
Albumin-bilirubin grade as a prognostic factor of hepatocellular carcinoma after treatment with orthotopic liver transplantation
Introduction
Hepatocellular carcinoma (HCC) represents the sixth most common malignancy and the second leading cause of cancer-related deaths worldwide (1). Currently, the therapeutic tools for HCC include surgery, radiofrequency ablation, chemotherapy, and targeted cancer therapy, with diversified treatment patterns. Meanwhile, orthotopic liver transplantation (OLT) still represents the best tool predicting long-term survival in the treatment of liver malignancy. Clinical prognosis and therapeutic options in HCC after OLT widely depend on both tumor recurrence and hepatic function (2,3). Currently, tumor size, histological grade of differentiation, microvascular and macrovascular invasion, ischemia time, and some related genes are prognostic factors after OLT in patients with HCC (4-7). Factors impacting hepatocyte regeneration and proliferation, such as IL-6 (8) and TLR-4 (9), are associated with tacrolimus metabolism in early stage after transplantation, which may markedly influence patient prognosis after OLT (10). However, studies assessing the association of hepatic function grade standards with prognosis after OLT are scarce.
The Child-Pugh (C-P) grade is the most commonly used measure for the assessment of hepatic function and patient selection for OLT (11). Nevertheless, the use of interrelated and subjective variables, such as ascites and encephalopathy, limits the prognostic ability of this liver function indicator, particularly in patients with HCC. In 2015, Johnson proposed an objective measure to assess liver function, namely the albumin-bilirubin (ALBI) grade. This evidence-based model is solely based on serum bilirubin and albumin, which could help clinicians obtain a more objective scale that guides disease diagnosis and treatment (12). Since then, the ALBI grade has been shown to have better performance for assessing hepatic function in HCC patients compared with the C-P grade (13-16). Especially, the ALBI grade has been reported as a prognostic factor in independent studies involving tumor resection (13), stereotactic ablative radiation therapy (14), sorafenib therapy (15), and acute-on-chronic liver failure (16). However, it has been rarely assessed in HCC patients undergoing OLT. Hepatic function is one of the critical indicators in assessing the surgical risk before transplantation; furthermore, its restoration is the main process taking place after liver transplantation. Thus, we hypothesized that the ALBI grade may affect patient prognosis after OLT in HCC.
The primary aim of the present study was to assess the ALBI grade, as a practical and potentially effective clinical marker for determining prognosis after OLT in patients with HCC.
Methods
Patients
All HCC patients treated by OLT in the Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine, between September 2007 and June 2012, were enrolled in this retrospective study. A total of 75 patients with HCC were included. Inclusion criteria for transplantation patients were: age ≥18 years; compatible blood and tissue type with respective donors; no macrovascular invasion or extrahepatic metastasis; and no history of other malignant tumors; no other grafts or organ dysfunction; complete follow-up records. All the patients were Han Chinese.
Laboratory parameters and follow-up
Venous blood samples were collected right before OLT. Alanine aminotransferase (ALT), aspartate transaminase (AST), total bilirubin, alkaline phosphatase, serum albumin, total protein, creatinine, and other biochemical indicators were assessed with specific ELISA kits, according to the manufacturer’s instructions. The C-P score was derived from five variables, including serum total bilirubin, albumin concentration, prothrombin time, ascites status, and the degree of encephalopathy. Based on the C-P score, the patients were classified into the following 3 groups: grade A (score ≤6); grade B (6< score ≤9); grade C (>9) (11). The ALBI score was calculated by the following formula: ALBI score =0.66×log10 [total bilirubin (µmol/L)] − 0.085× [albumin (g/L)]. According to the ALBI score, the patients are categorized into grade 1 (score ≤−2.60), grade 2 (−2.60< score ≤−1.39), and grade 3 (score >−1.39), respectively (12). The patients were followed up right after hospital discharge, every week within 3 months of OLT, and every month thereafter by telephone, email, or hospital visit. Follow-up occurred for at least 100 months or until patient death.
Statistical analysis
All statistical analyses were performed with SPSS v20.0 (SPSS, USA). Non-normally distributed continuous variables were compared by nonparametric tests, and presented as median and interquartile range. Categorical variables were expressed as absolute and relative frequencies, and compared by the chi-squared test. Survival analyses were performed using the log-rank test and Cox regression. Survival was described as mean and 95% confidence interval (CI). Multivariate logistic regression analyses were used to assess the factors associated with HCC recurrence. Two-sided P<0.05 was considered statistically significant.
Results
Clinical characteristics of the enrolled patients
The Clinical characteristics of all enrolled HCC patients are summarized in Table 1. The 75 liver transplantations performed in the Shanghai General Hospital involved 65 men and 10 women, with a median age of 50 years (range, 45–56 years). Median total bilirubin at the time of transplantation was 18.20 µmol/L (range, 12.50–43.63), while a median albumin of 40.10 g/L (range, 35.21–44.17) was obtained. The majority (92.0%) of patients had hepatitis B virus infection, and cirrhosis occurred in 64 (85.3%) individuals. The median ALBI score was −2.68 (range, −2.93 to −1.76); 64.0% (48/75), 24.0% (18/75), and 12.0% (9/75) of the patients were categorized into grades 1, 2 and 3, respectively. Most patients with ALBI grade 1 (26/48) had a C-P grade A, while the remaining patients had grade B. Meanwhile, 66.7% (12/18) of patients with ALBI grade 2 were stratified into C-P grade A, with the remaining into grade B. Only 1 (11.1%) patient with ALBI grade 3 was classified as C-P grade A, 4 were classified as grade B, the remaining were classified as grade C. There was a significant correlation between ALBI grade and C-P score (R2 =0.119, P=0.002, date not shown) (14). A total of 27 (36.0%) patients showed HCC recurrence after OLT, and 23 (30.7%) died during follow-up.
Table 1
| Factors | Statistical description |
|---|---|
| Age (years) | 50 (IQR: 45–56) |
| Sex (male/female) | 65/10 |
| Total bilirubin, μmol/L | 18.20 (IQR: 12.50–43.63) |
| Albumin, g/L | 40.10 (IQR: 35.21–44.17) |
| Cirrhosis (yes/no) | 64/11 |
| HBV infection (yes/no) | 69/6 |
| AFP (≤400/>400) ng/mL | 53/22 |
| Tumor size (≤5/>5) cm | 48/27 |
| Child-Pugh score (A/B/C) | 39/32/4 |
| ALBI grade (1/2/3) | 48/18/9 |
| TNM stage (1–2/3–4) | 52/23 |
| Milan criteria (out/in) | 41/34 |
| Microvascular invasion (yes/no) | 14/61 |
| Recurrence/nonrecurrence | 27/48 |
| Death (no/yes) | 52/23 |
HBV, hepatitis B virus; AFP, alpha-fetoprotein; IQR, interquartile range; Child-Pugh score A/B/C, 5–6/7–9/≥10; ALBI, albumin-bilirubin; TNM, tumor node metastasis.
Log-rank and Cox regression analyses
Clinical characteristics and their associations with overall survival (OS) and recurrence-free survival (RFS) are shown in Table 2. The Kaplan-Meier test was performed to analyze the associations of the eleven parameters with OS and RFS. As shown in Table 2, tumor size, ALBI grade, TNM stage, Milan criteria, and microvascular invasion were significantly associated with OS and RFS. The ALBI scale revealed 3 classes with different prognoses in patients treated with OLT. Patients with ALBI grade 1 had a survival advantage over ALBI grade 2 and 3 individuals (P=0.018), with mean survival time of 37.03 months (95% CI: 30.77–43.30) versus 32.31 months (95% CI: 23.88–40.75) and 14.27 months (95% CI: 9.38–19.16) for grades 2 and 3, respectively. Meanwhile, significant differences in RFS were also observed among ALBI grades (P=0.021). Mean RFS times in patients with ALBI grades 1 to 3 were 33.95 months (95% CI: 27.28–40.63), 26.88 months (95% CI: 16.28–37.48), and 9.69 months (95% CI: 3.71–15.66), respectively.
Table 2
| Factors | OS | RFS | |||
|---|---|---|---|---|---|
| χ2 value | P value | χ2 value | P value | ||
| Recipient age (≤50/>50) | 0.983 | 0.321 | 1.075 | 0.300 | |
| Sex (male/female) | 0.001 | 0.982 | 0.013 | 0.908 | |
| Cirrhosis (no/yes) | 0.124 | 0.725 | 0.397 | 0.529 | |
| HBV infection (no/yes) | 0.001 | 0.991 | 0.135 | 0.713 | |
| AFP (≤400/>400) ng/mL | 0.687 | 0.407 | 0.429 | 0.513 | |
| Child-Pugh score (A/B/C) | 4.150 | 0.126 | 2.546 | 0.280 | |
| Tumor size (≤5/>5) cm | 8.140 | 0.004 | 9.052 | 0.003 | |
| ALBI grade (1/2/3) | 8.007 | 0.018 | 7.713 | 0.021 | |
| TNM stage (1–2/3–4) | 28.046 | <0.001 | 26.067 | <0.001 | |
| Milan criteria (out/in) | 12.643 | <0.001 | 13.968 | <0.001 | |
| Microvascular invasion (yes/no) | 15.757 | <0.001 | 13.490 | <0.001 | |
HBV, hepatitis B virus; AFP, alpha-fetoprotein; Child-Pugh score A/B/C, 5–6/7–9/≥10; ALBI, albumin-bilirubin; TNM, tumor node metastasis.
Next, factors with corresponding P<0.05 in the univariate analysis were introduced into Cox proportional hazard regression analysis to further assess risk factors for OLT, and ALBI grade (P=0.022 and P=0.019, respectively) persisted as a statistically significant independent prognostic factor of both OS and RFS. Meanwhile, TNM stage was an independent predictor of OS (P=0.039); microvascular invasion stage remained a prognostic factor of RFS (P=0.042) (Table 3). According to previous findings (13-16), ALBI grade (grade 1 vs. grades 2–3) were subjected to Kaplan-Meier test and Cox proportional hazard regression analysis. In agreement with the above findings, patients with ALBI grade 1 had a survival advantage over those with other grades (Figure 1); ALBI grade 1 remained significant in predicting post-operative OS and RFS in HCC patients who underwent OLT [HR =3.095 (1.290–7.426), P=0.011; HR =3.967 (1.640–9.597), P=0.002, respectively] (Table 4).
Table 3
| Factors | Hazard ratio (95% CI) | P value |
|---|---|---|
| OS | ||
| ALBI grade (1/2/3) | 1.927 (1.099–3.378) | 0.022 |
| TNM stage (stage 1–2, stage 3–4) | 4.011 (1.074–14.975) | 0.039 |
| Tumor size (≤5/>5) | 0.761 (0.253–2.294) | 0.628 |
| Milan criteria (out/in) | 1.427 (0.473–4.312) | 0.528 |
| Microvascular invasion (yes/no) | 0.324 (0.089–1.180) | 0.087 |
| RFS | ||
| ALBI grade (1/2/3) | 1.844 (1.104–3.078) | 0.019 |
| Microvascular invasion (yes/no) | 0.270 (0.077–0.954) | 0.042 |
| TNM stage (1–2/3–4) | 3.472 (0.915–13.181) | 0.067 |
| Tumor size (≤5/>5) | 0.862 (0.286–2.601) | 0.792 |
| Milan criteria (out/in) | 1.325 (0.446–3.938) | 0.613 |
CI, confidence interval; ALBI, albumin-bilirubin; TNM, tumor node metastasis.
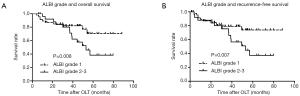
Table 4
| Factors | Hazard ratio (95% CI) | P value |
|---|---|---|
| OS | ||
| ALBI grade (1/2–3) | 3.095 (1.290–7.426) | 0.011 |
| TNM stage (1–2/3–4) | 3.991 (1.002–15.889) | 0.049 |
| Microvascular invasion (yes/no) | 0.306 (0.083–1.130) | 0.076 |
| Tumor size (≤5/>5 cm) | 0.738 (0.234–2.327) | 0.605 |
| Milan criteria (out/in) | 1.582 (0.530–4.717) | 0.411 |
| RFS | ||
| ALBI grade (1/2–3) | 3.967 (1.640–9.597) | 0.002 |
| TNM stage (1–2/3–4) | 4.056 (1.011–16.271) | 0.048 |
| Microvascular invasion (yes/no) | 0.234 (0.065–0.840) | 0.026 |
| Tumor size (≤5/>5 cm) | 0.856 (0.273–2.686) | 0.790 |
| Milan criteria (out/in) | 1.243 (0.412–3.751) | 0.699 |
CI, confidence interval; ALBI, albumin-bilirubin; TNM, tumor node metastasis.
Risk factors for recurrence
The prognostic value of the ALBI grade was further assessed for survival, especially RFS. Another test including the above eleven parameters revealed that tumor size (≤5 cm), low ALBI grade, TNM stage [1–2], inclusion by Milan criteria, and no microvascular invasion were found in patients with low probability of HCC recurrence after OLT, generally in agreement with previous studies (4-7). The clinical characteristics and their associations with HCC recurrence are presented in Table 5. To further elucidate the impact of ALBI grade on tumor recurrence, all the above parameters were subjected to multivariate logistic regression analysis. As shown in Table 5, ALBI grade (grade 1 vs. grades 2–3) and Milan criteria (out vs. in) were correlated with HCC recurrence [OR =6.842 (1.550–30.199), P=0.011; OR =0.084 (0.015–0.490), P=0.006, respectively] (Table 6).
Table 5
| Factors | Nonrecurrence group (n=48) | Recurrence group (n=27) | P value |
|---|---|---|---|
| Age (year) | |||
| ≤50 | 29 (64.4) | 16 (35.6) | 0.922 |
| >50 | 19 (63.3) | 11 (36.7) | |
| Sex | |||
| Male | 40 (61.5) | 25 (38.5) | 0.258 |
| Female | 8 (80.0) | 2 (20.0) | |
| Cirrhosis | |||
| Yes | 43 (67.2) | 21 (32.8) | 0.165 |
| No | 5 (45.5) | 6 (54.5) | |
| HBV infection | |||
| Yes | 46 (66.7) | 23 (33.3) | 0.180 |
| No | 2 (33.3) | 4 (66.7) | |
| AFP (ng/mL) | |||
| ≤400 | 34 (64.2) | 19 (35.8) | 0.966 |
| >400 | 14 (63.6) | 8 (36.4) | |
| Tumor size (cm) | |||
| ≤5 | 38 (79.2) | 10 (20.8) | <0.001 |
| >5 | 10 (37.0) | 17 (63.0) | |
| Child-Pugh score | |||
| A | 26 (66.7) | 13 (33.3) | 0.417 |
| B | 21 (65.6) | 11 (34.4) | |
| C | 1 (25.0) | 3 (75.0) | |
| ALBI grade | |||
| 1 | 35 (72.9) | 13 (27.1) | 0.020 |
| 2 | 10 (55.6) | 8 (44.4) | |
| 3 | 3 (33.3) | 6 (66.7) | |
| TNM | |||
| 1–2 | 42 (80.8) | 10 (19.2) | <0.001 |
| 3–4 | 6 (26.1) | 17 (73.9) | |
| Milan criteria | |||
| Out | 17 (41.5) | 24 (58.5) | <0.001 |
| In | 31 (91.2) | 3 (8.8) | |
| Microvascular invasion | |||
| No | 44 (72.1) | 17 (27.9) | 0.002 |
| Yes | 4 (28.6) | 10 (71.4) |
HCC, Hepatocellular carcinoma; HBV, hepatitis B virus; AFP, alpha-fetoprotein; Child-Pugh score A/B/C, 5–6/7–9/≥10; ALBI, albumin-bilirubin; TNM, tumor node metastasis.
Table 6
| Factors | Odds ratio (95% CI) | P value |
|---|---|---|
| Milan criteria (out/in) | 0.084 (0.015–0.490) | 0.006 |
| ALBI grade (1/2–3) | 6.842 (1.550–30.199) | 0.011 |
HCC, hepatocellular carcinoma; CI, confidence interval; ALBI, albumin-bilirubin.
Discussion
The patient’s systemic condition and residual liver function should be evaluated comprehensively before the operation, which could help patients with surgical and postoperative treatments. To date, several scoring systems have been proposed to evaluate liver function and predict the outcome of patients with liver disease; these include the Japan Integrated Stage score (17) and C-P (11) scales. However, unforeseeable complications remain after liver transplantation. How to improve patient prognosis is currently a major research hotspot. Recently, some clinical manifestations and gene mechanisms were shown to be related to post-transplantation prognosis and recurrence. Indeed, tumor size and number, histological grade of differentiation, microvascular and macrovascular invasion, ischemia time, SMO and the C6 genotype are associated with postoperative prognosis and recurrence after OLT (2-7,18). However, these factors require invasive or noninvasive assays, which are expensive and/or intolerable. The ALBI-grade, which is derived from only albumin and total-bilirubin measurements, compared with those mentioned above, is a more objective and effective scoring system. In the current study, we demonstrated the value of ALBI grade in predicting post-operative OS and RFS in HCC patients who underwent OLT.
Human serum albumin, synthesized predominantly in the liver as an abundant multifunctional non-glycosylated, negatively charged plasma protein, has an indispensable role in antioxidant functions and enzymatic activities, with ascribed ligand-binding and transport properties (19). Ischemia-reperfusion injury caused by hypoxia/reoxygenation in the liver is a major event during liver transplantation and failure, which inevitably causes liver damage and inflammatory reactions, promotes lipid peroxidation, and stimulates reactive oxygen species (ROS) production (20-22). Meanwhile, albumin was reported to protect against ischemia-reperfusion injury. Restoring the extracellular thiol status, scavenging neutrophil-derived ROS, modifying redox balance, regulating cell signaling, transporting antioxidative substances, and inhibiting TNF-α-induced upregulation of VCAM-1 and NF-KB activation were reported to help normal cells escape inflammation and oxidative stress related damage (23-28). According to Yamaguchi, heme oxygenase-1 gene and protein upregulation by ischemia-reperfusion of the liver may enhance the production of bilirubin, which acts as a scavenger via its own oxidation to sequester ROS, with a protective effect against oxidative stress (29). Although, studies of albumin and bilirubin in patients with liver disease have led to encouraging results, the potential role of effective albumin levels and physiological bilirubin amounts in inflammatory and oxidative stress damage remain unclear (30). As shown above, patients with ALBI grade (merely from albumin and bilirubin levels) 1 had a survival advantage over those of ALBI grades 2 and 3. The severity of early incidents during OLT is the most vital event for patient outcome (10). Thus, we hypothesized that initial albumin and bilirubin amounts might play an important role at this unique moment, and improved hepatic function could lead to better prognosis.
In the current study, we confirmed the value of the ALBI grade in predicting post-operative OS in HCC patients who underwent OLT. To date, Zou (13) and Wang (31) have reported that the ALBI grade is associated with post-operative outcomes in HCC patients after hepatectomy, with a better predictive value than the C-P grade; this was also confirmed in stereotactic ablative radiation therapy, sorafenib therapy, or acute-on-chronic liver failure (14-16). These findings were consistent with the present study. However, there was no means to verify that the ALBI grade was associated with HCC recurrence. In the current study cohort, 13 (27.1%), 8 (44.4%), and 6 (66.7%) patients with ALBI grades 1, 2, and 3, respectively, experienced HCC recurrence after OLT (P=0.020). Mean times to recurrence were 10.87 months (95% CI: 4.62–17.13), 9.03 months (95% CI: 1.85–16.20), and 5.76 months (95% CI: 1.31–11.48) for ALBI grades 1–3, respectively, indicating no significant differences (P=0.664). However, the ALBI grade clearly showed a tendency in estimating time to recurrence. In addition, 10 (20.8%) patients with ALBI grade 1, 9 (50.0%) with ALBI grade 2, and 4 (44.4%) with ALBI grade 3 died during follow up (P=0.048); patients with ALBI grade 1 had a better outcome than those with other grades. These findings suggested that a low ALBI grade does not delay HCC recurrence, but may decrease the incidence of HCC recurrence and help the patient against tumor cells, thereby leading to improved outcome. Moreover, preoperative albumin and bilirubin would play an important role in ischemia time, which has been demonstrated as a recurrence factor (3). Tumor recurrence is a major and potentially fatal challenge after OLT for HCC, with a fairly complicated underlying mechanism (32). Nonetheless, the patient’s basic hepatic function status, described by the ALBI grade, undisputedly has an irreplaceable value.
The limitations of this study should be mentioned. Firstly, the sample size was relatively small, and all subjects were Chinese Han enrolled from a single center. Secondly, the majority of patients were infected with HBV; therefore, regional differences in viral infection may affect the possible correlation between the ALBI grade and prognosis after OLT. Thirdly, the ALBI grade was not dynamically monitored; ALBI grade change during the perioperative period may produce different results. Fourthly, postoperative complications and effective related proteins were not currently included in the analysis. To validate these data, studies with larger patient cohorts in multiple centers and different regions are required. Besides, continuous monitoring of the ALBI grade is one of the main directions of future research.
Conclusions
Overall, in patients with HCC undergoing OLT, ALBI grade 1 results in higher OS, increased RFS and lower risk of recurrence. These novel findings indicate that the ALBI grade represents an independent marker of prognosis following OLT for HCC; improving the preoperative liver function status may improve the prognosis of patients with HCC after OLT.
Acknowledgments
We thank the native English speaking editors at MedSci (www.medsci.cn) for editing the manuscript.
Funding: This study was partly supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.07.52). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional review board of Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine (No. 2013KY050). The procedures were performed based on strict guidelines from the ethics committee of the hospital, following the current regulations of the Chinese Government as well as the Declaration of Helsinki (as revised in 2013). Informed consent was waived because this study consisted of a retrospective review of existing records without any direct patient contact. The research ethics board considered this a minimal risk study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. Ca Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Wang Z, Liao J, Wu S, et al. Recipient C6 rs9200 genotype is associated with hepatocellular carcinoma recurrence after orthotopic liver transplantation in a Han Chinese population. Cancer Gene Ther 2016;23:157-61. [Crossref] [PubMed]
- Nagai S, Yoshida A, Facciuto M, et al. Ischemia time impacts recurrence of hepatocellular carcinoma following liver transplantation. Hepatology 2015;61:895-904. [Crossref] [PubMed]
- Sumie S, Kuromatsu R, Okuda K, et al. Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors. Ann Surg Oncol 2008;15:1375-82. [Crossref] [PubMed]
- Parfitt JR, Marotta P, Alghamdi M, et al. Recurrent hepatocellular carcinoma after transplantation: Use of a pathological score on explanted livers to predict recurrence. Liver Transpl 2007;13:543-51. [Crossref] [PubMed]
- Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol 2009;10:35-43. [Crossref] [PubMed]
- Xu X, Ling Q, Wang J, et al. Donor miR-196a-2 polymorphism is associated with hepatocellular carcinoma recurrence after liver transplantation in a Han Chinese population. Int J Cancer 2016;138:620-9. [Crossref] [PubMed]
- Chen D, Fan J, Guo F, et al. Novel single nucleotide polymorphisms in interleukin 6 affect tacrolimus metabolism in liver transplant patients. PLoS One 2013;8:e73405. [Crossref] [PubMed]
- Wang Z, Wu S, Chen D, et al. Influence of TLR4 rs1927907 locus polymorphisms on tacrolimus pharmacokinetics in the early stage after liver transplantation. Eur J Clin Pharmacol 2014;70:925-31. [Crossref] [PubMed]
- Aidong W, Zhenjie C, Tong L, et al. Therapeutic drug monitoring of tacrolimus in early stage after heart transplantation. Transplant Proc 2004;36:2388-9. [Crossref] [PubMed]
- Durand F, Valla D. Assessment of prognosis of cirrhosis. Semin Liver Dis 2008;28:110-22. [Crossref] [PubMed]
- Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of Liver Function in Patients With Hepatocellular Carcinoma: A New Evidence-Based Approach—The ALBI Grade. J Clin Oncol 2015;33:550-8. [Crossref] [PubMed]
- Zou H, Wen Y, Yuan K, et al. Combining albumin-bilirubin score with future liver remnant predicts posthepatectomy liver failure in HBV-associated HCC patients. Liver Int 2018;38:494-502. [Crossref] [PubMed]
- Lo CH, Liu MY, Lee MS, et al. Comparison Between Child-Turcotte-Pugh and Albumin-Bilirubin Scores in Assessing the Prognosis of Hepatocellular Carcinoma After Stereotactic Ablative Radiation Therapy. Int J Radiat Oncol Biol Phys 2017;99:145-52. [Crossref] [PubMed]
- Lee PC, Chen YT, Chao Y, et al. Validation of the ALBI Grade-based Integrated Model as a Predictor for Sorafenib-failed Hepatocellular Carcinoma. Liver Int 2018;38:321-30. [Crossref] [PubMed]
- Chen B, Lin S. Albumin-bilirubin (ALBI) score at admission predicts possible outcomes in patients with acute-on-chronic liver failure. Medicine 2017;96:e7142. [Crossref] [PubMed]
- Ikai I, Takayasu K, Omata M, et al. A modified Japan Integrated Stage score for prognostic assessment in patients with hepatocellular carcinoma. J Gastroenterol 2006;41:884-92. [Crossref] [PubMed]
- Wang P, Song W, Li H, et al. Association between donor and recipient smoothened gene polymorphisms and the risk of hepatocellular carcinoma recurrence following orthotopic liver transplantation in a Han Chinese population. Tumour Biol 2015;36:7807-15. [Crossref] [PubMed]
- Azzazy HME, Christenson RH. All About Albumin: Biochemistry, Genetics, and Medical Applications. AACC Inc., 1997:43(10).
- Jaeschke H, Schini VB, Farhood A. Role of nitric oxide in the oxidant stress during ischemia/reperfusion injury of the liver. Life Sci 1992;50:1797-804. [Crossref] [PubMed]
- Pringle JH. Notes on the arrest of hepatic haemorrhage due to trauma. Ann Surg 1908;48:541-9. [Crossref] [PubMed]
- Radi R, Bush KM, Cosgrove TP, et al. Reaction of xanthine oxidase-derived oxidants with lipid and protein of human plasma. Arch Biochem Biophys 1991;286:117-25. [Crossref] [PubMed]
- Quinlan GJ, Margarson MP, Mumby S, et al. Administration of albumin to patients with sepsis syndrome: a possible beneficial role in plasma thiol repletion. Clin Sci 1998;95:459-65. [Crossref] [PubMed]
- Kouoh F, Gressier B, Luyckx M, et al. Antioxidant properties of albumin: effect on oxidative metabolism of human neutrophil granulocytes. Farmaco 1999;54:695-9. [Crossref] [PubMed]
- Quinlan GJ, Martin GS, Evans TW. Albumin: biochemical properties and therapeutic potential. Hepatology 2005;41:1211-9. [Crossref] [PubMed]
- Rubbo H, Parthasarathy S, Barnes S, et al. Nitric oxide inhibition of lipoxygenase-dependent liposome and low-density lipoprotein oxidation: termination of radical chain propagation reactions and formation of nitrogen-containing oxidized lipid derivatives. Arch Biochem Biophys 1995;324:15-25. [Crossref] [PubMed]
- Stocker R, Glazer AN, Ames BN. Antioxidant activity of albumin-bound bilirubin. Proc Natl Acad Sci USA 1987;84:5918-22. [Crossref] [PubMed]
- Zhang WJ, Frei B. Albumin selectively inhibits TNF alpha-induced expression of vascular cell adhesion molecule-1 in human aortic endothelial cells. Cardiovasc Res 2002;55:820-9. [Crossref] [PubMed]
- Yamaguchi T, Terakado M, Horio F, et al. Role of bilirubin as an antioxidant in an ischemia-reperfusion of rat liver and induction of heme oxygenase. Biochem Biophys Res Commun 1996;223:129-35. [Crossref] [PubMed]
- Garcia-Martinez R, Caraceni P, Bernardi M, et al. Albumin: Pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology 2013;58:1836-46. [Crossref] [PubMed]
- Wang YY, Zhong JH, Su ZY, et al. Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg 2016;103:725-34. [Crossref] [PubMed]
- Zimmerman MA, Ghobrial RM, Tong MJ, et al. Recurrence of hepatocellular carcinoma following liver transplantation: a review of preoperative and postoperative prognostic indicators. Arch Surg 2008;143:182-8. [Crossref] [PubMed]


