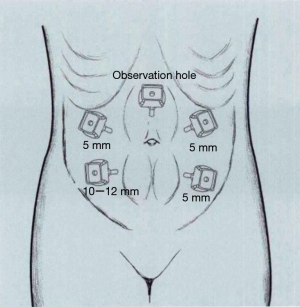
Trocar placement
A 10- or 12-mm trocar is placed on the upper edge of the umbilicus, and the laparoscope is placed as an observation port after the trocar is inflated. A second 12-mm trocar is placed at the McBurney’s point in the right lower abdomen under the laparoscope (two fingers above the anterior superior iliac spine) and used as the main operating port. A 5-mm trocar is inserted at the flat umbilical point on the right midclavicular line as the auxiliary operating port; if the patient is short, the point can be moved upwards by 3–4 cm to facilitate operation. A 5-mm trocar is inserted at the outer 1/3 site of the connection between the left anterior superior iliac spine and the umbilicus as the main operating port for the assistant. Finally, a second 5-mm trocar is inserted 1–2 cm above the umbilicus near the left rectus abdominis muscle as the auxiliary operating port for the assistant (Figure 3).
Main surgical steps
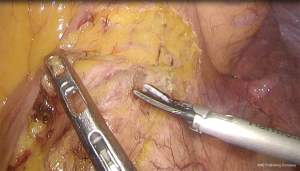
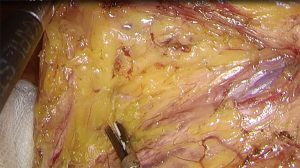
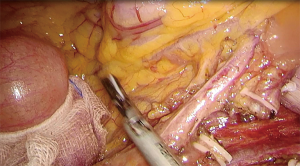
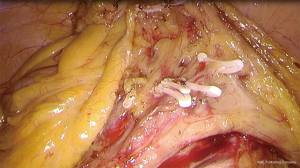
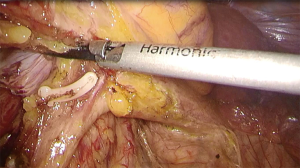
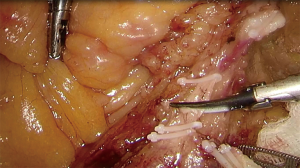
- Mobilization of mesenteric vessels and lymph node dissection: after the exploration is completed, the physiological adhesions of sigmoid colon and lateral peritoneum are firstly separated. After the bifurcation of the abdominal aorta is identified, the right side of the sigmoid mesocolon is cut open along the tibial condyle (Figure 4). After the Toldt’s gap is exposed, mobilization is performed towards its caudal portion (till the rectum-sigmoid junction), cephalic portion (till the root of IMA), and left-sided walls (till the Toldt line), respectively (Figure 5), thus forming a tunnel between the sigmoid mesocolon and the abdominal aorta. The mobilization continues along the tunnel towards the caudal portion and reaches the posterior rectal space, approximately at the S3 level. Special care should be taken to maintain the integrity of the left colonic mesentery and prerenal fascia, so as to avoid damage to the inferior mesenteric plexus, left ureter, and left genital vasculature (Figure 6). Careful dissection of IMA exposes the trunk of IMA. The surrounding lymphatic tissue is dissected from the IMA root to its distal end. The LCA is preserved (Figure 7). After IMA divides LCA, 2–5 sigmoid colon arteries are transected one after another at the distal end of the left colon artery (Figure 8) until it further divides into left and right rectal arteries before entering the lateral wall of rectum. The mobilization continues along the Toldt gap towards the cephalic portion and the left side until the inferior mesenteric vein (IMV) is exposed (Figure 9). After the adjacent lymph nodes are dissected, the IMV is transected at the lower edge of the pancreas (Figure 10). Then, the mobilization continues towards the caudal portion of the pancreas along the Toldt’s gap, and the mesorectum is cut open towards the spleen curvature at the lower edge of the pancreas. If necessary, the colonic splenic flexure should be mobilized to ensure that there is no tension at the anastomosis. The cutting of the descending mesorectum should be performed in the avascular zone near the IMV to avoid any damage to the vascular arch at the edge of the descending colon.
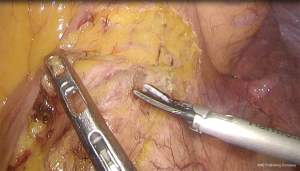 Figure 5 Mobilization towards caudal portion, cephalic portion, and left side after entering the Toldt’s gap.
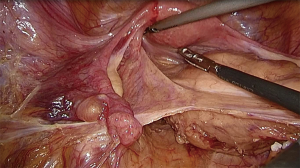
Figure 5 Mobilization towards caudal portion, cephalic portion, and left side after entering the Toldt’s gap.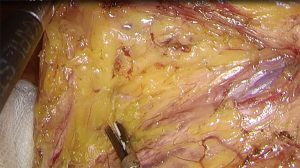 Figure 6 Mobilization along the Toldt’s gap (pay attention to protecting the left ureter and left-sided vessels that feed the reproductive system).
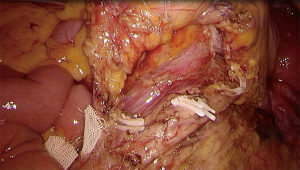
Figure 6 Mobilization along the Toldt’s gap (pay attention to protecting the left ureter and left-sided vessels that feed the reproductive system).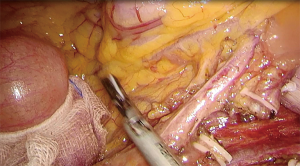 Figure 7 Dissect and skeletonize the IMA trunk, with the LCA preserved. IMA, inferior mesenteric artery; LCA, left colic artery.
Figure 7 Dissect and skeletonize the IMA trunk, with the LCA preserved. IMA, inferior mesenteric artery; LCA, left colic artery. - XMobilization of sigmoid colon and cutting of mesentery: after the transection of the branches of sigmoid artery and IMV, the lateral peritoneum and the retroperitoneum behind left paracolic sulcus can be cut open along the Toldt’s line at the left side of sigmoid colon. If the above-mentioned “tunnel” has been fully mobilized, cutting along the Toldt’s line can achieve the communication with the “tunnel”. If the “tunnel” has not been fully mobilized, the sigmoid colon can be pulled to the right to fully expose the Toldt’s gap (Figure 11). Mobilizing along this gap till the original “tunnel” can achieve the complete mobilization of the entire sigmoid colon. If the sigmoid colon is found to be short and the intestine might not be long enough after tumor resection, mobilization of the left colic flexure may be considered.
- Removal of tumor and reconstruction of the digestive tract: if the sigmoid colon is long, extraperitoneal resection and anastomosis can be performed. The original camera port can be utilized to create umbilical midline incision, and side-to-side or end-to-side anastomosis is performed after the tumor is removed (Figure 12). Notably, at least 10 cm of bowel on both sides of the tumor should be resected. If the extraperitoneal anastomosis is not feasible, the bowel can be skeletonized 10 cm beneath the lower edge of tumor, followed by the laparoscopic transection of the bowel by using the linear cutter stapler. The precut site at proximal bowel is marked with a titanium clip to ensure that there is no tensional anastomosis after transection. After the tumor is resected, the proximal bowel is placed into the anvil of the stapler to return to the abdominal cavity, and the pneumoperitoneum is then reconstructed. The stapler is inserted via the anus to complete the anastomosis with the proximal bowel, during which the bowel should not be twisted. If there is a large tension on the anastomosis, the splenic flexure of the descending colon must be further mobilized to the cephalic side. After the anastomosis is completed, routinely check the integrity of two anastomosis rings on the stapler and place a drainage tube close to the anastomosis before the abdomen is closed.
Key points of surgery
Maintaining a correct anatomical plane
The dissection must be performed on the correct anatomical plane (i.e., the Toldt’s gap). The Toldt’s gap is a fascial plane which is formed by the fusion of left mesentery and prerenal fascia.
Transection of vessels
Vessels should be transected at the origins of the branches of sigmoid artery where the IMA divides, along with the dissection of lymphoadipose tissues around the vessels.
Reducing the incidence of anastomotic leak
Maintaining anastomotic blood supply, reducing tension, and preventing infections are key measures to reduce the incidence of anastomotic leak. The left colon artery and SRA should be preserved. If there is a large tension on the anastomosis, the bowel shall be thoroughly mobilized, along with good nutritional support and adequate preoperative preparation.
Discussion
Lymph node metastasis of sigmoid colon cancer has been widely recognized as one of the most important factors leading to poor prognosis. Therefore, both the scope of lymph node dissection and the quality of surgical specimens can affect the prognosis. For patients with locally advanced sigmoid colon cancer, D2 lymph node dissection (i.e., the removal of lymph nodes around the colon, in the intermediate group, and at the root of IMA) is typically recommended. During the classical radical treatment of sigmoid colon cancer, ligation of the IMA at its root is often performed to ensure better scope of lymph node dissection (3,4). Kanemits et al. (5) reported that high ligation of the IMA prolonged the survival of patients, and postoperative pathology confirmed that the 5-year survival rate reached 40% in patients with lymph node metastases at the root of IMA. Chin et al. (6) also had similar findings. This procedure is simple and time-saving and is helpful for freeing the descending colon and lowering the tension of the descending colon-rectum anastomosis. However, the ligation of the IMA at its root also blocks the blood supply of the left colon artery, sigmoid arteries, and SRA and reduces blood supply to the descending colon-rectum anastomosis (1,2). Anatomically, most of the rectal blood supply above the dentate line comes from the SRA; furthermore, while the blood supply of the distal rectum and anal canal mainly depends on the middle rectal artery and the internal pudendal artery, the descending colon is mainly supplied by the left branch of middle colonic artery and LCA. It has been reported that about LCA is absent in about 12% of patients (7). In patients with certain physiological/anatomical abnormalities (e.g., the LCA offers major blood supply to the descending colon, especially the distal end of the descending colon), the LCA should be preserved to the maximum extent possible. Furthermore, in order to achieve the optimal oncological cure, the LCA and the SRA should be completely skeletonized and preserved while dissecting the lymphoadipose tissues near the IMA, along with ligation of the branch of sigmoid artery at its origin. Such a procedure not only fully ensures the oncological effectiveness of the radical treatment but also satisfies the blood supply required by descending colon and rectum. The tension of the descending colon-rectum anastomosis will not increase after surgery. Dissection of the lymphoadipose tissues at the root of IMA with the preservation of LCA and SRA does not significantly increase the operative time and blood loss compared with the direct ligation of the IMA at its root. Finally, postoperative pathology has confirmed the number of lymph node harvested was comparable between two groups, which was consistent with literature (8).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2018.05.14). The authors have no conflicts of interest to declare.
Ethical statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dworkin MJ, Allen-Mersh TG. Effect of inferior mesenteric artery ligation on blood flow in the marginal artery-dependent sigmoid colon. J Am Coll Surg 1996;183:357-60. [PubMed]
- Seike K, Koda K, Saito N, et al. Laser Doppler assessment of the influence of division at the root of the inferior mesenteric artery on anastomotic blood flow in rectosigmoid cancer surgery. Int J Colorectal Dis 2007;22:689-97. [Crossref] [PubMed]
- Titu LV, Tweedle E, Rooney PS. High tie of the inferior mesenteric artery in curative surgery for left colonic and rectal cancers: a systematic review. Dig Surg 2008;25:148-57. [Crossref] [PubMed]
- Lange MM, Buunen M, van de Velde CJ, et al. Level of arterial ligation in rectal cancer surgery: low tie preferred over high tie. A review. Dis Colon Rectum 2008;51:1139-45. [Crossref] [PubMed]
- Kanemitsu Y, Hirai T, Komori K, et al. Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery. Br J Surg 2006;93:609-15. [Crossref] [PubMed]
- Chin CC, Yeh CY, Tang R, et al. The oncologic benefit of high ligation of the inferior mesenteric artery in the surgical treatment of rectal or sigmoid colon cancer. Int J Colorectal Dis 2008;23:783-8. [Crossref] [PubMed]
- Horton KM, Fishman EK. 3D CT angiography of the celiac and superior mesenteric arteries with multidetector CT data sets: preliminary observations. Abdom Imaging 2000;25:523-5. [Crossref] [PubMed]
- Sekimoto M, Takemasa I, Mizushima T, et al. Laparoscopic lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery. Surg Endosc 2011;25:861-6. [Crossref] [PubMed]