
Effect of prosthetic rehabilitation on oral health-related quality of life of patients with head and neck cancer: a systematic review
Introduction
Head and neck cancers constituting malignancies of lip, tongue and oral cavity (ICD10: C00-06), nasopharynx, oropharynx and hypopharynx (ICD10: C09-C10), salivary glands (ICD10: C07-08), larynx, and paranasal sinuses (ICD10: C11-C13) are reported with high morbidity rates (1,2). It can be difficult for the diseased to cope and adapt with its physical, psychological and emotional repercussions affecting their general well-being. With an intention to improve longevity it can be equally challenging for the clinicians to manage such cases, as they not only need to deliver effective treatment but also restore the functional capabilities of the survivors (3).
The vital structures of head and neck enable functions such as mastication, speech, communication, expressions and more. Pathophysiological changes caused by malignancies can substantially impede these functions leading to nutritional deficiencies and social isolations thus hampering the general well-being of an individual. This puts the quality of life (QoL) of such patients more in the forefront than ever before. In a seminal paper published as early as 1995, the author argues that QoL is frequently used in head and neck cancers but it is still not clearly defined (4). Since then, there has been a gradual evolution in the approach by oral health care providers and oral epidemiologists that have led to personalized and condition-specific constructs termed as oral health-related quality of life (OHRQoL) (5). OHRQoL is a multi-dimensional concept that broadly identifies the impact of oral conditions on daily living, such as, problems related to a person’s eating, sleeping, social-interaction and emotional habits (6-8). Generic QoL constructs have long been used to evaluate the QoL in patients with head and neck cancers. However, these questionnaires often do not cater to specific oral health conditions affecting the OHRQoL, as patients with head and neck cancer may be at higher risk of depleted oral health-related daily performances (9). Even the ones treated have been reported with impairment of voice, speech difficulty, and problem to swallow food (10). One recent study states that the oral functions of the patients suffering from head and neck cancers are far worse than the non-head and neck cancer patients (11).
Surgical intervention is a common treatment modality for most head and neck cancers; and oral defects, deformities, dysfunction, and dysphagia are its related complications (12). These oral defects are later treated using various types of prostheses; the outcome of which is to restore the oral functions (13). This idea of oral rehabilitation of patients after their treatment is one of the foremost priorities to the clinicians. Although such improvement in function could be assessed using clinical parameters, but patients’ self-reports using QoL instruments provide insights into their needs, expectations and treatment effectiveness.
The existing evidences talk about the importance of having good health-related QoL among head and neck cancer patients (14,15). Another systematic review done by So et al., 2012; evaluated the QoL of head and neck cancer survivors after treatment (16). However, there is no systematic review to date that assesses the QoL of head and neck cancer patients who have undergone oral rehabilitation using condition specific QoL measuring instrument. The findings are paramount to clinicians and the oral health researchers, as OHRQoL reflects patient’s own evaluation of their oral health status, functional and emotional wellbeing. It is essential to understand the patients’ perspective to enhance the QoL among the head and neck cancer survivors. Thus, the objective of the current study is to conduct a systematic review to evaluate the OHRQoL of head and neck cancer survivors after they have been treated with prosthetic rehabilitation. We hypothesize that prosthetic rehabilitation given to head and neck cancer patients after surgical interventions improves their OHRQoL.
Methods
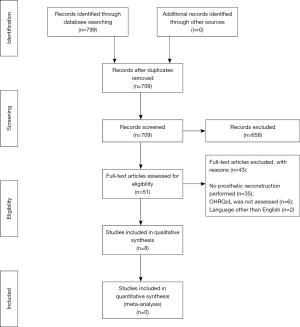
Guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were utilized as the framework in designing, implementing and reporting the current review (17). This invited systematic review was registered at the Research Unit, College of Dentistry, Jazan University, Saudi Arabia. The search was performed during the month of May 2019 and the all published studies until the date were subjected to the selection criteria.
Selection criteria
Inclusion criteria
Publications in English language that use OHRQoL or oral functions as prognostic measure after performing a surgical reconstruction with a prosthetic appliance to treat the patients suffering from head and neck cancer were included. The search of articles was not limited to a particular research design.
Exclusion criteria
Abstract presentations, opinion-based commentaries, and dissertations were excluded. Articles using general health QoL measures with no mention of OHRQoL or oral functions were excluded after reading the abstracts.
Exposure and outcome
The exposure of interest for the current study was the prosthetic rehabilitation performed on the surgically treated head and neck cancer patients, irrespective of the size of the defect, material used for prosthetic reconstruction, duration of the prostheses, age and gender of the patient. Outcome was the OHRQoL after the restoration of oral functions of the treated patients. The patient, intervention, comparison, outcome (PICO) question ordered for the current study: “Does prosthetic rehabilitation improve the OHRQoL among the head and neck cancer survivors?”
Study selection and data extraction
Search of literature was done electronically using Medline, Embase, and Cochrane databases. Two authors (MF Quadri and SK Tadakamadla) independently performed searches using the mentioned keywords and the Boolean operators (Table 1). T John and M Nayeem then independently retrieved the articles according to the set selection criteria, which was later cross checked again by MF Quadri, A Jessani and SK Tadakamadla. Data extraction chart was prepared and used by T John, AW Alamir and M Nayeem, and the information such as, name of the authors, year of publication, type of study, age of patients, gender, type and number of head and neck cancer cases, type of prosthetic appliance used, follow-up period, OHRQoL questionnaire used, assessed oral functions, result of the study and conclusion were extracted.
Table 1
| Search steps | Search terminologies |
|---|---|
| #1 | Oral OR Dental OR Mouth OR intra oral OR gingiva OR Palate or Palatal OR oropharynx OR Cheek OR Head AND Neck |
| #2 | Cancer* OR neoplas* OR carcinoma* OR tumour* OR tumor OR malignan* |
| #3 | #1 AND #2 |
| #4 | Head and Neck Neoplasms OR Squamous Cell Carcinoma of Head and Neck OR Mouth Neoplasms OR Gingival Neoplasms OR Lip Neoplasms OR Palatal neoplasms OR Salivary gland neoplasms OR Tongue neoplasms |
| #5 | #3 OR #4 |
| #6 | Quality of life [tiab] OR Wellbeing [tiab] OR Well-being [tiab] OR Health related Quality of life [tiab] OR HRQOL [tiab] OR Life quality [tiab] OR Daily performances [tiab] OR Daily activities [tiab] OR Daily living [tiab] OR Patient Reported Outcome Measures [tiab] OR Health outcomes [tiab] OR Patient outcome [tiab] |
| #7 | #3 AND #6 |
Search steps were used in appropriate combinations to retrieve the articles. *, truncation was used to broaden the search.
Quality assessment of included studies
Methodological index for non-randomized studies (MINORS) was the assessment tool utilized to report on the quality of the included studies. It has a total of 12 questions assessing the various aspects of published researches, specifically focusing on their methodologies. Each question could be scored on a scale of 0 to 2 with “2” being ideal and “0” being not reported. An ideal score of 16 is suggested for non-comparative studies and 24 for comparative studies. The scale is exclusively designed for research involving compulsory surgical procedures wherein randomization of the patients is not always possible (18).
Results
The initial search had 799 hits and after removal of duplicates 709 published articles remained. Titles and abstracts of these publications were reviewed for their eligibility and 51 articles were selected. Full texts of these were reviewed and assessed in detail according to the selection criteria. Out of the 51 mentioned earlier, 35 articles had no description of the prosthetic rehabilitation, 6 did not assess the OHRQoL and 2 were published in languages other than English (Figure 1).
Study characteristics
Included studies (n=8) were published during the last decade (2009–2019), wherein two were from Japan (13,19) and Germany (20,21); and one each were conducted in Denmark (11), Nigeria (22), India (12) and Switzerland (23). Six out of these eight studies were experimental (11-13,19-21) in design and two were cross-sectional studies (22,23). The cumulative sample size from the selected studies was 382 with the highest and lowest mean age values of 35.9 (14.9) and 72.4 (8.7) years, respectively and more male cases (69.5%) were reported than female cases (30.5%) (Table 2). Squamous cell carcinoma was more frequently reported among all the assessed malignant tumors and maxillary reconstruction and implant supported prosthesis were the choice of treatment for most of the cases (Table 3). The patients in seven studies were followed for at least a year before assessing their oral function and OHRQoL, however one study did not report the duration of follow-up (Table 2).
Table 2
| Author/year | Place of study | Objective of the study | Study type | Mean age (SD) | Sample size (N) |
|---|---|---|---|---|---|
| Sato et al., 2019 (13) | Japan | Evaluate the changes in OHRQoL and self-assessed masticatory ability and investigate the relationship between the self-assessed masticatory ability and occlusal force in patients that underwent oral tumor resection and mandibular implant-supported prosthesis (ISP) placement | Experimental study | Not mentioned | N=10: male =6, female =4 |
| Fromm et al., 2019 (11) | Denmark | To evaluate the OHRQoL as well as the esthetic and functional outcome of oral rehabilitation in HNC—patients compared to non-HNC patients | Prospective experimental study | 70.2 (10.6). Age and gender are matched | N=18: male =12, female =6 |
| Akinmoladun et al., 2018 (22) | Nigeria | To appraise the pattern and challenges of managing patients with maxillectomy and the QoL of a subset of the study population | Cross sectional study | 35.88 (14.9) | N=67: male =30, female =37 |
| Hagio et al., 2018 (19) | Japan | To identify factors affecting the improvement of OHRQoL by using maxillofacial prosthetic treatment after surgery to repair maxillary, mandibular, tongue, and oral floor defects | Prospective experimental study | 72.4 (8.7) | N=50: male =34; female =16 |
| Dholam et al., 2016 (12) | India | Primary—to assess the impact of dental rehabilitation on patients’ OHRQoL following treatment for cancer of oral cavity using LORQv3 and OHIP-14 questionnaire | Experimental study | 51 | N=75: male =50, female =25 |
| Schweyen et al., 2017 (20) | Germany | To evaluate OHRQoL in long-term survivors after RT for HNC and to compare the results with a normal population | Prospective experimental study | 57.7 | N=116: males =87, females =29 |
| Fierz et al., 2013 (23) | Switzerland | To document tumor patients’ QoL 3 to 6 years after prosthetic rehabilitation. | Cross-sectional study | Not mentioned | N=18: male =13, female =5 |
| Linsen et al., 2009 (21) | Germany | To investigate the prevalence of TMD in patients with oral cancer after surgery and prosthodontic rehabilitation, and to evaluate the correlation between TMD, the maximum voluntary bite force, OHRQoL | Experimental study | 62 [16] | N=26: male =14 Female =12 |
OHRQoL, oral health-related quality of life; SD, standard deviation; HNC, head and neck cancer; RT, radiotherapy; TMD, temporomandibular disorders.
Table 3
| Author/year | Site | Type of OC | T/t performed, type of surgery [chemotherapy, radiotherapy (RT)] | Implant supported | Follow-up period |
|---|---|---|---|---|---|
| Sato et al., 2019 | Mandible =10 | Squamous cell carcinoma =5, benign =5 | Tumor resection =10, + chemotherapy =1, chemotherapy + RT =1 | Yes [10] | 1 year |
| Fromm et al., 2019 | Maxilla =5, mandible =1, base of mouth =5, hypopharynx =2, sino-nasal =1, salivary =1, cutaneous =1, oropharynx =2 | Cancer cavum oris =11, other cancer types =7 | Total RT =12, only RT =0, RT + surgery =4, RT + chemotherapy =2, RT + surgery + chemotherapy =6, non-RT =6, surgery alone =6 | Not mentioned | 1 year |
| Akinmoladun et al., 2018 | Maxilla =32 | Chondrosarcoma =1, hemangiopericytoma =1, osteogenic sarcoma =4, squamous cell carcinoma =7, ameloblastic fibrosarcoma =1, malignant ameloblastoma =1, adenocarcinoma =2, adenoid cystic carcinoma =10, mucoepidermoid carcinoma =3, polymorphous low-grade adenocarcinoma =2 | Surgery and prosthetic reconstruction for all | Not mentioned | 2 years |
| Hagio et al., 2018 | Hard palate =24, soft palate =1, mandible =17, tongue =5, oral floor =3 | Not mentioned | Surgery and prosthetic reconstruction for all. None of the defects in maxilla underwent reconstructive surgery | Not mentioned | 1 year |
| Dholam et al., 2016 | Palate (34%), upper alveolus (19%), buccal mucosa (15%), tongue (13%), gingivobuccal sulcus (7%), lower alveolus (7%), and retromolar trigone (5%) | Squamous cell carcinoma (73%), mucoepidermoid carcinoma (5%), adenoid cystic carcinoma (12%), ameloblastoma (1%), others (8%) | Surgery + chemotherapy + RT, partial dentures =20, complete dentures =10 | Not mentioned | 1 year |
| Schweyen et al., 2017 | Nasopharynx =6, oropharynx =31, uvula =1, tongue base =6, oral cavity =38, parotid gland =9, hypopharynx/larynx =25 | Not mentioned | No dentures or FPD =44, CD =30, RPD =42 | Yes for 4 patients | 1 year |
| Fierz et al., 2013 | Maxilla =5+3*, Mandible =10+3* (*, 3 patients had tumor in both jaws) | Squamous cell carcinoma =14, other tumors =4 | Obturator prothesis =3, bar prosthesis on implant (with obturator in maxilla) =8, fixed prosthesis on implant =5, partial prothesis (tooth-supported) =2, wire-clip provisional prosthesis =2, only vacuum-drawn splint (for fluoridation) =1 | Yes | 2 years and 3 months |
| Linsen et al., 2009 | Maxilla =14, mandible =12 | Squamous cell carcinoma =18, adenoid cystic carcinoma =3, Keratocyst =2, enameloblastoma =2, osteosarcoma =1 | Partial resection with segmental mandibulectomy =8, bony reconstruction =6, without bony reconstruction =2 | Yes | Not mentioned |
OC, oral cancer; T/t, treatment; FPD, fixed partial denture; CD, complete denture; RPD, removable partial denture.
OHRQoL assessments
Different versions of oral health impact profile (OHIP) constructs were preferred by most of the studies to assess the OHRQoL among the head and neck cancer patients. Akinmoladun et al. had utilized University of Washington quality of life (UW-QoL) questionnaire (22) and Fierz et al. had utilized European Organization for Research and Treatment of Cancer’s Quality of Life Questionnaire (EORTC QLQ-C30) (23), respectively. The evaluation was focused on the responder’s perception of oral health and the related activities within conceptual domains that are specific to the tool administered. Oral health problems for instance, difficulty in chewing, swallowing, and esthetics were common to most of the included studies (12,13,19,22,23) (Table 4).
Table 4
| Author/year | Name of OHRQoL questionnaire | Oral functions assessed | Analyses used | Results | Conclusion |
|---|---|---|---|---|---|
| Sato et al., 2019 | Japanese version of the Oral Health Impact Profile (OHIP-49) | Masticatory ability. Occlusal force | Wilcoxon signed-rank test | OHIP-49: before =65.3±9.79, after =46.0±8.14 | Implant placement improves OHRQoL and the self-assessed masticatory ability |
| Masticatory ability: before =54.5±9.79, after =68.0±8.37 | The prosthesis types might not significantly affect OHRQoL | ||||
| Fromm et al., 2019 | Danish version OHIP-49 | The Nordic Orofacial Test-Screening (NOT-S) 24 | Independent t-test, Mann-Whitney U-test | Mean OHIP-49: case =42.50 vs. control =20.94, P =0.05 | Oral function is significantly impaired in HNC-patients compared to non-HNC-patients after oral rehabilitation |
| Mean NOT-S: case =4.56 vs. control =0.56, P<0.01 | The mean OHIP-49 score was more among cases in comparison to controls | ||||
| Akinmoladun et al., 2018 | UW-QoL | Swallowing, chewing, speech, taste and saliva | Mean (SD) and % | UW-QoL scores: swallowing =97.2 (2.8), chewing =78.1 (3.1), speech =83.3 (4.2), taste =81.3 (4.1), saliva =100 (0) | Oral functions of the patients after treatment were not fully restored |
| Red | |||||
| Hagio et al., 2018 | Oral Health Impact Profile (OHIP-J54) | Masticatory function, swallowing function, and articulatory function | Wilcoxon signed-rank test | Results from mandibular reconstruction (pre vs. post): dysphagia, P=0.04, articulation, P=0.9, OHIP-J54, P=0.02 | OHRQoL of participants was improved in cancer survivors of the maxillary defect group |
| Green | |||||
| Dholam et al., 2016 | OHIP-14 | Chewing, swallowing, salivation, speech, mouth opening, oro-facial appearance, social interaction | Two group comparisons were made using Mann-Whitney U-test. Three or more group comparisons were made using Kruskal-Wallis test | PD, mean (SD): Chewing 1.45 (0.38), Swallowing 1.12 (0.32), Salivation 1.43 (0.46), Speech 1.15 (0.37), Mouth opening 1.10 (0.31), Orofacial appearance 1.27 (0.44) | The oral cancer patients coped well and adapted to near normal oral status after prosthetic rehabilitation |
| CD, mean (SD): Chewing 2.0 (0.83), Swallowing 1.40 (0.57), Salivation 1.42 (0.43), Speech 1.20 (0.42), Mouth opening 1.0 (0), Orofacial appearance 1.30 (0.48) | This showed improved QoL after one year of dental rehabilitation | ||||
| Schweyen et al., 2017 | OHIP -14 | Not specified | Mann-Whitney U test, Kruskal-Wallis test, linear regression | Denture status [N, mean OHIP (SD)]: none [44, 16.7 (15.5)], RPD [42, 21.2 (16.4)], FPD [30, 20.1 (16.7)] | Prosthetic treatment in HNC patients do not lead to the same improvement in OHRQoL as found in the normal population |
| Fierz et al., 2013 | EORTC QLQ | Sticky saliva, xerostomia, mouth opening, problems with teeth, chewing swallowing, tmj pain, oral pain | Mean (SD) and % | At least “a little effect” reported; sticky saliva =60–70%, xerostomia =40–60%, mouth opening =45–62%, problems with teeth =70–82%, chewing-Swallowing =68–72%, TMJ pain =65–89%, oral pain =45–77% | Most of the surveyed patients responded rather positively to questions about their post-treatment quality of life |
| Linsen et al., 2009 | OHIP-G | Sensitive teeth, toothache, painful gum | Fisher’s exact test, two-sided Cochran-Armitage trend test | Sensitive teeth, P=0.01; toothache, P=0.02; painful gum, P=0.03 | The OHRQoL of patients with oral cancer shows a satisfactory outcome |
OHRQoL, oral health-related quality of life; UW-QoL, University of Washington quality of life; SD, standard deviation; EORTC QLQ, European Organization for Research and Treatment of Cancer’s Quality of Life Questionnaire; CD, complete denture; PD, partial denture.
OHRQoL findings
Overall, the results were inconclusive to demonstrate the improvement in OHRQoL of head and neck cancer patients after prosthetic rehabilitation. Three studies displayed poor OHRQoL among the survivors (11,20,22) by comparing them with healthy controls, irrespective of the type and make of the prostheses. Fromm et al. stated that the oral habits like chewing and swallowing, and the overall esthetic score became worse in comparison to the control group post treatment (11). Similarly, most of the participants in the study conducted by Akinmoladun et al. (22) had reported issues pertaining to swallowing, chewing, speech, taste, and esthetic appearance after prosthetic reconstructions; and Schweyen and colleagues (20) indicated that the OHRQoL among the cancer patients did not improve well enough as compared to their normal counterparts. However, the other included publications had indicated good OHRQoL outcomes after the patients treated for head and neck cancers had been given prosthetic units (12,13,19,21,23). These studies assessed OHRQoL at baseline after cancer diagnosis and compared it after the prosthetic rehabilitation. Sato et al. stated that the QoL scores in the domains like functional limitations, physical discomfort, and physical disability after the placement of implant supported prosthesis had improved (13). Dholam et al. also revealed that there was a slight increase in the masticatory ability of the patients (12). Likewise, Fierz et al. had shown significant enhancement in the OHRQoL of head and neck cancer patients whose oral functions were attempted to be restored using prosthetic appliances (23). Finally, Hagio et al. and Linsen et al. concluded that “OHRQoL of participants had improved in the defect groups after the treatment” (19,21) (Table 4).
Findings of quality analyses using MINORS criteria
Quality analysis of included studies revealed the highest score of 13 for a non-comparative study and 15 for a comparative study. These are below the suggested ideal scores of 16 and 24, respectively. The objectives were clearly defined and the endpoint of the study, i.e., OHRQoL was properly assessed by most of the studies. However, not all the eligible patients were recruited by majority of the studies and one of them had adopted convenience sampling technique. Two studies were retrospective in nature and complex analyses with adequate control groups were missed by many of the included studies (Table 5).
Table 5
| Assessment criteria | Quality scores | |||||||
|---|---|---|---|---|---|---|---|---|
| Sato et al., 2019 | Fromm et al., 2019 | Akinmoladun et al., 2018 | Hagio et al., 2018 | Dholam et al., 2016 | Schweyen et al., 2017 | Fierz et al., 2013 | Linsen et al., 2009 | |
| 1. A clearly stated aim | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
| 2. Inclusion of consecutive patients | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 1 |
| 3. Prospective collection of data | 2 | 0 | 0 | 2 | 2 | 2 | 0 | 2 |
| 4. Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 5. Unbiased assessment of the study endpoint | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 6. Follow-up period appropriate to the aim of the study | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| 7. Loss to follow-up less than 5% | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 8 Prospective calculation of the study size | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 |
| 9. An adequate control group | 0 | 2 | 0 | 0 | 1 | 0 | 0 | 0 |
| 10. Contemporary groups | 0 | 2 | 0 | 0 | 1 | 0 | 0 | 0 |
| 11. Baseline equivalence of groups | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| 12. Adequate statistical analyses | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Total | 11 | 15 | 9 | 13 | 13 | 13 | 9 | 10 |
†, the items are scored 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate). Global ideal score being 16 for non-comparative studies and 24 for comparative studies.
Discussion
Significant advances have been made in treating cancer of head and neck with the emphasis to restore oral functions using prosthetic units. However, evaluating the success of such interventions using OHRQoL among these treated patients seems to be in its initial stages. The current systematic review is first to evaluate the effect of prosthetic rehabilitation on OHRQoL of patients with head and neck cancers. However, the finding based on the eight selected articles involving 382 patients with a minimum of 1-year follow-up is inconclusive to support the hypothesis. In this context, an earlier published report using the QoL construct had suggested that most of the treatment morbidities of head and neck cancer survivors do not return to baseline after being treated (16). However, another study concluded that it usually takes more than 12 months in order to completely restore the functions and thus improve the QoL among the survivors (24). Arguably, there are various other confounding factors that may influence the success of a prosthetic rehabilitation. For instance, implant support, size of reconstruction site, anatomical structures involved, presence of other debilitating systemic diseases etc. (25). Stellingsma et al. in 2005 reported that implant retained prostheses were more beneficial in comparison to the traditional removable prosthesis (26). This could be attributed to the difference in the stability of both the prostheses, and the rehabilitations performed using removable units may lead to functional limitation and physical discomfort thus hampering the OHRQoL (13).
It is to further discuss that the findings derived from the current review also depended on the methodology of the included studies. For instance, the sample sizes were relatively small and not representative. Most of them did not evaluate the OHRQoL of patients before and after the prosthetic rehabilitation. Due to these inconsistencies among the retrieved reports, a meta-analysis was not possible. In addition, studies should have considered longer follow-up period, as 12 months may not be appropriate to assess the rehabilitation outcomes. Analyses controlling for gender, age of the patient, stage of cancer, site of the cancer, type of prosthesis used, presence or absence of radiation therapy, presence or absence of chemotherapy, oral hygiene habits and other chronic medical illnesses would have provided more substantial results from each of the included study.
The strength of this review is exhibited in its comprehensive search strategy that had been applied. Studies were not exclusively limited to prosthetic related search terms as there could be several methods of prosthetic rehabilitation. To avoid loss of relevant articles, all the retrieved texts that spoke about QoL in head and neck cancer patients were individually assessed for their eligibility. Also, the titles involving placement of implants for jaw reconstruction were evaluated in the search.
Implications and future directions
There are volumes of published literature revealing the advancement in the biomedical model focusing on surgical techniques and dedicated man hours to treat head and neck cancer patients (27,28). In addition, similar efforts is required to improve the means of supporting care, restoring of functions and enhancing the QoL of the survivors (29), as this will in turn contribute towards a personalized treatment strategy and rehabilitation process (29-31). Experts have also put forth that the patients or their caregivers must be enlightened with the evidence based self-management strategies to overcome the persisting functional and emotional difficulties that the patients may encounter during the first 12 months of their treatment (16). Also, there are a variety of OHRQoL questionnaires currently available in multiple languages to ease the collection of data for the health care providers while assessing the final outcome of their treated patients, and the findings obtained will specify the type of care that is obtained while restoring the functional and emotional capabilities (32).
To conclude, the included studies in the current systematic review do not provide substantial evidence to support the statement that, prosthetic rehabilitation performed on the surgically treated head and neck cancer patients improves their OHRQoL. The findings are paramount for the clinical decision making and the epidemiological research to enhance patients and public health-related outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Shankargouda Patil, Sachin C. Sarode and Kamran Awan) for the series “Oral Pre-cancer and Cancer” published in Translational Cancer Research. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2019.12.48). The series “Oral Pre-cancer and Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Collaborators GBoDS. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743-800. [Crossref] [PubMed]
- Kalavrezos N, Scully C. Mouth Cancer for Clinicians. Part 1: Cancer. Dent Update 2015;42:250-2, 255-6, 259-60. [Crossref] [PubMed]
- Kalavrezos N, Scully C. Mouth Cancer for Clinicians. Part 9: The Patient and Care Team. Dent Update 2016;43:276-8, 81-2, 85-7.
- Morton RP. Evolution of quality of life assessment in head and neck cancer. J Laryngol Otol 1995;109:1029-35. [Crossref] [PubMed]
- Shiraz F, Rahtz E, Bhui K, et al. Quality of life, psychological wellbeing and treatment needs of trauma and head and neck cancer patients. Br J Oral Maxillofac Surg 2014;52:513-7. [Crossref] [PubMed]
- Black N. Patient reported outcome measures could help transform healthcare. BMJ 2013;346:f167. [Crossref] [PubMed]
- Boyce MB, Browne JP, Greenhalgh J. The experiences of professionals with using information from patient-reported outcome measures to improve the quality of healthcare: a systematic review of qualitative research. BMJ Qual Saf 2014;23:508-18. [Crossref] [PubMed]
- Vannier DM, Somerman MJ. Integrating the domains of dentistry and research: A perspective from the National Institute of Dental and Craniofacial Research. J Am Dent Assoc 2016;147:77-9. [Crossref] [PubMed]
- Tadakamadla J, Kumar S, Lalloo R, et al. Development and validation of a quality-of-life questionnaire for patients with oral potentially malignant disorders. Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:338-49. [Crossref] [PubMed]
- Epstein JB, Robertson M, Emerton S, et al. Quality of life and oral function in patients treated with radiation therapy for head and neck cancer. Head Neck 2001;23:389-98. [Crossref] [PubMed]
- Fromm L, Gotfredsen K, Wessel I, et al. Oral health-related quality of life, oral aesthetics and oral function in head and neck cancer patients after oral rehabilitation. J Oral Rehabil 2019;46:738-46. [PubMed]
- Dholam KP, Chouksey GC, Dugad J. Oral health-related quality of life after prosthetic rehabilitation in patients with oral cancer: A longitudinal study with the Liverpool Oral Rehabilitation Questionnaire version 3 and Oral Health Impact Profile-14 questionnaire. Indian J Cancer 2016;53:256-60. [Crossref] [PubMed]
- Sato N, Koyama S, Mito T, et al. Changes in oral health-related quality of life after oral rehabilitation with dental implants in patients following mandibular tumor resection. J Oral Sci 2019;61:406-11. [Crossref] [PubMed]
- Mehanna HM, De Boer MF, Morton RP. The association of psycho-social factors and survival in head and neck cancer. Clin Otolaryngol 2008;33:83-9. [Crossref] [PubMed]
- van Nieuwenhuizen AJ, Buffart LM, Brug J, et al. The association between health related quality of life and survival in patients with head and neck cancer: a systematic review. Oral Oncol 2015;51:1-11. [Crossref] [PubMed]
- So WK, Chan RJ, Chan DN, et al. Quality-of-life among head and neck cancer survivors at one year after treatment--a systematic review. Eur J Cancer 2012;48:2391-408. [Crossref] [PubMed]
- Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [Crossref] [PubMed]
- Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712-6. [Crossref] [PubMed]
- Hagio M, Ishizaki K, Ryu M, et al. Maxillofacial prosthetic treatment factors affecting oral health-related quality of life after surgery for patients with oral cancer. J Prosthet Dent 2018;119:663-70. [Crossref] [PubMed]
- Schweyen R, Kuhnt T, Wienke A, et al. The impact of oral rehabilitation on oral health-related quality of life in patients receiving radiotherapy for the treatment of head and neck cancer. Clin Oral Investig 2017;21:1123-30. [Crossref] [PubMed]
- Linsen S, Schmidt-Beer U, Fimmers R, et al. Craniomandibular pain, bite force, and oral health-related quality of life in patients with jaw resection. J Pain Symptom Manage 2009;37:94-106. [Crossref] [PubMed]
- Akinmoladun VI, Akinyamoju CA, Olaniran FO, et al. Maxillectomy and Quality of Life: Experience from a Nigerian Tertiary Institution. Niger J Surg 2018;24:125-30. [Crossref] [PubMed]
- Fierz J, Bürgin W, Mericske-Stern R. Patients with oral tumors. Part 2: Quality of life after treatment with resection prostheses. Resection prosthetics: evaluation of quality of life. Schweiz Monatsschr Zahnmed 2013;123:180-91. [PubMed]
- Murphy BA, Ridner S, Wells N, et al. Quality of life research in head and neck cancer: a review of the current state of the science. Crit Rev Oncol Hematol 2007;62:251-67. [Crossref] [PubMed]
- Patel SG, Deshmukh SP, Savant DN, et al. Comparative evaluation of function after surgery for cancer of the alveolobuccal complex. J Oral Maxillofac Surg 1996;54:698-703; discussion 703-4. [Crossref] [PubMed]
- Stellingsma K, Slagter AP, Stegenga B, et al. Masticatory function in patients with an extremely resorbed mandible restored with mandibular implant-retained overdentures: comparison of three types of treatment protocols. J Oral Rehabil 2005;32:403-10. [Crossref] [PubMed]
- Hay A, Nixon IJ. Recent advances in the understanding and management of oropharyngeal cancer. F1000Res 2018; [Crossref] [PubMed]
- Cognetti DM, Weber RS, Lai SY. Head and neck cancer: an evolving treatment paradigm. Cancer 2008;113:1911-32. [Crossref] [PubMed]
- Talwar B, Donnelly R, Skelly R, et al. Nutritional management in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016;130:S32-40. [Crossref] [PubMed]
- Mehanna H, Kong A, Ahmed SK. Recurrent head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016;130:S181-90. [Crossref] [PubMed]
- Rogers SN, Semple C, Babb M, et al. Quality of life considerations in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016;130:S49-52. [Crossref] [PubMed]
- Ojo B, Genden EM, Teng MS, et al. A systematic review of head and neck cancer quality of life assessment instruments. Oral Oncol 2012;48:923-37. [Crossref] [PubMed]


