
Primary malignant pericardial mesothelioma with a survival of 2.5 years: a case report
Introduction
Primary malignant pericardial mesothelioma (PMPM) is a highly malignant tumor originating from pericardium serosum with a prevalence rate of less than 0.002%. There are many risk factors for this disease, including exposure to asbestos, post-radiation, and possible viral infection (simian virus 40) (1-3). Previous studies have reported positive autopsy rates of 0.006–0.0022% (4,5). Clinical manifestations include constrictive pericarditis, pericardial tamponade, and heart failure (6). Confirmation of the diagnosis relies on histopathological examination (4). Malignant pericardial mesothelioma is clinically rare with a poor prognosis and an average survival time of 6–10 months (7). There is a lack of effective treatment, and patients are promptly treated with surgery and postoperative adjuvant chemotherapy to improve their quality of life and prolong survival (8,9). The patient reported in this case had a survival of 2.5 years, whereas previous studies of the disease found a mean survival of 6–10 months and a maximum survival of 2 years. Consider prolongation of patient survival in relation to other symptomatic supportive treatments. This has not been discussed in other cases. We present the following study in accordance with the CARE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-778/rc).
Case presentation
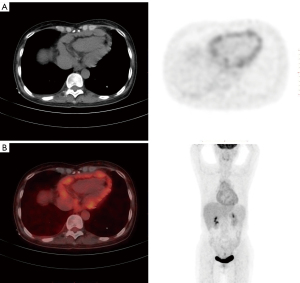
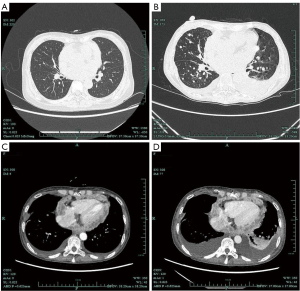
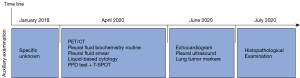
A 57-year-old female presented with chest tightness and panic in January 2018 with no apparent cause. The patient denied exposure to asbestos, post-radiation, possible viral infection, or other harmful substances. She was hospitalized in a local hospital with a suspected diagnosis of tuberculous pericarditis, and subsequently given anti-tuberculosis treatment for 1 year, which was discontinued upon symptomatic relief. In April 2020, the patient presented again with chest tightness. The positron emission tomography/computed tomography (PET/CT) examination suggested anterosuperior mediastinum occupancy, multiple lymph nodes (some with necrosis) in the mediastinum and top of the lateral septum, noticeable thickening of the pericardium with multiple nodules, tending towards tuberculosis, and localized encapsulated effusion in the pericardium (Figure 1). Pleural fluid biochemistry routine showed the following: yellow exudation with predominantly mononuclear, normal adenosine deaminase (ADA), no tumor cells on pleural fluid smear and liquid-based cytology, PPD test ++, and T-SPOT. After the diagnosis of tuberculous pericarditis, paroxysmal supraventricular tachycardia and radiofrequency ablation, the patient was again treated with anti-tuberculosis and metoprolol tartrate to lower the ventricular rate, and was discharged when her symptoms were relieved. Following discharge from the hospital until June 2020, she sought medical attention again for recurrent chest tightness, and echocardiogram showed the following: (I) small left and right ventricular internal diameters with restricted ventricular wall motion; (II) small amount of mitral regurgitation, medium amount of tricuspid regurgitation and micro regurgitation of pulmonary valve; (III) increased echogenicity in the pericardial cavity with viscous fluid inside (Figure 2); (IV) thickened pericardium with enhanced echogenicity. Pleural ultrasound (bilateral chest) showed bilateral pleural effusion. Lung tumor markers showed CA125: 140.5 U/mL↑, CYFRA21-1: 7.02 ng/mL↑, and pleural fluid carcinoembryonic antigen with 1.08 ng/mL. After continuing anti-tuberculosis treatment, it was found that the treatment effect was not good. The patient underwent a partial pericardial resection on July, 2020 with a postoperative pathological diagnosis of (pericardial) malignant mesothelioma (Figure 3). At the same time, complications such as chest tightness, shortness of breath, palpitations at rest, frequent arrhythmias, heart failure, cardiogenic shock, and multiple serosal cavity effusions. Chest CT revealed pericardial thickening and progressive enhancement with multiple metastatic lesions in the lungs (Figure 4). After discussing treatment plans and considering the prognosis, the patient opted for palliative care. Although the patient has been in a state of extreme fatigue for a long time, the patient has been treated for complications, symptomatic and supportive treatment and meticulous care after surgery, such as improving cardiac function, pleural effusion drainage, ascites drainage, nutritional support, bedsore care, psychological counseling, etc. way to prolong the lifespan. Overall, patients survived 2.5 years since onset and 1 year postoperatively. The timeline and auxiliary examination are shown in Figure 5. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.


Discussion
This case report describes a case of primary malignant pericardial mesothelioma with a survival of 2.5 years. This case has some points for discussion, as follows: (I) The most commonly misdiagnosed disease in PMPM is tuberculous pericarditis, where both pericardial lesions are similar, presenting as constrictive pericarditis, with pericardial tamponade and heart failure(6). When patients with pericardial effusion present with poor antitubercular concurrent with rapid effusion growth, the possibility of malignant mesothelioma of the pericardium needs to be considered, despite its low incidence and clinical rarity. (II) Low detection rate of pericardiocentesis fluid exfoliation cytology (10). The diagnosis of PMPM is often made via pathological surgical procedures or histopathological examinations with a particular disease location. Although the imaging is not specific, X-ray chest radiographs are related to tumor location, size, pericardial effusion, and pleural metastasis (11); local CT showing thickened, single, or multiple nodular shadows of varying size within the pericardium with clear borders, involving the pleura or lungs. The diffuse form mainly presents soft tissue-filled shadows within the pericardium, encasing the heart and producing atrial and ventricular compression changes. It is accompanied by a variable amount of bloody pericardial effusion, with slightly higher CT values. Enhanced CT allows observation of tumor aggressiveness and determination of the size and extent of the mass (1), while echocardiography has a diagnostic compliance rate of only 20% (4). (III) The low detection rate of pericardiocentesis exfoliative cytology cannot be used as an exclusion criterion in the presence of negative results. (IV) Therefore, it needs to be differentiated from pleural mesothelioma pericardial metastases: the primary focus is mostly bloody and exudative, with thickened and rough pleura, and the metastatic collection is yellowish, leaking fluid with a smooth plasma membrane surface (4). (V) Confirmation of the diagnosis relies on histopathological examination. Reactive mesothelial hyperplasia is morphologically indistinguishable from mesothelioma cells. Positive immunohistochemistry of IMP-3, Ki-67, and GLUT-4 help in the identification of PMPM (4).
This case shows that although clinical manifestations and non-invasive examination are very important for the diagnosis of PMPM, it is still a diagnosis of exclusion due to its rarity, non-specific symptoms and signs, and diverse imaging manifestations, and the diagnosis depends on cytology and histology. Physical examination. The detection rate of pericardiocentesis fluid stripping cytology is low. Repeated search can improve the detection rate, but it may be missed. Pathological diagnosis of pericardial tissue is a powerful means of diagnosis, and immunohistochemistry can improve the diagnostic accuracy and reduce the misdiagnosis rate. Although PMPM is a highly malignant disease, the survival time of this case was prolonged by means of treatment of complications, symptomatic and supportive care, and meticulous care. Therefore, we should not lose hope for such patients, and palliative care is also Not necessarily a bad choice. With the advancement of medicine, it is believed that there will be better treatment methods to prolong the survival time of such patients in the future.
The strength of this case report is that this patient survived for 2.5 years, suggesting that our survival time for this disease may not be limited to the time of reporting of existing cases. The limitation is that only one patient is included, the number of cases is small, and there may be uniqueness of individual cases. The etiology and risk factors of this patient are unclear.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-778/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-778/coif). The authors have no conflicts of interest to declare
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tian L, Xie D. A case of primary pericardial malignant mesothelioma. Imaging Diagnosis and Interventional Radiology 2016;25:433-4.
- Martínez-Girón R, Liron P. Sudden cardiac death due to primary malignant pericardial mesothelioma: brief report and literature review. Respir Med Case Rep 2019;26:185-8. [Crossref] [PubMed]
- Mensi C, Romano A, Berti A, et al. A second case of pericardial mesothelioma mimicking systemic lupus erythematosus in the literature in over 30 years: a case report . J Med Case Rep 2017;11:85-90. [Crossref] [PubMed]
- Kong L, Wang J, Sun L, et al. Misdiagnosis analysis of 164 cases of primary malignant pericardial mesothelioma in mainland China. Journal of Clinical Cardiovascular Diseases 2017;33:348-52.
- Kawakami N, Kawai M, Namkoong H, et al. Cardiac tamponade due to primary malignant pericardial mesothelioma diagnosed with surgical pericardial resection. J Cardiol Cases 2021;24:149-52. [Crossref] [PubMed]
- Savarrakhsh A, Vakilpour A, Davani SZ, et al. Malignant primary pericardial mesothelioma presenting as effusive constrictive pericarditis: a case report study. J Cardiothorac Surg 2021;16:298. [Crossref] [PubMed]
- Wang S, Li T, Zou Y, et al. Imaging manifestations of pericardial malignant mesothelioma Journal of Molecular Imaging 2019;42:473-5.
- Seal S, Simon H. Primary Pericardial Mesothelioma: A Rare but Serious Consideration. Cureus 2021;13:e19966. [Crossref] [PubMed]
- Karagodin I, Nagle K, Scheidemantle B, et al. Metastatic pericardial mesothelioma: a rare case of constrictive pericarditis. J Am Coll Cardiol 2019;73:2640-7. [Crossref]
- Zhang Z, Wu D, Xiao H, et al. Primary malignant pericardial mesothelioma: a case report. Chin J Med 2021;32:627-8.
- Kong L, Wang J, Sun L, et al. Primary malignant pericardial mesothelioma in China: clinical, imaging, pathological and prognostic analysis. Chinese Journal of Circulation 2017;32:1005-9.


