
Using T stage and tumor thrombosis as predictive factors for patients with resected I–IIA small cell lung cancer: a retrospective study
Introduction
Lung cancer is the leading cause of cancer-related death both nationally and internationally (1,2). Based on its biological behavior and morphological characteristics, lung cancer can be divided into small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC), with SCLC accounting for 15–20% of all lung cancer cases (3,4). In contrast to NSCLC, few cases of SCLC are diagnosed early, with only 5% of SCLC cases being diagnosed without lymph node involvement or metastasis (5). According to the National Comprehensive Cancer Network (NCCN) and European Society for Medical Oncology (ESMO) guidelines for SCLC, patients with stage I–IIA SCLC can benefit from surgery (6,7). This conclusion was derived from analyzing the National Cancer Database (NCDB) and The Surveillance, Epidemiology, and End Results (SEER) Program databases. Based on data from the NCDB, Yang et al. stated that surgery was the best predictive factor for the survival of patients with I–IIA stages, with lobectomy the preferred choice of surgery (8). Yang et al. also found that surgery followed by adjuvant therapy could improve the long-term survival of patients with early-stage SCLC (9), while Wakeam et al. reported that surgery was the best predictive factor for stage not only I–IIA patient survival but also IIB–IIIA patients. However, these benefits decreased with T stage progression (10).
Data for Asian patients are limited as the NCDB only includes patients from the United States. Zhang et al. performed a retrospective survival analysis with 153 limited-stage SCLC patients and reported that these patients might have benefited from surgery in addition to chemotherapy and radiotherapy (11). Zhang et al. retrospectively reviewed patients with combined SCLC who had undergone surgery in 2 institutions and concluded that adjuvant therapy was associated with significantly improved survival in complete resection and lymphadenectomy patients (12). Other research groups have similarly reported the benefits of surgery in limited-stage SCLC patients (13,14). These latter 2 studies reported the clinical benefits of surgery and adjuvant chemotherapy in limited stage SCLC, but due to the low number of patients with stage I/II SCLC in these studies, which are based on Asian populations, it was mostly patients with stage I–IIIA of the disease who were enrolled. Furthermore, the nature of SCLC would be an important predictive factor for long-term survival or recurrence and/or metastasis, but the 4 studies above did not focus on these specifics. According to data from the NCDB, the treatment of stage I/II patients has become standardized, but Chinese practices relating to this treatment were yet to be reported.
Our study was conducted to explore the predictive factors relating to resected stage I/II SCLC concerning overall survival (OS) and time to tumor progression (TTP).
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/tcr-21-525).
Methods
Patients
This was a retrospective, single-center study that reviewed patient surgical records between January 1st, 2014, and December 30th, 2016, at the Shanghai Chest Hospital. Inclusion criteria were as follows: (I) Patients with stage I–IIA SCLC were selected according to the eighth edition of the tumor, nodes, and metastasis (TNM) classification (15); (II) Each patient had undergone preoperative evaluation for staging included brain, thorax, and abdomen computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET) scanning. A bronchoscopy or a mediastinoscopy had also been performed before each operation to exclude patients with known metastasis, (III) Complete patient records of staging, surgical procedures, pathology findings, adjuvant treatment, and follow-up results were available for review. The exclusion criteria were: (I) Patients who had undergone an incomplete resection or died within 1 month of surgery due to postoperative complications; (II) Patients who were not followed up after surgery. The clinical characteristics, pathological diagnoses, and treatment records of the SCLC patients were recorded. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by The Ethics Committee of Shanghai Chest Hospital (KS1752). All included patients signed informed consent documentation.
Follow-up
The adjuvant therapy, including adjuvant chemotherapy, had been administered as advised by the treating clinician, but some patients refused to undergo adjuvant treatment. As our study focused on the predictive factors that may influence the long-term survival of patients with stage I SCLC, the details of each surgery and follow-up adjuvant therapy were recorded. Adjuvant therapy included adjuvant chemotherapy, adjuvant radiotherapy, and prophylactic cranial irradiation (PCI). On average, the patients visited their doctor every 3–6 months. The examinations collectively included: a chest CT scan, B-ultrasonic examination of the abdomen and supraclavicular lymph nodes, MRI, and single-photon emission computed tomography (SPECT) bone scan. If patients did not attend their follow-up appointment, a telephone call was arranged to collect the required details. All metastatic and/or recurrence sites were recorded.
Statistical analysis
For this study, normally distributed continuous variables are presented as the mean ± standard deviation (SD), otherwise as to the median and range, while categorical variables are presented as numbers and percentages. TTP is defined as the period from the date of surgery to the date of detection of the first metastatic or recurrence site, and OS is defined as the period from the date of surgery to the date of death. Univariate analysis was used to estimate the above factors, including age, sex, surgery type, and adjuvant therapy status. Statistically significant factors and other clinical factors considered noteworthy were examined by multivariate analysis. The proportional hazards model was applied in univariate and multivariate analysis, with all tests being two-sided. P<0.05 was considered statistically significant. All analyses were performed using Statistical Package for the Social Sciences (SPSS) software (version 22.0; IBM-SPSS, Inc., Chicago, IL, USA).
Results
A total of 67 patients with pathological T1-2aN0M0 SCLC were initially enrolled in this study. Among them, 1 patient died of pulmonary embolism after surgery, 5 patients were excluded due to missing adjuvant therapy data, and 2 patients were excluded because of incomplete follow-up consultations. In total, 59 patients were included in this study (Figure 1). Most patients were male, older than 60, had undergone lobe and s, and did not have cancer emboli or nerve or vascular invasions. Most patients had received standard adjuvant chemotherapy, with only a small number of patients being given adjuvant radiotherapy or PCI. Details are presented in Table 1.
Table 1
| Item | Group | No. (%) |
|---|---|---|
| Total | 59 | |
| Age (years) | Median 65 (range: 41–82) | |
| >60 | 44 (74.6) | |
| ≤60 | 15 (25.4) | |
| Sex | Male | 52 (88.1) |
| Female | 7 (11.9) | |
| T stage | T1 | 30 (50.8) |
| T2 | 29 (49.2) | |
| Tumor size (cm) | Median 2.5 (range: 0.7–5) | |
| Lesion location | Left upper lobe | 20 (33.9) |
| Left lower lobe | 7 (11.9) | |
| Whole Left lobe | 1 (1.7) | |
| Right upper lobe | 20 (33.9) | |
| Right lower lobe | 11 (18.6) | |
| Operative type | Lobe resection | 46 (80.0) |
| Wedge resection | 10 (16.9) | |
| Sleeve resection | 2 (3.4) | |
| Whole resection | 1 (1.7) | |
| Pathology | Pure | 34 (57.6) |
| Combined | 25 (42.3) | |
| Surgical margin | Positive | 0 (0) |
| Negative | 59 (100.0) | |
| Tumor thrombus | Present | 3 (5.1) |
| Absent | 56 (94.9) | |
| Nerve invasion | Present | 1 (1.7) |
| Absent | 58 (98.3) | |
| Vascular invasion | Present | 1 (1.7) |
| Absent | 58 (98.3) | |
| Adjuvant chemotherapy | Yes (≥4 cycle) | 43 (72.9) |
| Yes (<4 cycle) | 6 (10.2) | |
| Yes (unclear cycle) | 4 (6.8) | |
| No/Chinese herb | 6 (10.1) | |
| Adjuvant radiotherapy | Yes | 6 (10.1) |
| No | 53 (89.9) | |
| Prophylactic cranial irradiation | Yes | 4 (6.8) |
| No | 55 (93.2) |
The median length of time for patient follow-up was 53.7 months, with 17 patients showing recurrence or metastasis. Among them, 12 patients showed single-site metastasis or recurrence, and the rest showed multiple-site recurrence and/or metastasis (Table 2). Eight patients died. The 3-year disease free and 3-year OS rates were 62.5% and 75.0%, respectively. Neither the median TTP and median OS rates nor the 5-year disease free and 5-year OS rates were reached.
Table 2
| Item | Group | Number |
|---|---|---|
| Number | Single | 12 |
| Multiple | 5 | |
| Location | Lung | 3 |
| Pleura | 2 | |
| Intrapulmonary lymph node | 2 | |
| Liver | 2 | |
| Bone | 3 | |
| Brain | 6 | |
| Adrenal gland | 3 | |
| Subcutaneous nodule | 1 | |
| Retroperitoneal lymph nodes | 1 | |
| Lymph node | 1 |
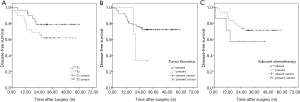
Univariate analysis was then conducted to explore the potential predictive factors of the recurrence and/or metastasis or OS of SCLC. Patient sex, age, surgery type, pathology, tumor (T) stage, evidence of tumor thrombus, if they had received either adjuvant chemotherapy, adjuvant chest radiotherapy, or PCI were recorded in the univariate analysis (Table 3). In contrast, no parameters for TTP were considered statistically significant (i.e., P<0.05), a lower T stage, absence of tumor thrombus, and administration of adjuvant chemotherapy showed a trend towards a longer patient TTP (Figure 2), while only adjuvant chemotherapy showed evidence for a longer patient OS (Figure 3).
Table 3
| Predictor | Time to progress | Overall survival | |||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | ||
| Sex, male vs. female | 1.025 | 0.234, 4.494 | 0.974 | 1.014 | 0.132, 8.209 | 0.970 | |
| Age, ≤60 vs. >60 y | 1.092 | 0.356, 3.348 | 0.878 | 0.863 | 0.229, 3.254 | 0.828 | |
| Surgery, lobectomy vs. non-lobectomy | 0.805 | 0.262, 2.469 | 0.704 | 1.131 | 0.243, 5.261 | 0.875 | |
| Pathology, non-combined vs. combined | 1.517 | 0.585, 3.933 | 0.391 | 1.049 | 0.320, 3.444 | 0.937 | |
| T stage, T2 vs. T1 | 2.157 | 0.797, 5.837 | 0.130 | 1.215 | 0.382, 4.100 | 0.712 | |
| Tumor thrombus, present vs. absent | 2.493 | 0.556, 10.967 | 0.227 | 2.103 | 0.269, 16.459 | 0.479 | |
| Adjuvant chemotherapy, present vs. absent | 0.384 | 0.110, 1.341 | 0.134 | 0.353 | 0.076, 1.641 | 0.184 | |
| Adjuvant chemotherapy, standard vs. other | 0.535 | 0.198, 1.448 | 0.218 | 0.567 | 0.166, 1.939 | 0.366 | |
| Adjuvant chest radiotherapy, present vs. absent | 1.221 | 0.279, 5.344 | 0.791 | 0.718 | 0.092, 5.624 | 0.752 | |
| Prophylactic cranial irradiation, present vs. absent | 0.044 | 0.000, 94.079 | 0.424 | 0.044 | 0.000, 734.887 | 0.529 | |
HR, hazard ratio; CI, confidence interval.
Finally, a multivariate analysis was conducted. Based on the results of the univariate analysis, the following were included: Evidence of recurrence and/or metastasis, T stage, tumor thrombus status, adjuvant chemotherapy, and adjuvant chest radiotherapy status, surgical history, pathology, and PCI status. Only T stage and tumor thrombus status showed statistical significance in the multivariate analysis (P<0.05), while adjuvant chemotherapy trended towards a longer TTP (P=0.059). SCLC patients with a higher T stage and present tumor thrombus and who had received no adjuvant chemotherapy had a higher likelihood of recurrence and/or metastasis (Table 4). Multivariate analysis was not conducted for OS, as adjuvant chemotherapy was the only significant factor in the univariate analysis.
Table 4
| Predictor | Time to progress | ||
|---|---|---|---|
| HR | 95% CI | P value | |
| T stage, T2 vs. T1 | 3.210 | 1.012, 10.175 | 0.048 |
| Tumor thrombus, present vs. absent | 6.021 | 1.057, 34.277 | 0.043 |
| Adjuvant chemotherapy, absent vs. present | 3.425 | 0.953, 12.346 | 0.059 |
HR, hazard ratio; CI, confidence interval.
Discussion
Surgery for early-stage SCLC is still considered controversial. Thus far, only 2 randomized clinical trials have explored the role of surgery in SCLC treatment (16,17), with the trials concluding that surgery was not the optimal treatment option for SCLC. However, this evidence may be limited as not all patients attached to these trials underwent complete resection. Moreover, the surgery in these 2 trials was based on retrospective data. Badzio et al. and Stish et al. suggested that a surgical resection could achieve reasonable treatment outcomes for well-selected patients with early stages of the disease (18,19), and Zhang et al. reported the same results based on their center’s observations (11). Other groups have also reassessed the role of surgery in SCLC treatment based on information located on databases, such as Yang, who found that stage I–IIA patients could benefit from surgery, while adjuvant chemotherapy would further improve survival rate (8,9). Another 2 research groups found that patients with stage I and II SCLC would benefit from surgery (20,21). Based on those same studies, the NCCN guidelines suggest surgery for patients with stage I–IIA SCLC (6,22), but only 1 out of every 3 patients with stage I and II SCLC currently receive surgery (10). SCLC quickly metastasizes in early stages (23), and Thomas et al. observed that about 25% of clinical stage I patients developed more severe forms of the disease following surgery due to lymph node involvement (24,25). As such, the NCCN guidelines recommend the staging of mediastinal lymph nodes before surgery. Furthermore, Takenaka et al. also concluded that surgical resection was effective for Asian patients with stage I SCLC and some cases of stage II–III of the disease (26).
We were neither aware of any research specifically focused on Asian patients with stage I–II resected SCLC nor had we previously been able to identify any predictive factors relating to the survival of Asian patients. Moreover, because guidelines tend to originate from Western countries, data on the Asian population was lacking. Therefore, we explored the predictive factors of stage I/II SCLC relating to surgical procedures. Despite the mean follow-up duration of patients in this study is 53.7 months, the median TTP or the median OS was not reached.
During follow-up appointments, it was noted that single-site recurrence and/or metastasis was more common. Furthermore, intrathoracic recurrence and/or metastasis occurred more frequently at other sites, and these results were consistent with the results of a previous study (19). The disease-free rate in our study was high as patients were in their third postoperative year, with I–IIA stages of the disease, and most had received adjuvant chemotherapy. Moreover, univariate and multivariate analyses were undertaken to explore the predictive factors of OS and indications of recurrence and/or metastasis. A patient’s T stage, tumor thrombus status and adjuvant chemotherapy status were all seen as good indicators of predicting disease outcomes. To explain further, worse outcomes were expected for T2 stage patients compared to those with T1 as it is associated with a more serious tumor burden. The absence of a tumor thrombosis acted as a negative factor in recurrence and/or metastasis, and in patients with NSCLC, a tumor thrombosis is believed to be a predictor of poor prognosis as it is regarded as a prerequisite for tumor invasion of the vascular system or lymph node metastasis (27,28). Some studies have even suggested that tumor thromboses should be considered in TNM staging (29). Although adjuvant chemotherapy showed no statistical significance, it showed a tendency for a longer TTP, and studies conducted by Yang (9,30), Zhang (12), and Zhang (11) confirm the benefits of adjuvant chemotherapy following surgery for patients with early-stage SCLC. In univariate and multivariate analysis of OS, only adjuvant chemotherapy was seen to improve patient prognosis. It is suggested that the benefits of OS may come from a longer TTP (31,32).
Our study supposes that parameters, such as type of surgery (lobe resection or other), pathology (pure or combined), nerve invasion, vascular invasion, adjuvant radiotherapy, and PCI status were not related to recurrence and/or metastasis or OS. Some of these factors were regarded as showing correlation with OS orTTP, while other treatment options have been viewed as more controversial (33). In some studies, lobe resection was reported to be associated with a longer OS than other types of surgery (34,35). Zhang et al. indicated that the combined components of NSCLC would affect the OS (12), while Weckler BC suggests that complete resection was the only predictor of OS (36). However, in patients with NSCLC, nerve invasion or vascular invasion have also influenced the OS (37,38). In our study, most enrolled patients had received a lobectomy, showed absence of nerve or vascular invasion, and had not undergone an R1 resection. Due to the small number of patients, we did not find predictive values relating to operation type or nerve or vascular invasion.
The brain and thorax are the main sites of recurrence and/or metastasis after SCLC surgery. Therefore, the role of chest radiotherapy and PCI are frequently discussed as treatment options following an SCLC resection. Yang et al. suggested that PCI should be included in adjuvant therapy in patients with stage I–II SCLC (9), with Wang also having made similar suggestions based on their patients of combined SCLC (39). However, Xu et al. has speculated that PCI was unnecessary for patients with resected stage I SCLC (40). In our study, no clinical benefits of PCI were found. Yu et al. reported that adjuvant chest radiotherapy did not improve the OS in patients with stage I SCLC (41), while Varlotto et al. drew the same conclusion using information from the SEER database (35). In our study, only 6 of 59 patients received adjuvant radiotherapy, and we found that this factor did not affect the likelihood of recurrence and/or metastasis or patient OS.
Our study has some limitations. First, as it was a single-center study with relatively small sample size, some selection bias was inevitable. Second, due to the low number of resected SCLC patients, the number of patients available for enrollment was limited. Third, the statistical results of some subgroups (e.g., PCI group) should be interpreted with caution due to this limited number of included patients.
In summary, it was found that T stage, tumor thrombus status, and adjuvant chemotherapy status could affect the TTP in patients with resected stage I SCLC, while adjuvant chemotherapy was the only predictor of OS. Although the number of enrolled patients was relatively small, we believe that this study has provided important evidence concerning Asian patients sharing the same predictive factors. More data on Asian populations with SCLC has been produced by Western countries, especially discussing patients who had undergone stage I–IIA SCLC resections. These results could have potential applications for clinical practice and should be validated by further investigation.
Acknowledgments
The authors would like to acknowledge the support of the Department of Pathology of Shanghai Chest Hospital. We also thank the patients and their families for their contributions.
Funding: This work was support by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/tcr-21-525
Data Sharing Statement: Available at https://dx.doi.org/10.21037/tcr-21-525
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/tcr-21-525). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by The Ethics Committee of Shanghai Chest Hospital (KS1752). All included patients signed informed consent documentation.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 2015;10:1243-60. [Crossref] [PubMed]
- Fisseler-Eckhoff A, Demes M. Neuroendocrine tumors of the lung. Cancers (Basel) 2012;4:777-98. [Crossref] [PubMed]
- Lüchtenborg M, Riaz SP, Lim E, et al. Survival of patients with small cell lung cancer undergoing lung resection in England, 1998-2009. Thorax 2014;69:269-73. [Crossref] [PubMed]
- NCCN Guidelines—Small Cell Lung Cancer 2021,V3. Available online: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1462
- Früh M, De Ruysscher D, Popat S, et al. Small-cell lung cancer (SCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013;24:vi99-105. [Crossref] [PubMed]
- Yang CJ, Chan DY, Shah SA, et al. Long-term Survival After Surgery Compared With Concurrent Chemoradiation for Node-negative Small Cell Lung Cancer. Ann Surg 2018;268:1105-12. [Crossref] [PubMed]
- Yang CF, Chan DY, Speicher PJ, et al. Role of Adjuvant Therapy in a Population-Based Cohort of Patients With Early-Stage Small-Cell Lung Cancer. J Clin Oncol 2016;34:1057-64. [Crossref] [PubMed]
- Wakeam E, Acuna SA, Leighl NB, et al. Surgery Versus Chemotherapy and Radiotherapy For Early and Locally Advanced Small Cell Lung Cancer: A Propensity-Matched Analysis of Survival. Lung Cancer 2017;109:78-88. [Crossref] [PubMed]
- Zhang J, Li S, Chen X, et al. Retrospective study of surgery versus non-surgical management in limited-disease small cell lung cancer. Thorac Cancer 2014;5:405-10. [Crossref] [PubMed]
- Zhang C, Yang H, Zhao H, et al. Clinical outcomes of surgically resected combined small cell lung cancer: a two-institutional experience. J Thorac Dis 2017;9:151-8. [Crossref] [PubMed]
- Yin K, Song D, Zhang H, et al. Efficacy of surgery and prophylactic cranial irradiation in stage II and III small cell lung cancer. J Cancer 2018;9:3500-6. [Crossref] [PubMed]
- Chen MY, Hu X, Bao Y, et al. Comparison Of Long Term Results Between Matched Chemoradiotherapy And Surgery For Limited Stage Small Cell Lung Cancer. Cancer Manag Res 2019;11:9049-55. [Crossref] [PubMed]
- Asamura H, Chansky K, Crowley J, et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revision of the N Descriptors in the Forthcoming 8th Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2015;10:1675-84.
- Fox W, Scadding JG. Medical Research Council comparative trial of surgery and radiotherapy for primary treatment of small-celled or oat-celled carcinoma of bronchus. Ten-year follow-up. Lancet 1973;2:63-5. [Crossref] [PubMed]
- Lad T, Piantadosi S, Thomas P, et al. A prospective randomized trial to determine the benefit of surgical resection of residual disease following response of small cell lung cancer to combination chemotherapy. Chest 1994;106:320S-3S. [Crossref] [PubMed]
- Badzio A, Kurowski K, Karnicka-Mlodkowska H, et al. A retrospective comparative study of surgery followed by chemotherapy vs. non-surgical management in limited-disease small cell lung cancer. Eur J Cardiothorac Surg 2004;26:183-8. [Crossref] [PubMed]
- Stish BJ, Hallemeier CL, Olivier KR, et al. Long-Term Outcomes and Patterns of Failure After Surgical Resection of Small-Cell Lung Cancer. Clin Lung Cancer 2015;16:e67-73. [Crossref] [PubMed]
- Jin K, Zhang K, Zhou F, et al. Selection of candidates for surgery as local therapy among early-stage small cell lung cancer patients: a population-based analysis. Cancer Commun (Lond) 2018;38:5. [Crossref] [PubMed]
- Weksler B, Nason KS, Shende M, et al. Surgical resection should be considered for stage I and II small cell carcinoma of the lung. Ann Thorac Surg 2012;94:889-93. [Crossref] [PubMed]
- Verma V, Simone CB 2nd. Surgery Versus Conventional Radiation Therapy for T1-2 N0 M0 Small-cell Lung Cancer: A Fair Comparison? Clin Lung Cancer 2018;19:e69-70. [Crossref] [PubMed]
- Kalemkerian GP, Akerley W, Bogner P, et al. Small cell lung cancer. J Natl Compr Canc Netw 2013;11:78-98. [Crossref] [PubMed]
- Thomas DC, Arnold BN, Rosen JE, et al. Defining outcomes of patients with clinical stage I small cell lung cancer upstaged at surgery. Lung Cancer 2017;103:75-81. [Crossref] [PubMed]
- Saji H, Miyazawa T, Marushima H, et al. Pathological upstaging and treatment strategy of clinical stage I small cell lung cancer following surgery. J Thorac Dis 2017;9:E285-9. [Crossref] [PubMed]
- Takenaka T, Takenoyama M, Inamasu E, et al. Role of surgical resection for patients with limited disease-small cell lung cancer. Lung Cancer 2015;88:52-6. [Crossref] [PubMed]
- Wang Y, Jing L, Wang G. Risk factors for lymph node metastasis and surgical methods in patients with early-stage peripheral lung adenocarcinoma presenting as ground glass opacity. J Cardiothorac Surg 2020;15:121. [Crossref] [PubMed]
- Tan ZK, Casipit P, Pandit NS. PO-10 - Lung cancer with tumour thrombosis: a poor prognosticator. Thromb Res 2016;140:S180. [Crossref] [PubMed]
- Tsuchiya T, Hashizume S, Akamine S, et al. Upstaging by vessel invasion improves the pathology staging system of non-small cell lung cancer. Chest 2007;132:170-7. [Crossref] [PubMed]
- Yang CJ, Chan DY, Speicher PJ, et al. Surgery Versus Optimal Medical Management for N1 Small Cell Lung Cancer. Ann Thorac Surg 2017;103:1767-72. [Crossref] [PubMed]
- Hoda MA, Klikovits T, Klepetko W. Controversies in oncology: surgery for small cell lung cancer? It's time to rethink the case. ESMO Open 2018;3:e000366. [Crossref] [PubMed]
- Veronesi G, Bottoni E, Finocchiaro G, et al. When is surgery indicated for small-cell lung cancer? Lung Cancer 2015;90:582-9. [Crossref] [PubMed]
- Low M, Ben-Or S. Thoracic Surgery in Early-Stage Small Cell Lung Cancer. Thorac Surg Clin 2018;28:9-14. [Crossref] [PubMed]
- Combs SE, Hancock JG, Boffa DJ, et al. Bolstering the case for lobectomy in stages I, II, and IIIA small-cell lung cancer using the National Cancer Data Base. J Thorac Oncol 2015;10:316-23. [Crossref] [PubMed]
- Varlotto JM, Recht A, Flickinger JC, et al. Lobectomy leads to optimal survival in early-stage small cell lung cancer: a retrospective analysis. J Thorac Cardiovasc Surg 2011;142:538-46. [Crossref] [PubMed]
- Weckler BC, Baldes N, Schirren J. Survival following Multimodality Treatment Including Surgery for Stage IA-IIIB Small-Cell Lung Cancer. Thorac Cardiovasc Surg 2019;67:291-8. [Crossref] [PubMed]
- Maeda R, Yoshida J, Ishii G, et al. Prognostic impact of intratumoral vascular invasion in non-small cell lung cancer patients. Thorax 2010;65:1092-8. [Crossref] [PubMed]
- Ramnefjell M, Aamelfot C, Helgeland L, et al. Vascular invasion is an adverse prognostic factor in resected non-small-cell lung cancer. APMIS 2017;125:197-206. [Crossref] [PubMed]
- Wang Y, Xu J, Han B, et al. The role of prophylactic cranial irradiation in surgically resected combined small cell lung cancer: a retrospective study. J Thorac Dis 2018;10:3418-27. [Crossref] [PubMed]
- Xu J, Yang H, Fu X, et al. Prophylactic Cranial Irradiation for Patients with Surgically Resected Small Cell Lung Cancer. J Thorac Oncol 2017;12:347-53. [Crossref] [PubMed]
- Yu JB, Decker RH, Detterbeck FC, et al. Surveillance epidemiology and end results evaluation of the role of surgery for stage I small cell lung cancer. J Thorac Oncol 2010;5:215-9. [Crossref] [PubMed]




