
Palliative care access in the elderly metastatic breast cancer population: obstacles and opportunities
Metastatic breast cancer: incidence and natural historyOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
Breast cancer is the common cancer diagnosed and the second leading cause of cancer deaths in women. For the year 2019, it is estimated that about 271,270 new cases of breast cancer will be diagnosed in the United States. Although breast cancer mortality has declined by 40% through the years 1989 to 2016, about 42,360 deaths will likely occur due to breast cancer alone in the United States for the year 2019 (1). Due to wide heterogeneity of the disease, the natural course of breast cancer and outcome with treatment is variable. Early stages of diagnosis lead to better prognosis and cure from existing treatments, with risk for relapse based on clinical and molecular risk factors (2). About 5–10% of patients have metastatic disease at initial diagnosis who are incurable, except when the presentation involves one or few metastatic sites (3). Progression free survival (PFS) and overall survival (OS) have improved with newer combination systemic therapies for specific subgroups, but overall long term survival is still poor with only about 20% of patients with metastatic breast cancer (MBC) surviving at 5 years (4). Among MBC patients, those with high tumor burden and visceral disease respond poorly to treatment and those with multiple brain metastatic disease and triple negative breast cancer (TNBC) experience inferior survival (5). Molecular subtype of the tumor along with sites of metastatic disease affects response to treatment and survival (2,6). Traditionally, the overall the median survival of metastatic hormone receptor positive breast cancer patients with bone only disease is reported around 9 years (7). Survival among this group of patients may be further improved by utilizing combination biologic therapies with endocrine treatment upfront. In this regard, initial therapy with palbociclib and letrozole demonstrated improved progression free survival with continued maintenance of benefit along subsequent lines of therapy which also delayed the use of chemotherapy (40.4 vs. 29.9 months, palbociclib and letrozole arm vs. letrozole only arm) (8,9). As combination therapy is increasingly used in metastatic breast cancer patients, side effects from therapy as well as adverse events will increase as well. Further, with a natural history of years for most metastatic breast cancer patients, many patients are living with metastatic breast cancer who would potentially benefit from long-term palliative care. Elderly metastatic breast cancer patients have a worse breast cancer specific survival, suggesting barriers to care and potentially worse symptoms during their course of disease (10).
Symptoms in metastatic breast cancer and role of palliative careOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
The physical symptoms that patients with metastatic breast cancer experience largely depend upon the location to which the cancer has spread and the type of tissue the growth invades. Further, the types of systemic therapy utilized to control the disease carry their own set of unique symptoms depending on the drugs utilized. In addition to physical symptoms, patients typically experience substantial symptoms regarding their psychological well-being—each set of symptoms can exacerbate the other (11). By far, the most common physical symptom experienced by patients is pain. Pain is often the first indicator of a problem (12). The most common sites of breast cancer metastases are bone, brain, liver and lung.
Bone is by far the most common site of breast cancer metastases. These bony metastases are often associated with skeletal-related events (SRE), including pathological fractures and breaks; spinal cord compression; bone pain that can be severe and progressive; as well as hypercalcemia. Bone metastasis can also invade the bone marrow, leading to anemia, fatigue, weakness and dyspnea. White blood cells could also be affected, leaving the patient more susceptible to infections. All these sequelae can lead to decreases in mobility and an overall reduction in quality of life (13). Spinal cord compression is one SRE in which radiotherapy is particularly effective, along with surgical decompression and stabilization (14). In addition to these treatments, opioid analgesic therapy will most likely also be needed for most patients with severe or chronic pain (11).
Liver metastases generally do not cause any symptoms in the early stage, however, as the cancer advances it can cause abnormally high liver enzymes, jaundice, pruritis, skin rashes, peripheral edema, abdominal pain, appetite loss, and other gastrointestinal issues (15).
Brain metastases are more common in HER2-positive and triple-negative breast cancer patients. Common symptoms associated with brain metastases include headache, confusion, new onset seizures, vision disturbances and behavioral and personality changes (15).
Pulmonary metastases, like liver metastases, typically are asymptomatic initially. Patients may eventually experience hemoptysis, persistent cough, dyspnea, chest pain, and other nonspecific symptoms of metastatic cancer (12).
It is important to note that systemic treatment is the norm for metastatic cancer treatment in addition to the organ specific treatments that were discussed previously. Systemic treatment generally involves chemotherapy regimens, immunotherapy, hormonal medical therapy, monoclonal antibodies as well as radiopharmaceutical therapy. Radiation therapy was mentioned in the organ specific treatments and is a very common treatment modality for metastases either on it’s own or in combination with other treatments. Surgery and ablation procedures are particularly useful for isolated lesions or low volume disease. Each of these modalities have their unique sets of side effects that can affect the quality of life of the patient.
Pain management is another important consideration in metastatic disease management. The most commonly used medications for cancer-associated pain include opioids, corticosteroids and nonsteroidal anti-inflammatory drugs. Tumors may cause pain by exerting pressure on nerves; in these cases radiotherapy, chemotherapy or surgery are particularly helpful to reduce tumor size and decrease pain (12). Finally, it is necessary to help address the psychological well-being of patients through treatment of anxiety, depression and existential distress that is often associated with metastatic cancer (11). As patients approach end-of-life, spiritual needs and care for the caregivers are of paramount importance as well. Psychosocial needs and socioeconomic status interact with the ability of patients to seek care and with the quality of life. These also need to be addressed. Management of patients with advanced breast cancer can be challenging and requires a interdisciplinary approach to supportive and palliative care. This enables optimization of quality of life and well-being for patients and their families.
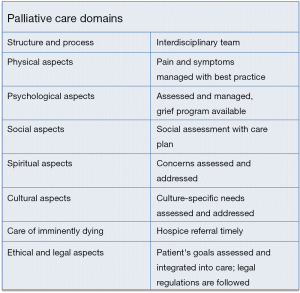
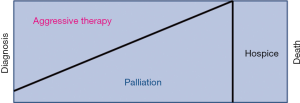
As in Figure 1, palliative care encompasses therapy for the whole individual and takes into account the physical, but as only a portion of the total care. All patients with cancer have needs in these domains. Palliative care requires a multidisciplinary team that includes nursing, social work, nutrition, pastoral care, and providers. Often the needs are least at the beginning of therapy and increase with time, as symptoms increase and psychosocial/spiritual needs increase concomitantly. Figure 2 below shows a typical progression of cancer treatment and symptom needs through the course of a cancer patient’s illness.
Outpatient palliative care and models of careOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
Early outpatient palliative care has shown a survival benefit in metastatic non-small cell lung cancer. Temel et al. demonstrated in a non-blinded, randomized, controlled trial that when early palliative care is integrated into standard oncologic care for metastatic lung cancer patients both quality and quantity of life are improved. This study showed a two-month survival benefit which is similar to the increased quantity of survival many chemotherapeutic drugs confer (16). Similarly, Blackhall et al. at the University of Virginia showed that patients referred to outpatient palliative care within three months prior to death had improved quality of life and decreased healthcare costs. The patients also lived an average of four months longer (17).
Given these findings in lung cancer and advanced cancers of any origin, trials have been completed and are active regarding integration of palliative care into the care of advanced and metastatic breast cancer patients as well. A Yale study “Integrating Palliative Care Into Self-Management of Breast Cancer” evaluated the use of an educational tool to increase patients’ knowledge regarding palliative care to investigate the uptake of palliative care in this group. A prospective, observational study out of Poland is investigating the use of a palliative care intervention for fourteen days and its effect on quality of life in advanced breast cancer patients. Duke University is evaluating via a randomized pilot trial a multi-symptom management protocol targeting distress, pain, and fatigue in women with advanced breast cancer in the United States and Singapore. The University of Michigan is investigating use of an internet-based symptom management intervention in advanced breast cancer (http://clinicaltrials.gov).
These studies are predominantly focusing on palliative interventions that empower both the patient and oncologist to incorporate palliative care early into the patient’s cancer care. This is most useful for uptake into the current healthcare climate, as outpatient palliative care physicians and clinics are sparse. With the realization that early palliative care can be powerful in the overall oncologic management, patients require more visits and more resources from palliative care than in previous models—only inpatient palliative care provided at end-of-life.
Palliative care outpatient physicians are concentrated in large private and academic medical centers. In these large facilities the need for palliative care physicians is larger than the staffing. In community cancer centers, palliative care physicians are often unable to be recruited, as there is an estimated 6,000–18,000 palliative care physician shortage in the inpatient setting alone (17).
Outpatient palliative care services face even more barriers, as palliative care predominantly exists in the inpatient setting. Outpatient palliative care is the early intervention that has shown a survival benefit in metastatic lung cancer. While many oncologists recognize the need for early palliative care, there is a large unmet need, particularly in the community setting. Further, geographic disparities contribute to disparate access to palliative care across the United States (18).
Appalachia and rural America have a paucity of palliative care programs. The Center to Advance Palliative Care Report Card indicated that most states with a grade of C or lower were in the southeast region of the United States. Overall grade for the United States was a B with most of the coastal regions receiving a grade of A. With regard to breast cancer, these are also the regions with a greater delta in breast cancer specific mortality among ethnic groups. Further, these many of these states overlap with a lower uptake of breast cancer screening and more likely to have patients present with metastatic breast cancer and require palliative care (https://statecancerprofiles.cancer.gov/).
Palliative care decreases cost for patients and health care systems and increases value by providing improved quality of life in the setting of decreased costs. It is estimated that if a palliative care team sees 500 patients per year, these savings could net $1.3 million per year (19). Outpatient palliative care could potentially prevent admission to the hospital for these patients with even greater savings for the patient, hospital, and health care system.
However, while palliative care services save the healthcare system costs, they can also negatively impact the revenue of a hospital system. Palliative care requires a multidisciplinary team that includes nursing, social work, nutrition, pastoral care, and providers. These are expensive outpatient ventures focused on quality of life and the patient experience. In a fee-for-service reimbursement model, these benefits are not always attractive to administrators of hospital systems. This impact is greater in cancers with a high incidence and large number of long-term survivors with breast cancer being one of the best examples. Metastatic breast cancer patients potentially require the most outpatient palliative care resources, as this cancer is relatively common and many patients have multi-year survival even in the setting of metastatic disease (https://icer-review.org/wp-content/uploads/2016/03/Palliative-Care-Revised-Draft-Report-030916.pdf).
While leadership from a board certified palliative care physician is optimal, design of a program to harness resources already available at cancer centers with a palliative focus would potentially expand the footprint of palliative care into smaller cancer centers and underserved areas. There is no one best way for oncologists and palliative care specialists to work together, but a few different models have been developed over the years. One method is oncologist-based palliative care where the oncologist assumes the role of coordinating care, providing anti-cancer as well as palliative care services to their patients. The limitations of this model include the palliative care skill level of oncologists, their ability to balance competing interests of care and comfort for patients, as well as the availability of a strong care team for oncologist support (19).
Another successful method that is widely used is a concurrent model in which patients are co-managed by their oncologist as well as a palliative medicine specialist. This is typically an advanced practice nurse specialist with palliative and oncological management experience and education (20). This model is also typically referred to as an integrated or simultaneous care approach (21). These nurse specialists are able to help educate and guide patients through crisis prevention, problem-solving/decision-making skills, symptom management, communication, and advanced care planning. They are also available to patients to help in the coordination of care, specifically with referrals to help improve the patient and caregiver’s quality of living and end of life experiences (20). These nurse specialists are commonly referred to as patient nurse navigators.
This model was measured according to referral rates to social work and palliative care, symptoms, anxiety and overall well-being scores of 118 women with metastatic breast cancer receiving treatment at an urban outpatient breast cancer clinic (22). This study showed that patient navigators have a positive influence on care coordination, physical functioning, financial burden, access to clinical trials and overall improved access to all services (22). The role of patient navigator is found to be most successful when delivered earlier in the metastatic cancer disease trajectory rather than closer to end of life. Earlier intervention provides patients with better access to the resources that will help improve the quality and extend the length of their lives (22). These models of outpatient palliative care can help in the overall care of metastatic and advanced cancer patients and should be able to be adapted to the resources of any cancer care setting.
Unique challenges of metastatic breast cancer in the elderlyOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
Approximately 30% of metastatic breast cancer patients are aged 70 and older. These patients in a SEER analysis have been shown to have inferior breast cancer specific survival. Competing co-morbid conditions, social isolation, socioeconomic factors, family support, and increased likelihood of living in a rural area could all contribute to this survival difference. Approximately 25% of people over 65 years of age and older live in rural areas. The trend for baby boomers has been to move to rural areas with the rural elderly population growing at a rate more quickly than the urban elderly population (10). Access to all healthcare services, but of note palliative care access, is lower in these areas. Palliative care has the power to improve quality of life, but also potentially prolong survival in metastatic cancer populations. Elderly metastatic breast cancer patients have many risk factors and barriers to suggest a lower survival after metastatic breast cancer diagnosis as well as decreased access to palliative care services.
ConclusionsOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
Metastatic breast cancer patients can live many years with metastatic disease. Elderly breast cancer patients have a poorer prognosis and potentially more physical symptoms as well as lower access to palliative care and other healthcare services often due to physical or social isolation. Physical symptoms from the cancer and from systemic therapy agents as well as local therapy side effects can cause significant impact on quality of life. Studies have shown quality of life benefits, more access to services, and improved survival for palliative care in metastatic cancer. Outpatient palliative care access is likely lowest in the elderly metastatic breast cancer patient due to their relatively long survival with the disease, high incidence of the disease, and concentration of the elderly in rural areas where palliative care and healthcare access is low. Harnessing palliative care resources in these areas with nurse navigation as well as use of telemedicine or incentivizing palliative care networks to form with nurse practitioner driven care would be helpful in alleviating this issue and the suffering of this patient population.
AcknowledgmentsOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
Funding: None.
FootnoteOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vincent Vinh-Hung and Nam P Nguyen) for the series “Radiotherapy for Breast Cancer in Advanced Age” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.08.03). The series “Radiotherapy for Breast Cancer in Advanced Age” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Metastatic breast cancer: incidence and natural history
- Symptoms in metastatic breast cancer and role of palliative care
- Outpatient palliative care and models of care
- Unique challenges of metastatic breast cancer in the elderly
- Conclusions
- Acknowledgments
- Footnote
- References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. [Crossref] [PubMed]
- Dai X, Li T, Bai Z, et al. Breast cancer intrinsic subtype classification, clinical use and future trends. Am J Cancer Res 2015;5:2929-43. [PubMed]
- Gennari A, Conte P, Rosso R, et al. Survival of metastatic breast carcinoma patients over a 20-year period: A retrospective analysis based on individual patient data from six consecutive studies. Cancer. 2005;104:1742-50. [Crossref] [PubMed]
- Giordano SH, Buzdar AU, Smith TL, et al. Is breast cancer survival improving? Cancer 2004;100:44-52. [Crossref] [PubMed]
- Chamberlain MC, Baik CS, Gadi VK. Systemic therapy of brain metastasis: non-small cell lung cancer, breast cancer, and melanoma. Neuro Oncol 2017;19:i1-24. [Crossref] [PubMed]
- Caswell-Jin JL, Plevritis SK, Tian L, et al. Change in survival in metastatic breast cancer with treatment advances: Meta-analysis and systematic review. JNCI Cancer Spectr 2018;2:pky062.
- Brufsky AM. Long-term management of patients with hormone receptor-positive metastatic breast cancer: Concepts for sequential and combination endocrine-based therapies. Cancer Treat Rev 2017;59:22-32. [Crossref] [PubMed]
- Rugo HS, Finn RS, Dieras V, et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Res Treat 2019;174:719-29. [Crossref] [PubMed]
- Finn RS, Martin M, Rugo HS. Palbociclib and letrozole in advanced breast cancer. N Engl J Med 2016;375:1925-36. [Crossref] [PubMed]
- Chen MT, Sun HF, Zhao Y, et al. Comparison of patterns and prognosis among distant metastatic breast cancer patients by age groups: a SEER population-based analysis. Sci Rep 2017;7:9254. [Crossref] [PubMed]
- Cherny NI, Paluch-Shimon S, Berner-Wygoda Y. Palliative care: needs of advanced breast cancer patients. Breast Cancer (Dove Med Press) 2018;10:231-43. [Crossref] [PubMed]
- Peart O. Metastatic Breast Cancer. Radiol Technol 2017;88:519M-39M. [PubMed]
- Li BT, Wong MH, Pavlakis N. Treatment and Prevention of Bone Metastases from Breast Cancer: A Comprehensive Review of Evidence for Clinical Practice. J Clin Med 2014;3:1-24. [Crossref] [PubMed]
- Lutz S, Berk L, Chang E, et al. Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 2011;79:965-76. [Crossref] [PubMed]
- NBCF. Metastatic Breast Cancer : The National Breast Cancer Foundation. www.nationalbreastcancer.org. Available online: https://www.nationalbreastcancer.org/metastatic-breast-cancer. Accessed April 30, 2019.
- Temel JS, Greer JA, Muzikansky A, et al. Early Palliative Care of Patients with Metastatic Non-Small-Cell Lung Cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Blackhall LJ, Read P, Studenborg G, et al. PCARE Track for Advanced Cancer: Impact and Timing of an Outpatient Palliative Care Clinic. J Palliat Med 2016;19:57-63. [Crossref] [PubMed]
- Center to Advance Palliative Care. A state-by-state report card on access to palliative care in our nation’s hospitals. 2015 Available online: http://www.capc.org/reportcard.
- Morrison RS, Penrod JD, Cassel JB, et al. Cost Savings associated with US hospital palliative care consultation programs. Arch Intern Med 2008;168:1783-90. [Crossref] [PubMed]
- Bakitas M, Lyons KD, Hegel MT, et al. The Project ENABLE II Randomized Controlled Trial to Improve Palliative Care for Rural Patients with Advanced Cancer: Baseline Findings, Methodological Challenges, and Solutions. Palliat Support Care 2009;7:75-86. [Crossref] [PubMed]
- Byock I, Twohig JS, Merriman M, et al. Promoting excellence in end-of-life care: a report on innovative models of palliative care. J Palliat Med 2006;9:137-51. [Crossref] [PubMed]
- Reiser V, Rosenzweig M, Welsh A, et al. The Support, Education, and Advocacy (SEA) Program of Care for Women With Metastatic Breast Cancer: A Nurse-Led Palliative Care Demonstration Program. Am J Hosp Palliat Care 2019; [Epub ahead of print]. [Crossref] [PubMed]


