
Hypofractionated radiosurgery for meningiomas—a safer alternative for large tumors?
Meningiomas are a common non-glial primary brain tumor. While they have a generally favorable prognosis, they may progress locally and result in neurologic deficits from mass effect on adjacent brain or cranial nerves, and they can sometimes cause seizures. The main goal of treatment of benign meningiomas is the prevention of mass-related symptoms. Surgical resection is the preferred treatment for patients with symptomatic, intracranial meningiomas as it relieves mass effect for large tumors, permits pathologic grading, and reduces the chance of tumor recurrence or progression. However, the rate of recurrence after incomplete resection can be high. In 1957, Simpson (1) published a landmark article in which he described WHO grade I meningioma recurrence rates to be 9% after complete resection including the dural base, 19% after excision and coagulation of the dural base, 29% after excision without coagulation of the dural base, and 40% after subtotal resection. Condra (2) confirmed Simpson’s results, and demonstrated that adjuvant treatment of subtotally resected tumors results in tumor control rates equivalent to gross-total resection. Additionally, many tumors arise deep within the skull base or near eloquent areas, making complete surgical resection difficult or impossible.
Stereotactic radiosurgery has historically been delivered in a single, large dose of radiation. This is due to the fact that in many systems, a fixed frame must be placed before treatment in order to localize the tumor. The dose to the periphery of the tumor is generally between 12-16 Gy (3). However, treatment of larger volumes in a single dose can result in unacceptably high rates of symptomatic peritumoral edema and other side effects (4-9). In recent years, newer systems have allowed for similar precision without the requirement of a fixed frame, allowing for multiple extremely precise, highly conformal treatments. According to the ASTRO stereotactic radiosurgery (SRS) Model Coverage policy, “SRS typically is performed in a single session, using a rigidly attached stereotactic guiding device, other immobilization technology and/or a stereotactic-guidance system, but can be performed in a limited number of sessions, up to five”. So-called hypofractionated radiosurgery couples the precision and convenience of single-fraction radiosurgery while possibly causing fewer side effects. The dose to the periphery of the tumor is most commonly 25 Gy in 5 fractions. In this study we review 28 patients who were treated with hypofractionated radiosurgery to determine the rate of tumor control and factors associated with relief of symptoms and radiation-related complications after hypofractionated radiosurgery for patients with postoperative and imaging defined intracranial meningiomas.
Methods
Patient population
Patient information was taken from a prospective database approved by Scripps Mercy Hospital Institutional Review Board. Thirty-four patients with a total of 36 lesions with the clinical and imaging findings of a meningioma with at least 12 months of follow up were identified. Of these 34 patients, 3 were lost to follow up shortly after treatment, 2 who were treated palliatively for large, symptomatic tumors died of other causes within 1 year of treatment, and 1 refused consent to have her information shared.
The patients’ mean age was 60 years. The majority of tumors involved the skull base (n=15, 50%) and the convexity (n=8, 27%). The mean treatment volume was 14.7 cm3 (range, 0.79-64.5 cm3), median 9.4 cm3. The prescription isodose line ranged from 58% to 90%, median 78%. Most patients were treated with a 5 fraction course of 4.5 to 6 Gy/fraction. The mean new conformality index was 1.61 (range, 1.2-2.28). The formula for the new conformality index is CI = (PVTV + NTV)/PVTV, where PVTV is the volume of target TV encompassed by the prescription isodose surface, and NTV is the volume of the normal tissue encompassed by the prescription isodose surface. Mean follow up is 32.6 months, ranging from 12-66 months. Nineteen of the patients were treated for imaging-defined meningiomas, while nine were treated either adjuvantly (six) or for recurrence after previous resection (three). Two of these patients were noted to have atypia histologically.
Radiosurgery technique
All patients were treated with the CyberKnife system. Patients were immobilized with an Aquaplast facemask and underwent CT imaging with 1.25 mm thick axial slices. A gadolinium enhanced MRI scan was fused with the treatment planning CT in all cases. The planning treatment volume was defined as the gross tumor volume with no additional margin. Inverse planning was used to determine the dose to the target volume, while minimizing the dose to adjacent critical structures.
Patient follow-up
Post treatment MRI scans were typically obtained at 3 months following treatment and every 6 months thereafter until 2 years post treatment, at which time MRI scans were obtained yearly. Neurological symptoms were clinically assessed and recorded by the attending radiation oncologists and neurosurgeons. Peritumoral edema was assessed on T2 weighted and FLAIR MRI sequences. Patient steroid requirements were assessed at each follow-up visit.
Results
Progression-free survival and clinical outcomes
Tumor control was evaluated by serial imaging, assessed by measurements of maximal axial and craniocaudal dimensions, and performed at the same imaging center whenever possible. In all cases the images were also reviewed by one or more of the authors. There were no instances of in-field progression; one patient experienced marginal progression outside the field (scalp nodules) which required surgical resection. Eight patients presented with symptoms prior to treatment: one had severe facial pain, one had weakness of the upper extremity, one had numbness of the upper extremity, one had vertigo, one had hearing loss, one had diplopia, one had facial numbness, one had headaches, and one had visual loss (one patient had both upper extremity numbness and headaches). The patient with severe facial pain experienced complete resolution of her pain within 3 months after treatment. The patients with weakness of the upper extremity and vertigo experienced complete resolution of their symptoms within one year after treatment. The patient with upper extremity numbness and headaches experienced no change in his numbness but improvement of his headaches. The patients with hearing loss and diplopia experienced improvement but not complete resolution of their symptoms at the time of last follow up. The patients with facial numbness and visual loss experienced persistence, but no worsening, of their symptoms at the time of last follow up.
Post radiosurgery complications
Four patients experienced side effects as a result of their treatment. One patient with a parasagittal tumor experienced increasing hemiparesis as a result of increased peritumoral edema. A resection was performed, resulting in improvement of the hemiparesis to baseline. One patient with a tumor near the orbital apex experienced diplopia. This is persistent at 17 months and is being treated with a prismatic lens. One patient with a skull based tumor in the infratemporal fossa, who had been treated with surgery and external beam radiation therapy prior to radiosurgery and who was treated to a very large volume (65 cm3), experienced cognitive changes and headaches requiring months-long steroid therapy. These symptoms have since resolved. One patient with a convexity lesion experienced headaches secondary to post-treatment edema causing headaches which required a 3 months long course of steroid therapy. Thus the rate of complications in our series for convexity tumors was 25% (2 of 8) while the rate for skull base tumors was 7% (1 of 15). The rate of permanent morbidity is 3.5%. No patient died of tumor or treatment-related causes.
Discussion
Single-fraction radiosurgery has a long track record of successful treatment of meningiomas, both in the definitive and adjuvant setting (4,5,10-12). Santacroce (10) reported on 4,565 consecutive patients harboring 5,300 meningiomas from 15 participating Gamma Knife centers. Detailed results from 3,768 meningiomas were analyzed. The 5- and 10-year progression-free survival rates were 92.5% and 88.6% respectively. The median tumor volume was 4.8 cm3. Complications developed in 12.9% of patients. In 6.6% of their patients the complications were permanent. Pollock (4) reported on 416 patients treated with Gamma Knife radiosurgery from 1990 to 2008. The 10-year local control rate was 89%. The median tumor volume was 7.7 cm3. The permanent complication rate was 11.5%. Zada (5) reported on 116 patients who underwent 136 Gamma Knife radiosurgery treatments with a median follow up time of 75 months. The 5- and 10-year actuarial tumor control rates were 99% and 84% respectively. The median tumor volume was 3.4 cm3. Complications developed in 8% of patients.
Several studies identified a higher incidence of complications in patients with larger tumors. Pollock (13) reported radiation-related complications in 4.8% of patients with tumor volumes in the lowest quartile (<3.2 cc) compared with 22.6% for patients with tumor volumes in the highest quartile (>9.6 cc). Zada (5) reported a complication rate in 8% of their patients, in whom the mean tumor volume was nearly double that in patient with no adverse effects (11 vs. 5.7 cm3).
Bledsoe (6) demonstrated, in a series of large tumors with an average volume of 17.5 cm3, equivalent tumor control rates but an increased rate of complications of 23%. The average rate of complications from all radiosurgery series published between 2000-2010 was 9.5% (14). Maruyama (7) reported a higher incidence of permanent cranial nerve deficits when the tumor volume was greater than 10 cm3. Kim (8) demonstrated a statistically significant increase in peritumoral edema in lesions greater than 4.2 cm3. Unger (9) reported a 24-month actuarial rate of development of symptomatic edema of 15.8% for tumors larger than 4.9 cm3 versus 2.2% for tumors smaller than 4.9 cm3. Location of tumor can also be a factor in the development of complications. The rate of complications in our series for convexity tumors was 25% (2 of 8) while the rate for skull base tumors was 7% (1 of 15). Pollock (13) also reported radiation-related complications in 26.8% of patients with tumors involving the falx or cerebral convexities and 9.5% of patients with skull-base tumors.
Several authors (9,15-20) have reported results using a hypofractionated approach for treatment of intracranial meningiomas. Unger (9) reported on 173 patients, of whom 97 received single-fraction radiosurgery and 74 received fractionated radiosurgery of 2 or more fractions. The crude tumor control rate was 94%. Oermann (15) reported a 100% local control at relatively short follow up (median 20 months) for 38 patients treated with 5 fraction radiosurgery. Post-treatment symptomatic peritumoral edema occurred in 5 patients (13%). Han (20) demonstrated excellent efficacy (radiographic control of
A hypofractionated approach may be useful for prevention of post treatment edema and other side effects. Unger (9) found in his series of patients treated with both single-fraction radiosurgery and hypofractionated radiosurgery that large tumor volumes and single-fraction radiosurgery had an increased risk for post treatment edema. Han (20) reported symptomatic edema in 11% of their patients treated with single-fraction radiosurgery and only 4% in their patients treated with a hypofractionated approach, although the difference was not statistically significant. Additionally, the rate of cranial nerve injury, which usually manifests as new or worsened facial pain or numbness, may be lower with a hypofractionated approach. In Pollock’s series (4) of 416 patients treated in a single fraction, 24 patients (5.7%) developed this complication. In contrast, Colombo (21) reported only 1 out of 199 patients (0.5%) developing this complication after hypofractionated radiosurgery using CyberKnife. Han (20) reported worsened facial pain in four patients (7%) treated with single-fraction radiosurgery and none in patients treated with a hypofractionated or fractionated approach. This complication was not seen in our series. Nevertheless, since the alpha/beta ratio of cerebral tissue is relatively small, the risk of developing side effects can only be completely assessed with long-term follow up, and this is a potential limit of the present study. See clinical cases 1 and 2 for relevant examples of cases treated.
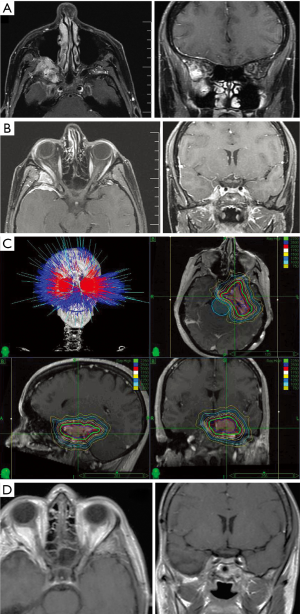
Clinical case 1. Sphenoid Wing Meningioma: a 55-year-old female presented with gradual onset of right periorbital pain and progressive exophthalmos. MRI revealed a tumor involving the right sphenoid wing extending into the infratemporal fossa and cavernous sinus (Figure 1A). After presentation at multidisciplinary skull base conference, she underwent an orbitozygomatic craniotomy with post-operative vision and hearing preservation. Pathology confirmed meningioma. Subsequent MRI demonstrated resection of >90% of the gross tumor volume with residual tumor involving the cavernous sinus, the anterior aspect of Meckel’s cave, and the superior orbital fissure (Figure 1B). Cyberknife Radiosurgery was administered with a dose of 2,400 cGy in 4 fractions delivered to a tumor volume of 6.8 cm3 to the 85% isodose line in 186 beams and conformality index of 1.44 (Figure 1C). Follow-up imaging at 5 years shows no tumor progression (Figure 1D).
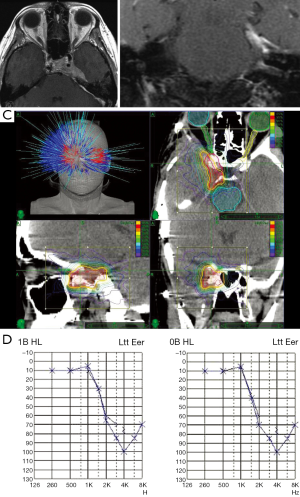
Clinical case 2. Petroclival Meningioma: a 54-year-old female presented with a 1-month history of left cheek dysesthesia prompting evaluation with CT and subsequent MRI which revealed a large CPA mass centered on petroclinoid dura, indenting the lateral surface of the pons with medial extension to the cavernous sinus (Figure 2A). Her case was reviewed at the multidisciplinary skull base conference and she underwent left retrosigmoid craniotomy with debulking of a posterior fossa tumor and complete decompression of the trigeminal nerve and the pons. The patient recovered with normal facial nerve function and post-op MRI confirmed gross resection of the CPA component of the tumor (Figure 2B). The residual cavernous sinus component was treated using a Cyberrknife Radiosurgery plan of 2,250 cGy delivered in five fractions with 137 beams to a tumor volume of 16.6 cm3, and 78% isodose line with conformality index of 1.38 (Figure 2C). The patient has residual post-op ipsilateral hypesthesia and post-op audiogram showed no significant change in functional hearing (Figure 2D).
Conclusions
In our series, a high rate of local control was obtained, with a low incidence of complications, in a heterogeneous group of patients who had significantly larger tumors than is generally reported (median 9.4 cm3 in our series vs. 4.8 cm3 in Santacroce’s report of 3,768 meningiomas treated). Hypofractionated radiosurgery, delivered in a dose of 22.5-30 Gy in 5 fractions, appears to offer excellent local control with a lower incidence of complications than single-fraction radiosurgery. Longer follow up is needed to confirm these findings.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Sandra Vermuelen, Kevin T. Murphy, Huan Giap) for the series “SBRT/SRS in Radiation Research” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.3978/j.issn.2218-676X.2014.08.02). The series “SBRT/SRS in Radiation Research” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Scripps Mercy Hospital Institutional Review Board. Written informed consent was obtained from the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 1957;20:22-39. [PubMed]
- Condra KS, Buatti JM, Mendenhall WM, et al. Benign meningiomas: primary treatment selection affects survival. Int J Radiat Oncol Biol Phys 1997;39:427-36. [PubMed]
- Kollová A, Liscak R, Novotny J, et al. Gamma knife surgery for benign meningioma. J Neurosurg 2007;107:325-36. [PubMed]
- Pollock BE, Stafford SL, Link MJ, et al. Single-fraction radiosurgery of benign intracranial meningiomas. Neurosurgery 2012;71:604-12. [PubMed]
- Zada G, Pagnini PG, Yu C, et al. Long-term outcomes and patterns of tumor progression after gamma knife radiosurgery for benign meningiomas. Neurosurgery 2010;67:322-8. [PubMed]
- Bledsoe JM, Link MJ, Stafford SL, et al. Radiosurgery for large-volume (>10cm3) benign meningioma. J Neurosurg 2010;112:951-6. [PubMed]
- Maruyama K, Shin M, Kurita H, et al. Proposed treatment strategy for cavernous sinus meningiomas: a prospective study. Neurosurgery 2004;55:1068-75. [PubMed]
- Kim DG, Kim Ch H, Chung HT, et al. Gamma knife surgery of superficially located meningioma. J Neurosurg 2005;102:255-8. [PubMed]
- Unger KR, Lominska CE, Chanyasulkit J, et al. Risk factors for posttreatment edema in patients treated with stereotactic radiosurgery for meningiomas. Neurosurgery 2012;70:639-45. [PubMed]
- Santacroce A, Walier M, Regis J, et al. Long-term tumor control of benign intracranial meningiomas after radiosurgery in a series of 4565 patients. Neurosurgery 2012;70:32-9. [PubMed]
- Starke RM, Nguyen JH, Rainey J, et al. Gamma Knife surgery of meningiomas located in the posterior fossa: factors predictive of outcome and remission. J Neurosurg 2011;114:1399-409. [PubMed]
- Ding D, Xu Z, McNeill IT, et al. Radiosurgery for parasagittal and parafalcine meningiomas. J Neurosurg 2013;119:871-7. [PubMed]
- Pollock BE, Stafford SL, Link MJ, et al. Single-fraction radiosurgery for presumed intracranial meningiomas: efficacy and complications from a 22-year experience. Int J Radiat Oncol Biol Phys 2012;83:1414-8. [PubMed]
- Bloch O, Gurvinder K, Jian BJ, et al. Stereotactic radiosurgery for benign meningiomas. J Neurooncol 2012;107:13-20. [PubMed]
- Oermann EK, Bhandari R, Chen VJ, et al. Five fraction image-guided radiosurgery for primary and recurrent meningiomas. Front Oncol 2013;3:213. [PubMed]
- Bria C, Wegner RE, Clump DA, et al. Fractionated stereotactic radiosurgery for the treatment of meningiomas. J Cancer Res Ther 2011;7:52-7. [PubMed]
- Morimoto M, Yoshioka Y, Shiomi H, et al. Significance of tumor volume related to peritumoral edema in intracranial meningioma treated with extreme hypofractionated stereotactic radiation therapy in three to five fractions. Jpn J Clin Oncol 2011;41:609-16. [PubMed]
- Kaul D, Budach V, Wurm R, et al. Linac-based stereotactic radiotherapy and radiosurgery in patients with meningioma. Radiat Oncol 2014;9:78. [PubMed]
- Marchetti M, Bianchi S, Milanesi I, et al. Multisession radiosurgery for optic nerve sheath meningiomas – an effective option: preliminary results of a single-center experience. Neurosurgery 2011;69:1116-22. [PubMed]
- Han J, Girvigian MR, Chen JC, et al. A Comparative Study of Stereotactic Radiosurgery, Hypofractionated, and Fractionated Stereotactic Radiotherapy in the Treatment of Skull Base Meningioma. Am J Clin Oncol 2012; [Epub ahead of print]. [PubMed]
- Colombo F, Casentini L, Cavedon C, et al. Cyberkife radiosurgery for benign meningiomas: short-term results in 199 patients. Neurosurgery 2009;64:A7-A13. [PubMed]


