
The prognostic roles of red blood cell-associated indicators in patients with resectable gastric cancers
Introduction
Gastric cancer (GC) is one of the most common malignancies in the world and the second leading cause of cancer-related death in China (1). The 5-year survival rate is 36% in patients diagnosed with the operable disease who receive perioperative chemotherapy, while that of patients in advanced or metastatic phase is only 5–20% with the mean overall survival (OS) being less than 1 year (2). Unfortunately, a lack of effective early diagnostic markers and obvious clinical symptoms leads to GC commonly being diagnosed at advanced stages (3). Therefore, it is essential to identify reliable predictive indicators for the diagnosis and follow-up of resectable GC.
Red blood cell (RBC)-related indicators include RBC, hemoglobin (HGB), hematocrit (HCT), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), and RBC distribution width (RDW). RBC, also known as erythrocytes, can carry oxygen throughout the body and circulate in the blood. A lack of RBCs in the blood is a major characteristic of anemia, a frequent complication in cancer patients (4). HGB concentration was considered as a significant prognostic indicator in squamous cell carcinoma at several sites, like the esophagus (5), head, and neck (6). HCT is the volume percentage of RBCs in blood and could indicate anemia (7,8). MCV is a measurement of RBC size (9), which could reflect folate deficiency (10). MCH refers to a calculation of the average HGB content of each RBC, another factor correlated with anemia that represents the iron metabolism (11). MCHC is calculated by dividing the HGB by the HCT and can reflect average HGB concentration (12). RDW reflects the heterogeneity in erythrocyte size, and it is used clinically to differentiate types of anemia (13).
Several factors, including the clinical tumor stage, have been confirmed to be involved in the natural history of GC. However, tumor staging alone cannot predict GC patients’ prognosis (14). A few serum indexes have attracted increasing interest as prognostic markers, like the C-reactive protein level, and platelet count (15,16). Accumulated evidence indicates that these serum biomarkers are becoming increasingly useful for monitoring and predicting early recurrence and poor prognosis (17,18).
However, the prognostic significance of the RBC-related indicators in resectable GC patients has not been well investigated thus far. Accordingly, we performed this retrospective cohort study in 104 resectable GC patients undergoing surgery or/and adjuvant chemotherapy and systematically evaluated the prognostic value of RBC-related indicators for survival.
Methods
Subjects and inclusion criteria
The researchers retrospectively analyzed resectable GC patients who had been admitted to Soochow University’s First Affiliated Hospital (Jiangsu, China) between June 2006 and July 2016. Approval for the research was given by the First Affiliated Hospital of Soochow University’s medical ethics board. Clinical and clinical records of all the patients involved in the study were periodically evaluated.
In total, this study enrolled 104 resectable GC patients. Cases were surgically and pathologically confirmed. The characteristics of patients are listed in Table 1. Of the 104 patients, the median age was 60 (range, 30–77) years, 77 patients were male, and 27 were female. Cancer treatment was performed according to the type of tumor-nodules-metastases (TNM) and graded through the guidelines of the American Joint Committee on Cancer (AJCC). Prognostic study on OS was performed.
Table 1
| Clinicopathologic features | n (n=104) | HGB | HCT | MCV | MCH | MCHC | RDW | RBC | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low (n) | High (n) | χ2 | P value | Low (n) | High (n) | χ2 | P value | Low (n) | High (n) | χ2 | P value | Low (n) | High (n) | χ2 | P value | Low (n) | High (n) | χ2 | P value | Low (n) | High (n) | χ2 | P value | Low (n) | High (n) | χ2 | P value | ||||||||
| Gender | 14.46 | 0.001** | 16.21 | 0.001** | 2.451 | 0.117 | 11.26 | 0.001** | 4.052 | 0.044* | 3.237 | 0.072 | 11.26 | 0.000** | |||||||||||||||||||||
| Male | 77 | 30 | 47 | 29 | 48 | 35 | 42 | 31 | 46 | 34 | 43 | 44 | 33 | 31 | 46 | ||||||||||||||||||||
| Female | 27 | 22 | 5 | 23 | 4 | 17 | 10 | 21 | 6 | 18 | 9 | 10 | 17 | 21 | 6 | ||||||||||||||||||||
| Age (years) | 0.000 | 1.000 | 0.154 | 0.695 | 1.387 | 0.239 | 1.387 | 0.239 | 0.154 | 0.695 | 1.353 | 0.245 | 1.387 | 0.239 | |||||||||||||||||||||
| ≤60 | 54 | 27 | 27 | 26 | 28 | 30 | 24 | 30 | 24 | 28 | 26 | 31 | 23 | 24 | 30 | ||||||||||||||||||||
| >60 | 50 | 25 | 25 | 26 | 24 | 22 | 28 | 22 | 28 | 24 | 26 | 23 | 27 | 28 | 22 | ||||||||||||||||||||
| Tumor size (cm) | 0.474 | 0.491 | 1.316 | 0.251 | 1.316 | 0.251 | 1.316 | 0.251 | 0.053 | 0.819 | 0.000 | 0.993 | 0.053 | 0.819 | |||||||||||||||||||||
| ≤5 | 79 | 38 | 41 | 37 | 42 | 42 | 37 | 37 | 42 | 40 | 39 | 41 | 38 | 40 | 39 | ||||||||||||||||||||
| >5 | 25 | 14 | 11 | 15 | 10 | 10 | 15 | 15 | 10 | 12 | 13 | 13 | 12 | 12 | 13 | ||||||||||||||||||||
| Depth of invasion | 0.840 | 0.359 | 0.840 | 0.359 | 0.840 | 0.359 | – | 0.028* | – | 0.028* | 1.011 | 0.315 | 0.000 | 1.000 | |||||||||||||||||||||
| T1, T2 | 5 | 1 | 4 | 1 | 4 | 1 | 4 | 0 | 5 | 0 | 5 | 1 | 4 | 3 | 2 | ||||||||||||||||||||
| T3, T4 | 99 | 51 | 48 | 51 | 48 | 51 | 48 | 53 | 47 | 52 | 47 | 53 | 46 | 49 | 50 | ||||||||||||||||||||
| Lymphonodus metastasis | 4.887 | 0.027* | 3.128 | 0.077 | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | 0.057 | 0.812 | 3.128 | 0.077 | |||||||||||||||||||||
| N0, N1 | 28 | 19 | 9 | 18 | 10 | 14 | 14 | 14 | 14 | 14 | 14 | 14 | 14 | 18 | 10 | ||||||||||||||||||||
| N2 | 76 | 33 | 43 | 34 | 42 | 38 | 38 | 38 | 38 | 38 | 38 | 40 | 36 | 34 | 42 | ||||||||||||||||||||
| AJCC stage | 4.685 | 0.030* | 4.685 | 0.030* | 0.000 | 1.000 | 0.750 | 0.387 | 0.750 | 0.387 | 0.467 | 0.495 | 6.746 | 0.009** | |||||||||||||||||||||
| II, II | 30 | 20 | 10 | 20 | 10 | 15 | 15 | 13 | 17 | 13 | 17 | 14 | 16 | 21 | 9 | ||||||||||||||||||||
| III | 74 | 32 | 42 | 32 | 42 | 37 | 37 | 39 | 35 | 39 | 35 | 40 | 34 | 31 | 43 | ||||||||||||||||||||
*, P<0.05; **, P<0.01. RBC, red blood cell; OS, overall survival; HGB, hemoglobin; HCT, hematocrit; MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; RDW, RBC distribution width; AJCC, American Joint Committee on Cancer.
Blood samples
Blood samples were analyzed using a hematology analyzer (Sysmex XE-2100; Sysmex, Kobe, Japan). RBC, HGB, HCT, MCV, MCH, MCHC, and RDW levels were recorded in Table 1. The patients were divided into two groups according to the median values of RBC, HGB, HCT, MCV, MCH, MCHC, or RDW. The post-/pre-treatment ratios were defined as the rate of pretreatment RBC-related indicators values and the corresponding ones obtained after therapy.
Evaluation
Computed tomography (CT) scanning was conducted every 2 months for response evaluation and analyzed according to Response Evaluation Criteria in Solid Tumors (RECIST) criteria 1.1.
Follow-up
Survival period has been estimated from the start of chemotherapy to death, or the last surgical examination. Prognostic analyses concerning OS were conducted, and OS was identified as the time from any cause from the date it was diagnosed to death.
Statistical analysis
All statistical analyses were performed using SPSS 19.0 software (Chicago, IL, USA). The χ2 tests explored the associations between RBC-related indicators status and clinicopathologic features. For analysis of survival data, Kaplan-Meier curves were constructed, and statistical analysis was conducted using the log-rank test. The t-tests assessed the relationships between changes in the RBC-related indicators status and surgery or chemotherapy. The multivariate logistic regression model was employed to find the independent risk factors associated with resectable GC. All values of P<0.05 were considered statistically significant.
Results
Pretreatment MCHC level was correlated with outcomes of resectable GC patients
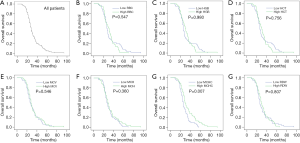
Median OS for all the resectable GC patients was 28 months [95% confidence interval (CI), 25.902–30.098] (Figure 1A). The Kaplan-Meier plots were used to determine the effect of pretreatment RBC, HGB, HCT, MCV, MCH, MCHC, and RDW status on OS (Figure 1B,C,D,E,F,G,H). The patients were divided into two groups according to the median value of RBC (low RBC, ≤4.205×1012/L or high RBC, >4.205×1012/L), HGB (low HGB, ≤129.000 g/L or high HGB, >129.000 g/L), HCT (low HCT, ≤0.380 L/L or high HCT, >0.380 L/L), MCV (low MCV, ≤90.825 fl or high MCV, >90.825 fl), MCH (low MCH, ≤30.745 pg or high MCH, >30.745 pg), MCHC (low MCHC, ≤337.935 g/L or high MCHC, >337.935 g/L) and RDW (low RDW, ≤12.900% or high RDW, >12.900%). The median OS of the high RBC group was 30 months (95% CI, 24.952–35.048), while that of the low RBC group was 26 months (95% CI, 24.233–27.767) (P=0.547). The median OS of the high HGB group was 30 months (95% CI, 26.467–33.533), while that of the low HGB group was 26 months (95% CI, 22.980–29.020) (P=0.980). The median OS of the high HCT group was 30 months (95% CI, 26.469–33.531), while that of the low HCT group was 26 months (95% CI, 23.432–28.568) (P=0.756). The median OS of the high MCV group was 28 months (95% CI, 25.646–30.354), while that of the low MCV group was 26 months (95% CI, 21.962–30.038) (P=0.546). The median OS of the high MCH group was 28 months (95% CI, 24.971–31.029), while that of the low MCH group was 26 months (95% CI, 22.859–29.141) (P=0.360). The median OS of the high MCHC group was 29 months (95% CI, 26.173–31.827), while that of the low MCHC group was 26 months (95% CI, 24.096–27.904) (P=0.007). The median OS of the high RDW group was 29 months (95% CI, 26.403–31.597), while that of the low RDW group was 26 months (95% CI, 23.606–28.394) (P=0.807). Thus, the patients with high pretreatment MCHC levels had increased survival ratio. However, pretreatment levels of RBC, HGB, HCT, MCV, MCH, and RDW had no effects on OS.
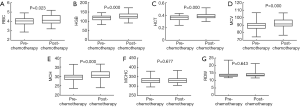
Effects of surgery on the values of RBC-related indicators
The relationships between changes in the RBC-related indicators levels and surgery are respectively presented in Figure 2. The median value of RBC was 4.205×1012/L (4.060×1012/L–4.330×1012/L) before surgery, and 4.060×1012/L (3.950×1012/L–4.185×1012/L) after surgery (P=0.109). The median value of HGB was 129.000 (123.170–134.830) g/L before surgery, and 121.000 (116.003–125.997) g/L after surgery (P=0.005). The median value of HCT was 0.380 (0.365–0.390) L/L before surgery, and 0.370 (0.350–0.380) L/L after surgery (P=0.052). The median value of MCV was 90.825 (90.265–92.400) fl before surgery, and 90.115 (88.902–90.920) fl after surgery (P=0.299). The median value of MCH was 30.745 (30.001–31.210) pg before surgery, and 29.700 (29.321–30.180) pg after surgery (P=0.046). The median value of MCHC was 337.935 (334.375–341.980) g/L before surgery, and 328.700 (325.240–333.659) g/L after surgery (P=0.013). The median value of RDW was 12.900% (12.635–13.100%) before surgery, and 13.580% (13.300–13.800%) after surgery (P=0.001). Surgery significantly decreased the values of HGB, MCH, and MCHC, and increased the value of RDW, while it had no obvious effects on the values of RBC, HCT, or MCV.

Effects of adjuvant chemotherapy on the values of RBC-related indicators
The effects of adjuvant chemotherapy on the levels of the RBC-related indicators are shown in Figure 3. The median value of RBC was 4.060×1012/L (3.950×1012/L–4.185×1012/L) before adjuvant chemotherapy, and 4.130×1012/L (4.005×1012/L–4.239×1012/L) after adjuvant chemotherapy (P=0.023). The median value of HGB was 121.000 (116.003–125.997) g/L before adjuvant chemotherapy, and 126.000 (122.839–130.161) g/L after adjuvant chemotherapy (P=0.000). The median value of HCT was 0.370 (0.350–0.380) L/L before adjuvant chemotherapy, and 0.385 (0.370–0.400) L/L after adjuvant chemotherapy (P=0.000). The median value of MCV was 90.115 (88.902–90.920) fl before adjuvant chemotherapy, and 91.700 (90.790–93.160) fl after adjuvant chemotherapy (P=0.000). The median value of MCH was 29.700 (29.321–30.180) pg before adjuvant chemotherapy, and 30.695 (30.200–31.000) pg after adjuvant chemotherapy (P=0.000). The median value of MCHC was 328.700 (325.240–333.659) g/L before adjuvant chemotherapy and 330.315 (325.240–332.000) g/L after adjuvant chemotherapy (P=0.677). The median value of RDW was 13.580% (13.300–13.800%) before adjuvant chemotherapy and 13.640% (13.500–13.940%) after adjuvant chemotherapy (P=0.643). Adjuvant chemotherapy significantly increased the values of RBC, HGB, HCT, MCV, and MCH, while it had no obvious effect on the value of MCHC or RDW.
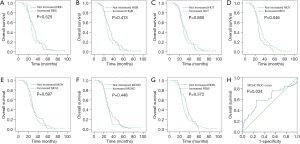
Effects of the whole course of treatment on the values of RBC-related indicators
The effects of the whole course of treatment (surgery plus adjuvant chemotherapy) on the values of the RBC-related parameters are presented in Figure 4. The median value of RBC was 4.205×1012/L (4.060×1012/L–4.330×1012/L) before treatment, and 4.130×1012/L (4.005×1012/L–4.239×1012/L) after treatment (P=0.707). The median value of HGB was 129.000 (123.170–134.830) g/L before treatment, and 126.000 (122.839–130.161) g/L after treatment (P=0.631). The median value of HCT was 0.380 (0.365–0.390) L/L before treatment, and 0.385 (0.370–0.400) L/L after treatment (P=0.083). The median value of MCV was 90.825 (90.265–92.400) fl before treatment, and 91.700 (90.790–93.160) fl after treatment (P=0.005). The median value of MCH was 30.745 (30.001–31.210) pg before treatment, and 30.695 (30.200–31.000) pg after treatment (P=0.225). The median value of MCHC was 337.935 (334.375–341.980) g/L before treatment, and 330.315 (325.240–332.000) g/L after treatment (P=0.026). The median value of RDW was 12.900% (12.635–13.100%) before treatment, and 13.640% (13.500–13.940%) after treatment (P=0.000). The whole course of treatment significantly decreased the value of MCHC and increased the values of MCV and RDW, whereas it had no obvious effects on the values of RBC, HGB, HCT, or MCH.

Changes in MCV level after the whole course of treatment could predict outcomes of resectable GC patients
The Kaplan-Meier plots were used to determine the effects of changes of RBC, HGB, HCT, MCV, MCH, MCHC, and RDW status on OS (Figure 5A,B,C,D,E,F,G). The median OS of patients whose RBC level increased following the whole course of treatment was 26 months (95% CI, 24.387–27.613), while that of the not-increased group was 31 months (95% CI, 26.885–35.115) (P=0.525). The median OS of patients whose HGB level increased following the whole course of treatment was 26 months (95% CI, 23.040–28.960), while that of the not-increased group was 31 months (95% CI, 26.896–35.104) (P=0.413). The median OS of patients whose HCT level increased following the whole course of treatment was 27 months (95% CI, 25.323–28.677), while that of the not-increased group was 30 months (95% CI, 23.141–36.859) (P=0.885). The median OS of patients whose MCV levels increased following the whole course of treatment was 31 months (95% CI, 27.336–34.664), while that of patients with decreased MCV was 26 months (95% CI, 25.038–26.962) (P=0.046). The median OS of patients whose MCH level increased following the whole course of treatment was 26 months (95% CI, 22.758–29.242), while that of the not-increased group was 28 months (95% CI, 25.376–30.624) (P=0.597). The median OS of patients whose MCHC level increased following the whole course of treatment was 26 months (95% CI, 20.456–31.544), while that of the not-increased group was 28 months (95% CI, 24.886–31.114) (P=0.448). The median OS of patients whose RDW level increased following the whole course of treatment was 26 months (95% CI, 24.247–27.753), while that of the not-increased group was 33 months (95% CI, 28.199–37.801) (P=0.372). Thus, the patients with increased MCV levels had an increased survival ratio. However, changes in RBC, HGB, HCT, MCH, MCHC, and RDW levels had no effects on OS.
Prognostic factors for resectable GC
Univariate analysis demonstrated that lymphonodus metastasis (N2) [hazard ratio (HR) 2.116; 95% CI, 1.316–3.403; P=0.002], AJCC stage (III) (HR, 2.764; 95% CI 1.641–4.657; P=0.000), and low pretreatment MCHC levels (HR, 1.704; 95% CI 1.138–2.549; P=0.010) were significant risk factors for a worse prognosis (Table 2). In multivariate analysis, AJCC stage (III) (HR, 3.518; 95% CI, 1.054–11.744; P=0.041) and low pretreatment MCHC levels (HR, 1.705; 95% CI, 1.124–2.586; P=0.012) were found to be independently associated with worse survival.
Table 2
| Risk factors | OS | ||||
|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | ||||
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| Gender (female or male) | 0.714 (0.457-1.115) | 0.139 | – | – | |
| Age (>60 or ≤60 years) | 1.015 (0.992–1.038) | 0.192 | – | – | |
| Tumor size (>5 or ≤5 cm) | 0.848 (0.538–1.337) | 0.478 | – | – | |
| Depth of invasion (T3–4 or T1–2) | 2.062 (0.745–5.705) | 0.164 | – | – | |
| Lymphonodus metastasis (N2 or N0–1) | 2.116 (1.316–3.403) | 0.002** | 0.803 (0.251–2.569) | 0.712 | |
| AJCC stage (III or I–II) | 2.764 (1.641–4.657) | 0.000** | 3.518 (1.054–11.744) | 0.041* | |
| Pre-treatment HGB (≤129.000 or >129.000 g/L) | 0.995 (0.668–1.482) | 0.980 | – | – | |
| Pre-treatment HCT (≤0.380 or >0.380 L/L) | 0.940 (0.632–1.401) | 0.940 | – | – | |
| Pre-treatment MCV (≤90.825 or >90.825 fl) | 1.123 (0.762–1.655) | 0.557 | – | – | |
| Pre-treatment MCH (≤30.745 or >30.745 pg) | 1.195 (0.807–1.768) | 0.374 | – | – | |
| Pre-treatment MCHC (≤337.935 or >337.935 g/L) | 1.704 (1.138–2.549) | 0.010* | 1.705 (1.124–2.586) | 0.012* | |
| Pre-treatment RDW (≤12.900% or >12.900%) | 1.049 (0.708–1.553) | 0.813 | – | – | |
| Pre-treatment RBC (≤4.205×1012/L or >4.205×1012/L) | 0.887 (0.595–1.324) | 0.559 | – | – | |
| Post/pre-treatment HGB ratio (≤1 or >1) | 0.852 (0.575–1.264) | 0.426 | – | – | |
| Post/pre-treatment HCT ratio (≤1 or >1) | 0.972 (0.655–1.443) | 0.888 | – | – | |
| Post/pre-treatment MCV ratio (≤1 or > 1) | 1.484 (0.993–2.217) | 0.054 | 1.258 (0.833–1.900) | 0.275 | |
| Post/pre-treatment MCH ratio (≤1 or >1) | 0.903 (0.611–1.333) | 0.607 | – | – | |
| Post/pre-treatment MCHC ratio (≤1 or >1) | 0.852 (0.558–1.303) | 0.461 | – | – | |
| Post/pre-treatment RDW ratio (≤1 or >1) | 0.815 (0.513–1.294) | 0.386 | – | – | |
| Post/pre-treatment RBC ratio (≤1 or >1) | 0.883 (0.596–1.309) | 0.536 | – | – | |
*, P<0.05; **, P<0.01. GC, gastric cancer; OS, overall survival; HR, hazard ratio; CI, confidence interval; RBC, red blood cell; OS, overall survival; HGB, hemoglobin; HCT, hematocrit; MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; RDW, RBC distribution width; AJCC, American Joint Committee on Cancer.
Specificity and sensitivity of baseline parameters on predicting resectable GC
The receiver operating characteristic (ROC) curve analysis (Figure 5H) showed that the area under the curve (AUC) for predicting resectable GC of MCHC was 0.621 (95% CI, 0.509–0.733; P<0.034). The optimal cutoff point of MCHC was 341.98 g/L, with a sensitivity of 58.3% and a specificity of 75.0%.
Discussion
RBC is a part of person’s complete blood count, and it can circulate in blood and carry oxygen throughout the body (4). A long-term retrospective study indicated that low RBC levels could predict poor survival in postoperative patients with liver cancer (19). Another analysis has indicated that the low RBC level of deglycating enzymes could be implicated in malignant colon mucosal transformation (20). The underlying mechanism was reported by Quemener et al. (21). He showed that alterations in RBC rheological properties could result in hemolysis, which was common in cancer-bearing hosts. In turn, the products of hemolysis were related to the advanced/aggressive nature of cancers. Our present study revealed that neither surgery nor the whole course of treatment had significant effects on serum RBC level, while adjuvant chemotherapy significantly increased the value of RBC. Likewise, neither the amount of pretreatment nor the RBC post-/pretreatment ratio had an effect on OS.
HGB was proposed as an independent prognostic factor for survival in a variety of malignancies. Low HGB concentration could indicate impaired outcomes for patients with carcinoma of the bladder (22), endometrium (23), and ovaries (24). As indicated in a previous report by Grimm et al. (25), HGB level could be decreased by inflammatory cytokines, which were released by tumor cells and might be able to decrease erythropoietin production and shorten the survival of RBCs. In the current study, we found no association between pretreatment HGB levels and the outcome of resectable GC patients. Surgery significantly decreased the value of HGB. On the contrary, chemotherapy significantly increased the value of HGB, making the HGB value remain stable during the whole course of treatment. Change in HGB level represented by post-/pre-treatment HGB had no significant impact on OS.
HCT is the proportion of blood volume that is occupied by red blood anemia, and is usually part of a complete blood count (26). Previous reports have demonstrated that a low HCT level was relevant to worse survival in many cancer diseases, including renal cell carcinoma (27) and breast cancer (26). Hypoxia was one of the underlying mechanisms in which HCT functioned as a prognostic factor for malignant diseases (26). Due to the reduced oxygen-carrying capacity, oxygen delivery reduces at a lower HCT level and further leads to the production of hypoxia (28). Meanwhile, the parallel relationship between cancer progression and hypoxia was reported (29). In the present study, although surgery and the whole course of treatment had no significant effect on the value of HCT, adjuvant chemotherapy could increase the HCT levels. We also found that neither the pretreatment nor the post-/pre-treatment ratio of HCT could affect OS on resectable GC patients.
MCV refers to the volume of RBCs. It has been long recognized as a biomarker for a variety of malignant diseases, like esophageal squamous cell carcinoma (30) and colorectal cancer (31). To our knowledge, MCV is a marker of internal folate concentration. Zheng et al. demonstrated that the deficiency of folate could result in aberrant DNA methylation, which has been proposed as a predictor of clinical outcome in cancer patients (30). In our study, we found that the pretreatment of MCV levels did not affect the OS of resectable GC patients. The whole course of treatment significantly increased the levels of MCV. Chemotherapy might have led to the upregulation of MCV, because surgery had no impact on MCV status. In contrast to earlier studies, we found that patients with increased MCV levels had increased survival ratio.
MCH is a measurement of the average HGB content of each RBC (11). One small-scale retrospective study revealed that a low MCH level was associated with worse survival in hepatectomized patients with hepatocellular carcinoma (11), and MCH was shown to be a marker of iron metabolism. As demonstrated in previous reports, abnormalities in iron metabolism might be crucial in cancer progression (32,33). In the present study, surgery significantly decreased the value of MCH, while chemotherapy significantly increased the value, leaving MCH values unchanged during the whole course of treatment. However, pretreatment MCH levels and post-/pre-treatment ratio of MCH had no significant effects on OS.
MCHC is calculated by dividing the MCH by the MCV and can reflect the average value of HGB concentration (12). A retrospective study was conducted and demonstrated that lower MCHC level was associated with unfavorable prognosis of resectable lung cancer (12). It is well known that MCHC is one of the key indicators of anemia, a frequent complication of cancer patients (4). Tumor cells produce anemia by secreting soluble molecules such as interleukin-1, interferon-ÿ, and tumor necrosis factor that may cause hemolysis, erythropoiesis suppression, and erythropoietin response deficiency on progenitor erythroid cells (12). Thus, it is not surprising to find out the parallel association between low MCHC and worse outcomes in cancer patients. Consistent with previous studies, our study showed that high pretreatment MCHC levels predicted better outcomes of resectable GC patients. The whole course of treatment significantly reduced MCHC rates. The decline of MCHC was mainly attributable to surgery, since chemotherapy had no impact on MCHC status. Both univariate and multivariate analyses demonstrated that low pretreatment MCHC level was one of the independent risk factors in early GC patients. Moreover, the ROC curve analysis showed that the pretreatment MCHC value of 341.98 g/L was considered to be the optimal cutoff value for prognosis, with a sensitivity of 58.3% and a specificity of 75.0%.
RDW is one of the most common blood parameters, which reflects the degree of heterogeneity of erythrocyte volume (also known as anisocytosis) (34). Accumulated evidence indicates that RDW could be a prognostic factor for various malignancies, like gastric (35), lung (13), and ovarian cancers (36). RDW has been reported to have a close association with many pathophysiological conditions, such as anemia, inflammation, and early nutritional deficiencies via changes in erythropoiesis (37). To the best of our knowledge, cancer can induce chronic inflammation and malnutrition (37). Also, anemia is another frequent complication in cancer patients (4). These findings reflect a widely accepted hypothesis that increased RDW level could be a marker of worse outcomes in cancer patients. Our study found that the whole course of treatment increased the level of RDW, and this change mainly resulted from surgery since chemotherapy had no impact on RDW status. However, no significant association was found between survival and pretreatment or the post/pre-treatment ratio of RDW.
A few limitations in this study should be addressed. First, this is a retrospective analysis, and the data were collected from only a single medical center. Secondly, although all measurements were taken in the same laboratory, a certain bias arising from the long study period cannot be completely excluded. Finally, the case number was insufficient.
In conclusion, our present study investigated the predictive values of RBC-related indicators in resectable GC patients and found that high pretreatment MCHC levels were a favorable predictor of OS. In comparison, both the univariate analysis and the multivariate analysis showed that the low level of MCHC pretreatment was an independent risk factor impacting OS. Since MCHC is an inexpensive and easily accessible indicator, our findings offer a new and valuable clue to evaluating prognosis in resectable GC.
Acknowledgments
Funding: This work was supported by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2020.03.46). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethics approval for the study was granted by the Medical Ethics Committees of the First Affiliated Hospital of Soochow University [No. (2019)015]. Informed consent was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Du DX, Lian DB, Amin BH, et al. Long non-coding RNA CRNDE is a novel tumor promoter by modulating PI3K/AKT signal pathways in human gastric cancer. Eur Rev Med Pharmacol Sci 2017;21:5392-8. [PubMed]
- Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 2010;376:687-97. [Crossref] [PubMed]
- Pasechnikov V, Chukov S, Fedorov E, et al. Gastric cancer: prevention, screening and early diagnosis. World J Gastroenterol 2014;20:13842-62. [Crossref] [PubMed]
- Peng F, Hu D, Lin X, et al. The monocyte to red blood cell count ratio is a strong predictor of postoperative survival in colorectal cancer patients: the Fujian prospective investigation of cancer (FIESTA) study. J Cancer 2017;8:967-75. [Crossref] [PubMed]
- Zhang F, Cheng F, Cao L, et al. A retrospective study: the prevalence and prognostic value of anemia in patients undergoing radiotherapy for esophageal squamous cell carcinoma. World J Surg Oncol 2014;12:244. [Crossref] [PubMed]
- Dubray B, Mosseri V, Brunin F, et al. Anemia is associated with lower local-regional control and survival after radiation therapy for head and neck cancer: a prospective study. Radiology 1996;201:553-8. [Crossref] [PubMed]
- Sun J, Wang Y, Yang J, et al. Long-term and stable correction of uremic anemia by intramuscular injection of plasmids containing hypoxia-regulated system of erythropoietin expression. Exp Mol Med 2012;44:674-83. [Crossref] [PubMed]
- Rodríguez-Morales AJ, Sánchez E, Arria M, et al. Haemoglobin and haematocrit: the threefold conversion is also non valid for assessing anaemia in Plasmodium vivax malaria-endemic settings. Malar J 2007;6:166. [Crossref] [PubMed]
- Solak Y, Yilmaz MI, Saglam M, et al. Mean corpuscular volume is associated with endothelial dysfunction and predicts composite cardiovascular events in patients with chronic kidney disease. Nephrology (Carlton) 2013;18:728-35. [Crossref] [PubMed]
- Bhattathiri VN. Relation of erythrocyte and iron indices to oral cancer growth. Radiother Oncol 2001;59:221-6. [Crossref] [PubMed]
- Huang P, Liu C, Li B, et al. Preoperative mean corpuscular hemoglobin affecting long-term outcomes of hepatectomized patients with hepatocellular carcinoma. Mol Clin Oncol 2016;4:229-36. [Crossref] [PubMed]
- Qu X, Zhang T, Ma H, et al. Lower mean corpuscular hemoglobin concentration is associated with unfavorable prognosis of resected lung cancer. Future Oncol 2014;10:2149-59. [Crossref] [PubMed]
- Koma Y, Onishi A, Matsuoka H, et al. Increased red blood cell distribution width associates with cancer stage and prognosis in patients with lung cancer. PLoS One 2013;8:e80240. [Crossref] [PubMed]
- Shimada H, Takiguchi N, Kainuma O, et al. High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer 2010;13:170-6. [Crossref] [PubMed]
- Shimada H, Nabeya Y, Okazumi S, et al. Elevation of preoperative serum C-reactive protein level is related to poor prognosis in esophageal squamous cell carcinoma. J Surg Oncol 2003;83:248-52. [Crossref] [PubMed]
- Shimada H, Oohira G, Okazumi S, et al. Thrombocytosis associated with poor prognosis in patients with esophageal carcinoma. J Am Coll Surg 2004;198:737-41. [Crossref] [PubMed]
- Nakajima K, Suzuki T, Shimada H, et al. Detection of preoperative serum anti-p53 antibodies in gastric cancer. Tumour Biol 1999;20:147-52. [Crossref] [PubMed]
- Nakajima K, Ochiai T, Suzuki T, et al. Impact of preoperative serum carcinoembryonic antigen, CA 19-9 and alpha fetoprotein levels in gastric cancer patients. Tumour Biol 1998;19:464-9. [Crossref] [PubMed]
- Xie X, Yao M, Chen X, et al. Reduced red blood cell count predicts poor survival after surgery in patients with primary liver cancer. Medicine (Baltimore) 2015;94:e577. [Crossref] [PubMed]
- Notarnicola M, Caruso MG, Tutino V, et al. Low red blood cell levels of deglycating enzymes in colorectal cancer patients. World J Gastroenterol 2011;17:329-33. [Crossref] [PubMed]
- Quemener V, Bansard JY, Delamaire M, et al. Red blood cell polyamines, anaemia and tumour growth in the rat. Eur J Cancer 1996;32A:316-21. [Crossref] [PubMed]
- Huang P, Lan M, Peng AF, et al. Serum calcium, alkaline phosphotase and hemoglobin as risk factors for bone metastases in bladder cancer. PLoS One 2017;12:e0183835. [Crossref] [PubMed]
- Tamussino KF, Gücer F, Reich O, et al. Pretreatment hemoglobin, platelet count, and prognosis in endometrial carcinoma. Int J Gynecol Cancer 2001;11:236-40. [Crossref] [PubMed]
- Obermair A, Handisurya A, Kaider A, et al. The relationship of pretreatment serum hemoglobin level to the survival of epithelial ovarian carcinoma patients: a prospective review. Cancer 1998;83:726-31. [Crossref] [PubMed]
- Grimm T, Buchner A, Schneevoigt B, et al. Impact of preoperative hemoglobin and CRP levels on cancer-specific survival in patients undergoing radical cystectomy for transitional cell carcinoma of the bladder: results of a single-center study. World J Urol 2016;34:703-8. [Crossref] [PubMed]
- Chen B, Dai D, Tang H, et al. Pretreatment hematocrit is superior to hemoglobin as a prognostic factor for triple negative breast cancer. PLoS One 2016;11:e0165133. [Crossref] [PubMed]
- Seda CJ, Salas AS, Sánchez CG, et al. Thrombocytosis and hematocrit as prognostic factors in renal carcinoma. Arch Esp Urol 2011;64:883-90. [PubMed]
- Habler OP, Messmer KF. Tissue perfusion and oxygenation with blood substitutes. Adv Drug Deliv Rev 2000;40:171-84. [Crossref] [PubMed]
- Szkandera J, Gerger A, Liegl-Atzwanger B, et al. Pre-treatment anemia is a poor prognostic factor in soft tissue sarcoma patients. PLoS One 2014;9:e107297. [Crossref] [PubMed]
- Zheng YZ, Dai SQ, Li W, et al. Prognostic value of preoperative mean corpuscular volume in esophageal squamous cell carcinoma. World J Gastroenterol 2013;19:2811-7. [Crossref] [PubMed]
- Nagai H, Yuasa N, Takeuchi E, et al. The mean corpuscular volume as a prognostic factor for colorectal cancer. Surg Today 2018;48:186-94. [Crossref] [PubMed]
- Wu XN, Su D, Wang L, et al. Roles of the hepcidin-ferroportin axis and iron in cancer. Eur J Cancer Prev 2014;23:122-33. [Crossref] [PubMed]
- Heath JL, Weiss JM, Lavau CP, et al. Iron deprivation in cancer--potential therapeutic implications. Nutrients 2013;5:2836-59. [Crossref] [PubMed]
- Salvagno GL, Sanchis-Gomar F, Picanza A, et al. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci 2015;52:86-105. [Crossref] [PubMed]
- Yazici P, Demir U, Bozkurt E, et al. The role of red cell distribution width in the prognosis of patients with gastric cancer. Cancer Biomark 2017;18:19-25. [Crossref] [PubMed]
- Li Z, Hong N, Robertson M, et al. Preoperative red cell distribution width and neutrophil-to-lymphocyte ratio predict survival in patients with epithelial ovarian cancer. Sci Rep 2017;7:43001. [Crossref] [PubMed]
- Hirahara N, Matsubara T, Kawahara D, et al. Prognostic value of hematological parameters in patients undergoing esophagectomy for esophageal squamous cell carcinoma. Int J Clin Oncol 2016;21:909-19. [Crossref] [PubMed]


