Comparison of safety and efficacy between total endoscopic resection and conventional open surgery for malignant thyroid tumors: a meta-analysis
Introduction
In the wake of the first successful implementation of thyroid lobectomy by Huscher et al. (1), endoscopic thyroid surgery has attracted wider interest from health providers, and ever since various surgical modalities were successively described (2,3), including endoscopic-assisted thyroidectomy (ET), endoscopic resection of the thyroid gland via breast access approach and other minimally invasive endoscopic surgery (4-7). Subsequently, endoscopic technique has been further discussed and investigated on how to apply it to thyroid surgery, which becomes one of the research interests. With extensive research on and maturity of endoscopy, endoscopic thyroid surgery has been applied to the treatment of practically all benign thyroid conditions including Graves’ disease, and even thyroid malignancy (8-10). As compared with conventional open thyroidectomy (COT), endoscopic thyroidectomy (ET) has remained controversial due to its inability in protecting recurrent laryngeal nerve (RLN) and parathyroid gland, though this procedure can lead to both treatment purpose and optimal cosmetic results (4,11,12). Although some meta-analyses have been done on the safety and possibility of endoscopic resection of thyroid tumors, yet cases included in previous studies are mostly limited to benign tumors. In order to clarify the disagreement, current study was undertaken to evaluate the efficacies and safety of total endoscopic surgery in thyroid neoplasm, with an attempt to expand scientific evidences in wider application of this technique to thyroid cancer treatment in clinic.
Methods
Search strategies
Published literatures were systematically retrieved from the electronic databases, including PubMed, Web of Science, Cochrane and Google scholar. Major retrieval subject words consisted of: (I) “thyroid neoplasms”; “thyroid cancer”; “thyroid carcinoma”; “thyroid*”, and (II) “endoscopy”; “endoscop*”. Paired subject words were chosen from each of the two categories aforementioned, and Boolean operator “AND” was used to narrow the results. If the studies retrieved in above-mentioned databases only included abstracts or incomplete information, we requested full texts or full data by document delivery service system within the library of Wannan Medical College or from the corresponding author.
Inclusion criteria
Criteria to include the studies were as follows: (I) published literatures in English language on the tumor treatment with endoscopy from January of 2005 through 2019; (II) the tumor was either benign or malignant thyroid postoperatively confirmed by pathology; (III) the surgical methods included both ET and COT. Studies were excluded if: (I) the reported cases were associated with thyroiditis; (II) they were non-English literatures, summary submitted to academic conference, correspondence letters, case reports or overlapped reports.
Data extraction
In the study, two authors (Lin-Long Mo and Fan-Lun Meng) were assigned to independently assess the extracted indexes. Detailed observations comprised full name for the first author, journal and publication year, research design, sample size, patients’ age and gender, tumor size, presence of extra-capsular invasion, lymph node metastasis, operative duration, hospital stay days, incidences of postoperative transient or permanent RLN paralysis, transient or permanent hypocalcemia, total postoperative complications, postoperative bleeding, haematoma and recurrence as well as patients’ satisfaction the cosmetic results.
Statistical analysis
Statistical analysis was carried out with software Review Manager (RevMan, version 5.3, Copenhagen: The Nordic Cocharane Centre) for meta-analysis. The counted data were statistically analyzed by advantage ratio (OR) as curative efficacies, and measured data were analyzed with weighted mean difference (WMD). Interval was estimated as 95% confidence interval (CI). Continuous variables were collectively calculated by mean difference (MD). The dichotomous variable was jointly computed using odds ratio (OR) in case of no occurrence of negative events, and analyzed as rate difference (RD) of otherwise, provided that more negative events were found. P<0.05 was accepted as statistical significance.
Results
Identification of the studies
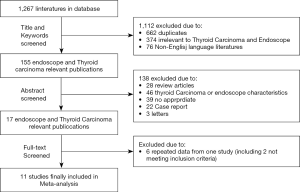
Of the 1,267 potential literatures initially retrieved (Figure 1), 662 were overlapped and excluded, in which 374 unrelated researches and 76 studies in non-English language were removed from the list after reviewing of the article titles and key words. Further review on the abstracts of the articles, 17 studies appeared credible for meta-analysis. Again, 2 studies considered ineligible for current work and another 6 overlapped investigation were excluded following our careful reading of the full texts and group discussion. Finally, 11 researches were included (13-23) (Figure 1). Primary informative indexes were summarized in Tables 1 and 2. Of the 11 studies, 6 were prospective randomized controlled, and 5 retrospective. Sample sizes in individual study ranged from 59 to 1,003.
Table 1
| First author | Year | Sample size | Median age [range] year | Sex (male/female) | Patient source | Research design |
|---|---|---|---|---|---|---|
| Yi-Chao Wang | 2015 | 442 | ET: 36.1±9.7; COT: 40.8±9.0 | ET: 13/211; COT: 20/198 | West China Hospital of Sichuan University | Prospective randomized controlled trial |
| Rui Qu | 2018 | 76 | ET: 6.7±10.0; COT: 43.2±14.3 | ET: 9/31; COT: 14/22 | First Affiliated Hospital of Jinan University | Prospective randomized controlled trial |
| Yoon Woo Koh | 2009 | 59 | ET: 36.5±5.1; COT: 38.3±4.5 | ET: 3/26; COT: 6/24 | Soonchunhyang University College of Medicine | Prospective randomized controlled trial |
| Ki Nam Park | 2015 | 152 | ET: 38.0±9.4; COT: 50.8±11.5 | ET: 4/46; COT: 14/88 | SoonChunHyang University College of Medicine | Prospective randomized controlled trial |
| Hayemin Lee | 2012 | 78 | ET: 42.3±7.6; COT: 49.0±10.8 | ET: 0/37; COT: 3/38 | Bucheon St. Mary’s Hospital, The Catholic University of Korea | Prospective randomized controlled trial |
| Doh Young Lee | 2015 | 280 | ET: 25.9±7.4; COT: 24.9±7.3 | ET: 12/64; COT: 37/167 | Korea University College of Medicine | Prospective randomized controlled trial |
| Seon Kwang Kim | 2015 | 1,003 | ET: 38.9 [17–57]; COT: 49.53 [17–84] | ET: 13/173; COT: 96/830 | Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital | Retrospective review |
| Eun Young Kim | 2017 | 738 | ET: 39.5±0.8; COT: 48.9±0.5 | ET: 8/192; COT: 138/400 | Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine | Retrospective review |
| Jong Ju Jeong | 2009 | 499 | ET: 39.6±8.8; COT: 49.5±10.2 | ET: 7/268; COT: 35/189 | Yonsei University College of Medicine | Retrospective review |
| Kyung Tae | 2011 | 88 | ET: 36.2±9.9; COT: 44.6±11.8 | ET: 1/30; COT: 11/25 | College of Medicine, Hanyang Universitye | Retrospective review |
| Weili Gao | 2013 | 67 | ET: 38.94±11.58; COT: 40.79±11.14 | ET: 8/27; COT: 7/26 | Huzhou Central Hospital, Zhejiang | Retrospective review |
ET, endoscopic thyroidectomy; COT, conventional open thyroidectomy.
Table 2
| First author | Year | Tumor size (cm) | Extrathyroidal invasion (+/total) | Lymph node metastases (+/total) | Surgical procedures |
|---|---|---|---|---|---|
| Yi-Chao Wang | 2015 | – | – | – | Ipsilateral total and contralateral partial thyroidectomy; unilateral lobectomy; subtotal thyroidectomy; total thyroidectomy |
| Rui Qu | 2018 | ET: 1.88±0.61; COT: 2.16±0.63 | – | ET: 11/40; COT: 13/36 | Total thyroidectomy; total thyroidectomy + CLND |
| Yoon Woo Koh | 2009 | ET: 0.72± 0.24; COT: 0.71± 0.27 | ET: 4/29; COT: 12/30 | ET: 10/29; COT: 12/30 | Total thyroidectomy; total thyroidectomy + CLND |
| Ki Nam Park | 2015 | ET: 0.80±0.37; COT: 0.76±0.19 | ET: 28/50; COT: 70/102 | – | Total thyroidectomy; total thyroidectomy + CLND |
| Hayemin Lee | 2012 | ET: 0.5±0.231; COT: 0.41±0.264 | ET: 4/37; COT: 6/41 | ET: 5/37; COT: 1/41 | Lobectomy and isthmectomy + CLND |
| Doh Young Lee | 2015 | ET: 0.8±0.5; COT: 0.8 ±0.5 | ET: 34/76; COT: 89/204 | – | Total thyroidectomy; total thyroidectomy + CLND |
| Seon Kwang Kim | 2015 | – | ET: 4/173; COT: 127/830 | ET: 34/1733; COT: 312/830 | Lobectomy; subtotal thyroidectomy; total thyroidectomy; total thyroidectomy + CLND |
| Eun Young Kim | 2017 | ET: 1.03±0.04; COT: 0.93±0.02 | ET: 111/200; COT: 374/538 | ET: 92/200; COT: 279/538 | Total thyroidectomy; total thyroidectomy + CLND |
| Jong Ju Jeong | 2009 | ET: 0.56±0.19; COT: 0.60±0.22 | ET: 88/275; COT: 91/224 | ET: 62/275; COT: 74/224 | Total thyroidectomy; total thyroidectomy + CLND |
| Kyung Tae | 2011 | ET: 0.76±0.49; COT: 0.64±0.23 | ET: 2/31; COT: 1/36 | ET: 4/16; COT: 2/12 | Total thyroidectomy + CCND |
| Weili Gao | 2013 | ET: 0.77±0.21; COT: 0.76±0.20 | ET: 2/35; COT: 2/33 | ET: 16/35; COT: 16/33 | Lobectomy and isthmectomy + CCND; total thyroidectomy + CCND |
ET, endoscopic thyroidectomy; COT, conventional open thyroidectomy; CLND, central lymph node dissection.
Main research indicators
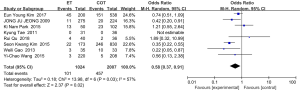
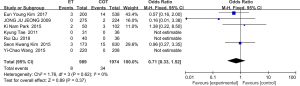
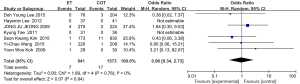
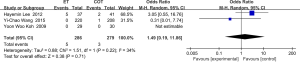
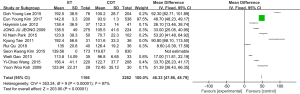
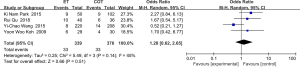
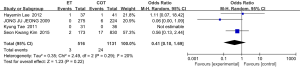
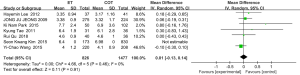
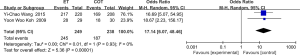
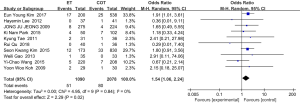
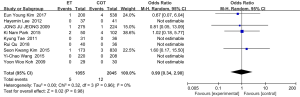
RLN is found above the tracheoesophageal sulcus, and injury to it in surgical procedure can mostly occur in the nerval segment prior to the larynx and deep plane beneath the thyroid gland. Of the 11 studies included in current work, 10 were involved in comparative analysis on causes for temporary RLN paralysis, and 9 for permanent RLN paralysis using fixed effect model. The findings showed that ET resulted in higher risk than COT for transient palsy of RLN, with significant statistical differences (OR =1.54, 95% CI: 1.06–2.24, P=0.02, Figure 2), yet difference was insignificant in permanent RLN injury between the two surgical options (OR =0.99, 95% CI: 0.34–2.90, P=0.98, Figure 3). Eight studies analyzed on the causes for transient hypocalcemia in patients following surgery, and concluded that incidence of postoperative hypocalcemia was much lower in ET group (OR =0.58, 95% CI: 0.37–0.91, P=0.02, Figure 4), whereas the difference was not significant in permanent hypocalcemia as described in 7 studies between ET and COT (OR =0.71, 95% CI: 0.33–1.52, P=0.37, Figure 5). Also, our meta-analysis covered the incidences of postoperative hemorrhage, incisional hematoma, total complications and recurrence rate of thyroid cancer treated by ET and COT, and the observations indicated no significant difference regarding the four indicators between the surgical approaches (Figures 6-9).
Secondary research outcomes
The operative duration was defined by the shortest as the procedure initiated from skin incision through completion of skin suturing, and generally described in the 11 studies. The results showed significant difference between the two surgical modalities, with COT being the shortest (MD =48.33, 95% CI: 47.86–48.79, P<0.000001, Figure 10). Post-operative hospital stay was counted from the next day after operation to the day at discharge, and no significant difference was found between groups (MD =0.01, 95% CI: −0.13–0.14, P=0.91, Figure 11). By far, evaluation on the cosmetic results after thyroidectomy was exclusively rooted on subjective conception from patients because of unavailable objective indicators. In the 11 studies by follow-up questions with “satisfaction” or “un-satisfaction”, two indicated that the patients were subjectively satisfied with aesthetic effect by ET (OR =17.14, 95% CI: 6.07–48.46, P<0.00001, Figure 12).
Discussion
Thyroid diseases often occur in women, and incidence of thyroid neoplasm tends to increase annually and affect younger population (24). Most patients with thyroid tumors have better long-term survival after operation (25,26), yet the visible scars from thyroidectomy at the neck become the concerns of patients with their beauty, even certain mental burden, potentially messing the quality of life. Therefore, ET with both treatment and cosmetic outcomes has been introduced and rapidly developed, widely accepted by patients.
Previously, ET mostly applies to benign thyroid lesions, yet remains controversial due to problems in protecting RLN and parathyroid gland in procedure, and few reports are available on the curative effects by this technique in malignant thyroid condition (4,11,12). In this study, we tentatively collected the clinical reports on endoscopic dissection of thyroid carcinomas published between January of 2005 and 2019 for a meta-analysis. The findings suggest ET and COT are not significantly different by long-term observation on the most complications following surgery, including RLN paralysis and hypocalcemia. Interestingly, we observed lower incidence of transient RLN palsy by COT than by ET through data analysis. This may possibly be attributed to: (I) easy visual identification of the laryngeal nerve from other adjacent structures by anatomy; (II) flexible COT on the part of surgeons can ensure higher safety in protection of the laryngeal nerves due to well-exposed surgical field. However, ET leads to much lower incidence of postoperative transient hypocalcemia. This may be associated with enlarged surgical field by endoscopy, because the parathyroid tissue is smaller and similar to adipose tissue surrounding it, making hard visual identification. In addition, we compared the total incidences of postoperative complications such as hemorrhage and incisional hematoma, recurrence rate of malignant thyroid gland, and found no significant difference in the four indexes between the two surgical options. The results are consistent with previous studies (26-28). Furthermore, observation on the follow-up evaluation of aesthetic effect in two of the 11 studies indicated that patients would be more satisfied with the results from private scars of ET.
In conclusion, our meta-analysis indicates that ET can be reasonable for thyroid cancer, and has better cosmetic effects. Although ET may be used as an alternative to COT in the treatment of thyroid cancer, yet our work failed to conduct investigation on the subgroup of thyroid neoplasm such as tumor size, for which the indications for ET should be further determined in following studies.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.02.29). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huscher CS, Chiodini S, Napolitano C, et al. Endoscopic right thyroid lobectomy. Surg Endosc 1997;11:877. [Crossref] [PubMed]
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [Crossref] [PubMed]
- Ng WT. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 2000;10:339-40. [Crossref] [PubMed]
- Zhang D, Wang T, Dionigi G, et al. Comparison of parathyroid hormone kinetics in endoscopic thyroidectomy via bilateral areola with open thyroidectomy. BMC Surg 2019;19:190. [Crossref] [PubMed]
- Park JH, Bilegsaikhan SE, Suh YJ. A Novel Technique for Performing Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA): A Single-port Platform. Surg Laparosc Endosc Percutan Tech 2020;30:e4-7. [Crossref] [PubMed]
- Luna-Ortiz K, Gomez-Pedraza A, Anuwong A. Lessons Learned from the Transoral Endoscopic Thyroidectomy with Vestibular Approach (TOETVA) for the Treatment of Thyroid Carcinoma. Ann Surg Oncol 2020;27:1356-60. [Crossref] [PubMed]
- Bamroong P, Kasemsiri P, Thongrong C, et al. Modified equipment for facilitating the transoral vestibular approach to endoscopic thyroidectomy. J Minim Access Surg 2019; [Epub ahead of print]. [PubMed]
- Nguyen XH, Nguyen XH, Mai TKN, et al. Feasibility and Safety of Endoscopic Thyroidectomy Via a Unilateral Axillobreast Approach for Unilateral Benign Thyroid Tumor in Vietnam. Surg Laparosc Endosc Percutan Tech 2019;29:447-50. [Crossref] [PubMed]
- Cho J, Park Y, Baek J, et al. Single-incision endoscopic thyroidectomy for papillary thyroid cancer: A pilot study. Int J Surg 2017;43:1-6. [Crossref] [PubMed]
- Chai YJ, Chung JK, Anuwong A, et al. Transoral endoscopic thyroidectomy for papillary thyroid microcarcinoma: initial experience of a single surgeon. Ann Surg Treat Res 2017;93:70-5. [Crossref] [PubMed]
- Tae K, Ji YB, Song CM, et al. Safety and efficacy of transoral robotic and endoscopic thyroidectomy: The first 100 cases. Head Neck 2020;42:321-9. [Crossref] [PubMed]
- Park JO, Wang SG, Park D, et al. The Feasibility of a Prototype Thyroidoscope for Gasless Transoral Endoscopic Thyroidectomy: A Preclinical Cadaver Study. J Laparoendosc Adv Surg Tech A 2019;29:953-7. [Crossref] [PubMed]
- Gao W, Liu L, Ye G, et al. Application of minimally invasive video-assisted technique in papillary thyroid microcarcinoma. Surg Laparosc Endosc Percutan Tech 2013;23:468-73. [Crossref] [PubMed]
- Jeong JJ, Kang SW, Yun JS, et al. Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol 2009;100:477-80. [Crossref] [PubMed]
- Kim EY, Lee KH, Park YL, et al. Single-Incision, Gasless, Endoscopic Trans-Axillary Total Thyroidectomy: A Feasible and Oncologic Safe Surgery in Patients with Papillary Thyroid Carcinoma. J Laparoendosc Adv Surg Tech A 2017;27:1158-64. [Crossref] [PubMed]
- Kim SK, Kang SY, Youn HJ, et al. Comparison of conventional thyroidectomy and endoscopic thyroidectomy via axillo-bilateral breast approach in papillary thyroid carcinoma patients. Surg Endosc 2016;30:3419-25. [Crossref] [PubMed]
- Koh YW, Kim JW, Lee SW, et al. Endoscopic thyroidectomy via a unilateral axillo-breast approach without gas insufflation for unilateral benign thyroid lesions. Surg Endosc 2009;23:2053-60. [Crossref] [PubMed]
- Lee DY, Lim S, Kang SH, et al. A prospective 1-year comparative study of transaxillary total thyroidectomy regarding functional outcomes: Is it really promising? Surg Endosc 2016;30:1599-606. [Crossref] [PubMed]
- Lee H, Lee J, Sung KY. Comparative study comparing endoscopic thyroidectomy using the axillary approach and open thyroidectomy for papillary thyroid microcarcinoma. World J Surg Oncol 2012;10:269. [Crossref] [PubMed]
- Qu R, Li J, Yang J, et al. Treatment of differentiated thyroid cancer: can endoscopic thyroidectomy via a chest-breast approach achieve similar therapeutic effects as open surgery? Surg Endosc 2018;32:4749-56. [Crossref] [PubMed]
- Tae K, Ji YB, Cho SH, et al. Initial experience with a gasless unilateral axillo-breast or axillary approach endoscopic thyroidectomy for papillary thyroid microcarcinoma: comparison with conventional open thyroidectomy. Surg Laparosc Endosc Percutan Tech 2011;21:162-9. [Crossref] [PubMed]
- Wang YC, Zhu JQ, Liu K, et al. Surgical Outcomes Comparison Between Endoscopic and Conventional Open Thyroidectomy for Benign Thyroid Nodules. J Craniofac Surg 2015;26:e714-8. [Crossref] [PubMed]
- Park KN, Cho SH, Lee SW. Nationwide multicenter survey for current status of endoscopic thyroidectomy in Korea. Clin Exp Otorhinolaryngol 2015;8:149-54. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. [Crossref] [PubMed]
- Hu JQ, Wen D, Ma B, et al. The extent of lymph node yield in central neck dissection can be affected by preoperative and intraoperative assessment and alter the prognosis of papillary thyroid carcinoma. Cancer Med 2020;9:1017-24. [Crossref] [PubMed]
- Borges AK, Ferreira JD, Koifman S, et al. Differentiated thyroid carcinoma: a 5-years survival study at a referral hospital in Brazil. Rev Saude Publica 2019;53:106. [Crossref] [PubMed]
- Miccoli P, Elisei R, Materazzi G, et al. Minimally invasive video-assisted thyroidectomy for papillary carcinoma: a prospective study of its completeness. Surgery 2002;132:1070-3; discussion 1073-4. [Crossref] [PubMed]
- Kitano H, Fujimura M, Kinoshita T, et al. Endoscopic thyroid resection using cutaneous elevation in lieu of insufflation. Surg Endosc 2002;16:88-91. [Crossref] [PubMed]