
Assessing patient navigation as a tool to address equity in cancer early detection
Introduction
Many cancers can be prevented or detected early enough to be cured. However, not all people have equal access to prevention and early detection services, leaving marginalized and underserved populations with the poorest cancer outcomes. Such populations include racial/ethnic minorities and rural residents (1-3). Racial/ethnic minorities are dying of breast cancer at a higher rate than White women in large part because of late diagnosis (1,3). Even with the advancements of early cancer detection tests, racial/ethnic minority women continue to be diagnosed at a late stage (1,3).
Early detection of breast and cervical cancer is critical to decrease mortality rates and improve survival outcomes in the US. In order to address this public health problem, Congress passed the Breast and Cervical Cancer Mortality Prevention Act of 1990, which led to the creation of the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) at the US Centers for Disease Control and Prevention. This national program funds all 50 states, the District of Columbia, six US territories and 13 American Indian/Alaska Native tribes or tribal organizations (4). With funding from NBCCEDP, the Louisiana Breast and Cervical Health Program (LBCHP) was established in 2002 with the goal of reaching underserved populations. LBCHP provides no-cost breast and cervical cancer early detection services to uninsured and underinsured, low-income women throughout Louisiana. Services include screening via Pap test and mammogram; diagnostic services such as colposcopy, ultrasound and biopsy; and patient navigation to help participants address emotional and logistical barriers to completing care. LBCHP has 14 clinical provider site partners administering early detection services across the state (5). Patient navigation data are collected on all women who complete their screening.
Similar to most states, Louisiana has undergone healthcare system changes requiring adaption, innovation, and flexibility. Louisiana expanded Medicaid in 2016, and since then, the state has reduced the number of residents with inadequate health coverage by 50% (6). In order to adapt to the decrease in uninsured women, LBCHP shifted the focus of its patient navigation component to better reach all underserved, low-income women. LBCHP has a total of 14 patient navigators in 14 clinical provider sites located in Louisiana’s nine most populous cities (one navigator per site). Having a patient navigator at each site helps to reduce barriers to early detection for women in the surrounding area. In the past, the navigation focused on low-income, uninsured women with abnormal screening results for completion of diagnostic testing and starting treatment; however, with the decrease in the uninsured rate, navigation has been refocused to include any woman meeting the age and income eligibility requirements and needing help with screening and/or diagnostic services.
Patient navigation is a service provided to individuals struggling with healthcare system barriers. A patient navigator is defined as:
“A person who helps guide a patient through the healthcare system. This includes help going through the screening, diagnosis, treatment, and follow-up of a medical condition, such as cancer. A patient navigator helps patients communicate with their healthcare providers so they get the information they need to make decisions about their health care. Patient navigators may also help patients set up appointments for doctor visits and medical tests and get financial, legal, and social support. They may also work with insurance companies, employers, case managers, lawyers, and others who may have an effect on a patient’s healthcare needs.” (7).
The purpose of patient navigation is to reduce barriers for medically underserved and vulnerable populations confronting the United States’ complex and sometimes overwhelming healthcare system (2,8-10). Some of the most significant barriers include unreliable transportation, cultural differences, inadequate insurance, shortage of support systems, and lack of education. By improving access to early diagnosis and treatment through navigation, mortality rates decrease and quality of life improves (3,8). Patient navigation has played an important role in improving timeliness of diagnosis and access to treatment and has been shown to improve outcomes for underserved racial/ethnic minority populations, specifically Black and Latinx women (2,9). Additionally, navigators can play a critical role in underserved rural communities where there often is poor access to healthcare leading to higher breast cancer mortality and morbidity (10).
In this paper, we explore if LBCHP is addressing health inequities specifically by examining how well navigation is reaching subpopulations of underserved populations in Louisiana, that is, racial/ethnic minority women and rural residents. Previous papers have identified that low-income women benefit from patient navigation services, but to our knowledge, no paper has attempted to measure if racial/ethnic minorities and rural population access these services equitably. By estimating the number of women who meet LBCHP’s eligibility criteria and comparing these data with LBCHP navigation services data, this paper identifies how well LBCHP is reaching specific subpopulations of racial/ethnic minorities and rural residents by parish (county) and region and provides a methodology that can be used by other programs.
Methods
This analysis includes all women who participated in LBCHP and received patient navigation services at one of LBCHP’s 14 participating healthcare facilities between July 01, 2016 and June 30, 2018. To qualify for LBCHP early detection services, including patient navigation, women must be between the ages of 21–64 years and have a household income at or below 250% of the federal poverty level (FPL). The FPL is a measure assigned by the Census Bureau. Household income thresholds vary by family size to determine poverty levels. Often percent of these thresholds are used by programs to assess eligibility for programs (11). To match LBCHP’s eligibility criteria of at or below 250% FPL, the FPL for 2019 was multiplied by 2.5 or 250%. For a single person household, for example, the FPL is $12,490 which when multiplied by 2.5 gives the eligibility threshold of $31,225 (12).
Screening services are provided to women who are due or past due for breast (mammogram) or cervical (Pap test) screening in accordance with United States Preventive Services Task Force recommendations; diagnostic services are provided to women with a recently abnormal mammogram or Pap test and/or women whom present with symptoms. Between July 01, 2016 and June 30, 2018, LBCHP served 5,431 women with 4,007 mammograms and 1,439 Pap tests.
To be considered navigated, women had at least one barrier identified and had a minimum of two contacts with a program navigator to resolve the barriers that resulted in screening or diagnostic services. Barriers are grouped into the following categories: uninsured, needing information/education, limited or inflexible appointment times, long wait times, financial distress not related to insurance, and not speaking English. The patient navigator identifies these types of barriers using a barriers assessment in person or over the phone. Once barriers are identified, the navigator is able to personalize each patients’ path to screening or diagnostic services completion. Demographic information (e.g., age at service, race/ethnicity and residential address) and medical information (e.g., breast and cervical screening tests, results and diagnoses) from LBCHP patient records were used in this analysis. We calculated differences between percentages of detected abnormalities and percentages with complete follow-up for each racial/ethnic group. We assessed statistically significant differences using a chi-square test (differences across all racial/ethnic groups) and t-tests for comparisons of percentages between specific racial/ethnic group; differences were considered statistically significant at P<0.05.
We used the combination of U.S. Census Bureau’s Small Area Health Insurance Estimates (SAHIE) 2016 (13) and the American Community Survey (ACS) 2017 5-year file (14) to calculate the number of eligible women by race/ethnicity and parish (county). ACS provides a more accurate estimate of population counts at the parish level than SAHIE data, but does not provide the population counts at or below 250% FPL that were needed to estimate the number of eligible women. Therefore, we used SAHIE counts to calculate the percentage of the female population ages 21–64 years at or below 250% FPL by parish, and statewide percentages at or below 250% FPL by race/ethnicity (a breakdown by race/ethnicity were unavailable at the parish level). We applied these poverty percentages to the ACS base population count estimates (all income levels) to estimate the number of women ages 21–64 years at or below 250% FPL by race/ethnicity in each parish. We used SAHIE to estimate percentages of women at or below 250% FPL by parish accounting for the varying poverty rates by race/ethnicity and racial/ethnic distribution within the parish. This methodology allowed us to create count estimates of the eligible population by race/ethnicity for each parish while accounting for different poverty percentages by race/ethnicity and by parish. The data were not adjusted for different years represented by the two sets. Though imperfect, both datasets provided the most up-to-date estimates at the time of the analysis. In the case of ACS, a 5-year file [2013–2017] was used to stabilize small estimates by parish and race/ethnicity, which includes 2016, the year of the SAHIE data. We assessed statistically significant differences using a chi-square test (differences between LBCHP patient navigated clients and the population at or below 250% FPL) and t-tests for comparisons of percentages between specific racial/ethnic group; differences were considered statistically significant at P<0.05.
We used the 2010 Census Summary File 1 (15) to estimate the distribution of the geographic mix of the population by the 336 cities or census designated places which then were aggregated into the 64 parishes and then into nine regions (see Figure 1). This file subdivided the total counts within a city and for the parish into three categories: inside urbanized area, inside urban cluster (suburban) and rural. These proportions were used to assign the estimated counts of LBCHP-navigated women based on their residential addresses into urban, suburban and rural, which we also aggregated to the parish level. We then aggregated parish-level data to nine administrative regions as defined by the Department of Health and Hospitals (16). LBCHP has at least one clinic in each of these nine regions. Because the study was not intended, nor should be used to evaluate individual clinics, the identity of each region is identified in this article with a randomly chosen capital letter. We calculated the P values testing the equality of Blacks, Latinx, rural and suburban proportions who were served versus not served by region using two sample tests of proportions at the P<0.05 level.
Results
Proximity of navigation services to eligible population
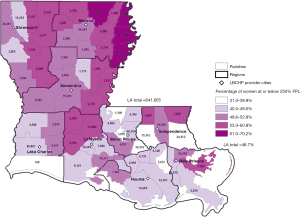
The Louisiana population of women ages 21–64 years is 1.37 million, of which almost half, 641,600 or 46.7%, qualify for LBCHP based on income estimates (at or below 250% FPL). Figure 1 displays the number of women by parish (county) who are eligible for LBCHP. The figure also includes the locations of LBCHP’s navigation services, which are in 14 clinical provider sites in nine cities. These nine cities are located within parishes that account for half of all the LBCHP-eligible population in the state.
High poverty areas and racial/ethnic minorities
Overlaid on Figure 1 is the overall percentage of women ages 21–64 years in the parish who live at or under 250% FPL. This additional information shows where there may be higher need. Poverty rates among the 64 parishes ranged from 31% to 70%. The map shows that the rural, northeastern part of Louisiana has the highest rates of women at or under 250% FPL but low population counts. It is more difficult to reach high numbers women in these less-populated parishes.
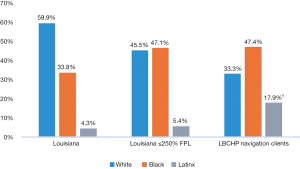
The population of White women ages 21–64 years in Louisiana is almost double that of Black women (59.9% vs. 33.8%, respectively) (Figure 2). However, the percentage of the population living at or under 250% FPL is much higher among LBCHP’s racial/ethnic minorities: 65.0% of Black women and 58.4% of Latinx women, compared to 35.4% of White women (Data not shown, SAHIE 2016). These higher poverty rates among racial/ethnic minorities affect the racial/ethnical distribution of women who qualify for LBCHP. Because of the disparity in 250% FPL rates between these two groups, more Black women qualify for LBCHP than White women (310,322 vs. 285,231) despite having a lower proportion of Black to White women in Louisiana (see Figure 2). To reach racial/ethnic equity, LBCHP participants would need to be at least 47% Black women and 5% Latinx women, the percentages of the state population living in poverty represented by these two groups. The population LBCHP served was not significantly different among Black women (47% vs. 47%, P=0.5959) but was higher among Latinx women (18% vs. 5%, P<0.0001).
Racial equity by region
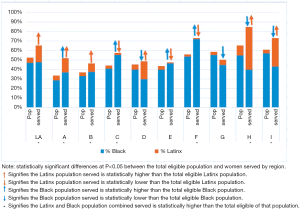
We analyzed the distribution of LBCHP’s clients’ race/ethnicity by parish and region. We serve a higher percentage of racial/ethnic minority women in LBCHP (65%) compared to the overall racial/ethnic minority eligible population in Louisiana (49%) (P<0.0001). More specifically, in every region but three (Region “D”, “E” and “G”), LBCHP serves a higher percentage of racial/ethnic minorities than the overall percent in that region (Figure 3, P<0.05). The Latinx eligible population is particularly well served. LBCHP serves a statistically significantly higher percentage of Latinx than the overall percent in that region in five out of the nine regions (see Figure 3, P<0.05) and significantly lower in 3 out of 9 regions. In Louisiana, Latinx women are 3.3 times more likely to receive LBCHP navigation services than their respective proportion in the state (17.9% vs. 5.4%). Among Black women the pattern is much less consistent with regions “A”, “C”, “E” and “F” having higher service proportions and regions “D”, “G”, “H” and “I” having lower service proportions (see Figure 3, P<0.05). As stated earlier, overall, Black women do not have a statistically significant difference in the percentage served by our program than is proportional to their population in Louisiana.
Rural communities
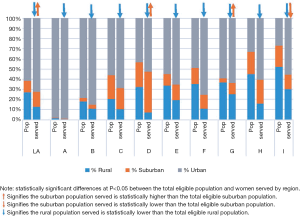
We examined the rural/suburban/urban mix of LBCHP’s clients by region (Figure 4) and parish (data not shown). There were slightly higher rates of suburban women served in LBCHP compared to the overall eligible percentage in Louisiana (15% vs. 12%, P<0.05) and no clear pattern by region. In contrast, there were lower rates of rural women served in LBCHP compared to the overall eligible percentage in Louisiana and in every single region (P<0.05). While 27% of Louisiana is rural, only 17% of LBCHP’s women served are from rural areas. In contrast, 61% of the state is urban, while 72% of LBCHP’s women served live in urban areas. Other than the one region with a negligible rural population (less than 2%), LBCHP inadequately serves the rural areas. It is difficult to reach the small populations that live in the larger rural areas; 11 (of 64) parishes that are more than 80% rural represent only 4% of the eligible population.
Quality of cancer screening and follow-up care
As an early detection program, LBCHP serves women from screening to the start of treatment, if needed. Women may begin services at screening, but they also may enroll in the program after screening in order to receive diagnostic follow-up for abnormal screening results or symptoms. A higher proportion of clients had abnormal screening results for mammograms (32%) than for Pap tests (2%). The high mammogram abnormality rate is likely caused by several factors: women are referred to LBCHP after abnormal screenings or with symptoms, rarely or never before screened women typically have higher rates of abnormalities and mammograms routinely have higher abnormality rates than Pap tests. The mammogram results are presented in Table 1. All racial/ethnic groups had excellent follow-up rates for abnormal results, and they were not significantly statistically different by race/ethnicity. The Latinx group had a statistically significantly higher percentage of abnormal results than Blacks and Whites (P<0.0001). Of the 4,007 clients receiving mammograms, 89 were diagnosed with breast cancer, and of the 1,439 receiving Pap tests, 22 were diagnosed with cervical cancer.
Table 1
| Test results | White | Black | Latinx | Total |
|---|---|---|---|---|
| Number of mammograms | 1,488 | 1,466 | 767 | 4,007 |
| Number of abnormal results | 501 | 400 | 325 | 1297 |
| Percentage of abnormal results | 33.7% | 27.3% | 42.4%† | 32.4% |
| Number of abnormalities with complete follow-up | 490 | 396 | 323 | 1,276 |
| % of abnormalities with complete follow-up | 97.8% | 99.0% | 99.4% | 98.4% |
†, statistically significantly higher than Black and White percentages at P<0.0001.
Barriers to be addressed
Table 2 summarizes the reported barriers by race/ethnicity and geographic location. Overall being uninsured and needing information were the most frequent categories of barriers. Black and rural women expressed more concern over appointment times and long waits while the majority of Latinx women expressed concern over lack of insurance and not being able to speak English.
Table 2
| Barriers | Race/ethnicity | Geographic location | ||||||
|---|---|---|---|---|---|---|---|---|
| White | Black | Latinx | Total | Rural | Urban | Total | ||
| Uninsured, % | 42 | 28 | 94 | 49 | 24 | 53 | 48 | |
| Need information (e.g., screening, testing), % | 32 | 31 | 44 | 37 | 22 | 39 | 36 | |
| Limited or inflexible appointment times, % | 33 | 45 | 5 | 32 | 47 | 25 | 28 | |
| Long wait times, % | 29 | 44 | 2 | 29 | 44 | 23 | 26 | |
| Financial distress (not insurance related), % | 29 | 19 | 2 | 18 | 37 | 19 | 21 | |
| Non-English speaking, % | <1 | 1 | 62 | 12 | 1 | 16 | 14 | |
Discussion
We undertook this work to explore to what extent LBCHP had been reaching women targeted as most in need of patient navigation services, as well as reducing health inequities (3). By using existing public data sources to estimate the numbers and proportions of women who meet LBCHP’s eligibility criteria, and comparing these data with LBCHP services data, we were able to estimate the number of women who qualify for LBCHP services [641,600], and determine how well we are reaching specific subpopulations by parish (county) and region. The large number of women who qualify for LBCHP services, almost half of the women in this age group, reflects the overall poverty level of the state; Louisiana has one of the highest percentages of population living in poverty (100% FPL) in the US (17).
The results indicate that the program is indeed reaching low-income women within the two largest racial/ethnic minority populations in the state: Black and Latinx. Black women are being served in proportion to their presence in the population, and the percentage of LBCHP patient navigation recipients is even higher than the percentage of low-income Latinx women in the state. LBCHP has more providers in heavily populated areas, and according to this analysis, Latinxs are more likely to live in those areas, which may contribute to this finding. Conversely, the program is not succeeding as well at reaching eligible participants in rural areas. When the program began in 2002, LBCHP focused on providing clinical services in population centers in order to reach more women given limited funding. There will continue to be tension between keeping the per woman cost low, and providing services equitably. However, now that more women have coverage for clinical services due to Medicaid expansion, and this analysis demonstrates that we are not reaching rural women as needed, expanding and tailoring patient navigation to rural areas will now become a priority.
The results also demonstrate that LBCHP is providing successful patient navigation to all women regardless of location and race/ethnicity. All participants had close to 100% timely and complete diagnoses and start of treatment as needed, a key metric for evaluating patient navigation (18). This is consistent with other studies, such as Markossian et al., which demonstrated near 100% diagnostic resolution as compared to 81% resolution for abnormal mammograms and 70% resolution for abnormal Paps, as well as much shorter times to resolution in a navigated arm versus control (19). In comparison, a large national study of facilities serving vulnerable women found that 90.3% of women received follow-up after abnormal mammography and that racial minorities follow-up rates were lower by 5% compared to white populations (20). One of the factors that may contribute to this result is that LBCHP’s patient navigation services are embedded in the health providers that serve potential participants (10). However, as we expand navigation services to reach more women, especially in rural areas with no or few providers, we will explore alternative models of navigation, such as centralized or network-based, that are suited to the local/regional capacity (21).
Additionally, this analysis will inform other LBCHP components to improve how we reach minority and rural women. We will look in underserved parishes with access to LBCHP’s target populations, and engage new clinical and navigation providers. Post Medicaid expansion, LBCHP has been piloting community-based initiatives to navigate women to screening (22), including working with food pantries and navigation to screening; these results will help determine where and how to proceed in a way that will promote health equity.
The lack of a comparison group is another limitation of this study. Our data include only women who received some screening services and navigation. However, the intent was to analyze the distribution of woman served in comparison to the distribution of women in the state. Therefore, the comparisons in this analysis are the state data.
The results indicate that LBCHP has been most effective in reaching Latinx participants. A next step is to do an analysis of this success. While it may be a function of Latinx populations being concentrated in metropolitan areas, there may be other lessons learned that we can use to improve LBCHP’s efforts for other women. Reported barriers clearly differ by group. A future study could focus more on the specific barriers encountered and navigation services among different populations, e.g., among racial/ethnic groups.
A limitation of this analysis is that it is conducted on the parish level; racial/ethnic minority populations do not live evenly spread across each parish. While parish level data is more easily accessed and easier to manage, it does not provide the best information on where potential participants live or would need to travel to access services.
Conclusions
We employed a unique analysis to explore LBCHP’s reach of underserved populations through patient navigation. This analysis demonstrates that through patient navigation, an evidence-based intervention for reducing health inequalities, LBCHP is equitably reaching racial/ethnic minority populations in Louisiana. LBCHP’s largest reach is among the Latinx population. In addition, the quality of patient navigation is equitable across population groups; once clients receive screening, they have excellent follow-up rates for any abnormalities. Because LBCHP’s priorities include serving a high number of women with limited resources, a majority of services were placed in population centers around the state creating an unintended consequence of underserving the rural population.
The results of this analysis will serve as the basis for ongoing, incremental changes in program planning, implementation and evaluation of patient navigation services, as well as other program activities. Having the estimated counts of both the number of women eligible for LBCHP and the number served by parish and race/ethnicity will help the balance between keeping the per woman cost low and providing services equitably in Louisiana.
Acknowledgments
Funding: This work was supported by
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Hui-Yi Lin, Tung-Sung Tseng) for the series “Population Science in Cancer” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.05.26). The series “Population Science in Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All Louisiana Breast and Cervical Health Program (LBCHP) participants gave their informed consent before receiving clinical and navigation services. All personal identifiers have been excluded from this study to protect participants’ privacy.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim S, Molina Y, Glassgow AE, et al. The effects of navigation and types of neighborhoods on timely follow-up of abnormal mammogram among black women. Med Res Arch 2015;2015: [Crossref] [PubMed]
- Roland KB, Milliken EL, Rohan EA, et al. Use of Community Health Workers and Patient Navigators to Improve Cancer Outcomes Among Patients Served by Federally Qualified Health Centers: A Systematic Literature Review. Health Equity 2017;1:61-76. [Crossref] [PubMed]
- Singh GK, Jemal A. Socioeconomic and Racial/Ethnic Disparities in Cancer Mortality, Incidence, and Survival in the United States, 1950-2014: Over Six Decades of Changing Patterns and Widening Inequalities. J Environ Public Health 2017;2017:2819372. [Crossref] [PubMed]
- National Breast and Cervical Cancer Early Detection Program. Program Manual. Available online: https://www.cdc.gov/cancer/nbccedp/index.htm
- History [Internet]. Louisiana Breast & Cervical Health Program. [cited 2019Mar4]. Available online: http://lbchp.org/history
- Norris L. Louisiana and the ACA’s Medicaid Expansion. November 21, 2018. Available online: https://www.healthinsurance.org/louisiana-medicaid/
- NCI Dictionary of Cancer Terms. National Cancer Institute. [cited 2019Mar8]. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/patient-navigator
- Krok-Schoen JL, Oliveri JM, Paskett ED. Cancer Care Delivery and Women's Health: The Role of Patient Navigation. Front Oncol 2016;6:2. [PubMed]
- Dudley DJ, Drake J, Quinlan J, et al. Beneficial effects of a combined navigator/promotora approach for Hispanic women diagnosed with breast abnormalities. Cancer Epidemiol Biomarkers Prev 2012;21:1639-44. [Crossref] [PubMed]
- Inrig SJ, Tiro JA, Melhado TV, et al. Evaluating a De-Centralized Regional Delivery System for Breast Cancer Screening and Patient Navigation for the Rural Underserved. Tex Public Health J 2014;66:25-34. [PubMed]
-
U.S. Department of Health & Human Services, Office of the Assistant Secretary for Planning and Evaluation - Annual Poverty Guidelines, all states (except Alaska and Hawaii). (2019, February 01). Available online: https://aspe.hhs.gov/system/files/aspe-files/107166/2019-pctpovertytool-highlight.xlsx
- Bowers L, Gann C, Upton R. (2018, March). Small Area Health Insurance Estimates: 2016. Available online: https://www.census.gov/content/dam/Census/library/publications/2018/demo/p30-03.pdf
- US Census Bureau. (2018, October 11). American Community Survey Data. Available online: https://www.census.gov/programs-surveys/acs/data.html
- US Census Bureau. (2016, November 01). Summary File 1 Dataset. Available online: https://www.census.gov/data/datasets/2010/dec/summary-file-1.html
- Hospitals by Administrative Region. Health Standards, Louisiana Department of Health. [cited 2019 Mar 8]. Available online: http://ldh.la.gov/index.cfm/page/2665
- Fontenot K, Semega J, Kollar M. Income and poverty in the United States: 2017. Library, United States Census Bureau. [cited 2019 Mar 8]. Available online: https://www.census.gov/library/publications/2018/demo/p60-263.html
- Guadagnolo BA, Dohan D, Raich P. Metrics for evaluating patient navigation during cancer diagnosis and treatment: crafting a policy-relevant research agenda for patient navigation in cancer care. Cancer 2011;117:3565-74. [Crossref] [PubMed]
- Markossian TW, Darnell JS, Calhoun EA. Follow-up and timeliness after an abnormal cancer screening among underserved, urban women in a patient navigation program. Cancer Epidemiol Biomarkers Prev 2012;21:1691-700. [Crossref] [PubMed]
- Goldman LE, Walker R, Hubbard R, et al. Timeliness of abnormal screening and diagnostic mammography follow-up at facilities serving vulnerable women. Med Care 2013;51:307-14. [Crossref] [PubMed]
- Inrig SJ, Higashi RT, Tiro JA, et al. Assessing local capacity to expand rural breast cancer screening and patient navigation: An iterative mixed-method tool. Eval Program Plann 2017;61:113-24. [Crossref] [PubMed]
- Phillips CE, Rothstein JD, Beaver K, et al. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med 2011;26:123-9. [Crossref] [PubMed]


