
Comparing the efficacy and safety of cement-augmented fenestrated pedicle screws and conventional pedicle screw in surgery for spinal metastases: a retrospective comparative cohort study
Highlight box
Key findings
• CAPS is effective and safe in the surgical operation of spinal metastatic tumors.
What is known and what is new?
• In surgery for spinal metastases, pedicle screw internal fixation can restore spinal stability.
• Proximal segmental metastases often occur after CPS, leading to spinal instability and even failure of internal fixation, recurrent symptoms.
• Bone cement can strengthen the vertebrae, and kill tumors.
• CAPS is a new type of screw, which can strengthen the vertebral body and reduce the probability of internal fixation failure in patients undergoing surgery with osteoporosis.
What is the implication, and what should change now?
• By applying CAPS, whether it is possible to reduce the incidence of near level metastasis, thereby improving patient symptoms and reducing spinal instability and internal fixation failure.
Introduction
In recent years, the incidence of cancer patients with bone metastasis has shown an annually increasing trend (1). The spine is the most common site of metastasis. Bone destruction and spinal cord compression caused by spinal metastasis often lead to severe bone pain and neurological dysfunction. Effective spinal cord decompression surgery is needed to relieve the symptoms (2). Combined pedicle screw fixation can maintain or reconstruct the spinal stability (3,4). However, with the advancement of medical treatment for malignant tumors, the survival time of patients with spinal metastases is being gradually prolonged, and adjacent segment vertebral metastases often occur after conventional pedicle screw (CPS) surgery. The study has shown that some patients with spinal metastases have adjacent segment vertebral metastases with the development of the disease, resulting in Tomita type 7 spinal metastases (5), postoperative pain, and neurological dysfunction for a second time. Meanwhile, osteolytic bone destruction caused by metastasis of adjacent vertebral body segments may also lead to failure of internal fixation, resulting in the recurrence of spinal instability, which may require revision surgery.
There are various scoring systems for preoperative evaluation of surgical methods for spinal metastases, including the Tomita score (6), the modified Tokuhashi score (7), Tomita classification (8), Weinstein-Boriani-Biagini (WBB) classification (9), spinal instability neoplastic score (SINS) (10), neurologic, oncologic, mechanical stability, and systemic disease (NOMS) score (11) and Harrington score (12). According to various kinds of scores and types, total en-bloc spondylectomy (TES) surgery can achieve the purpose of local radical resection and reduce the local recurrence rate for patients with an expected survival time of more than 1-year, solitary oligometastases, and poor spinal stability (13,14). The polymethylmethacrylate (PMMA)-augmented fenestrated screws/cement-augmented pedicle screw (CAPS) is a new type of pedicle screw with a hollow type and lateral hole, which can inject bone cement into the vertebral body through the tail of the screw after screw implantation. Through the anchoring effect of bone cement, the fixation effect of the pedicle screw can be enhanced, the stability of the screws can be improved, and the probability of the screw loosening and pulling out can be reduced (15). The screw was originally used in spinal surgery in patients with osteoporosis to prevent the failure of internal fixation caused by bone loss of screw-implanted segments (16). Biomechanical tests showed that it had a good anti-pullout effect, and it was safe and effective in surgical models of osteoporosis and revision of failure after spinal internal fixation (17). In addition, the thermal and chemical effects of PMMA during the coagulation process can effectively destroy tumor cells and inhibit the progression of spinal metastases. Studies have found that the application of cement-enhanced pedicle screws in surgical operations for spinal metastases can effectively reduce the pain symptoms of patients and improve their quality of life (18,19). However, there is a paucity of reports on whether the CAPS group can be used in the surgery of spinal metastases to reduce screw loosening caused by osteolytic destruction, prevent adjacent segment vertebral metastasis, and improve local control rate. In other word, the efficacy and safety of CAPS in the separation surgery for spinal metastases need to be explored.
The purpose of separation surgery for spinal metastatic tumors is to quickly relieve pain and spinal cord compression and maintain or reconstruct spinal stability to enable a safe distance for postoperative radiotherapy. As a result, the risk of radiation-induced spinal cord injury could be reduced, and the efficacy of radiotherapy would be improved. Maintaining long-term and effective spinal stability and local control of the surgical segments of spinal metastases are important evaluation criteria for surgical efficacy. It is of great significance to explore the application prospects of CAPS in the separation surgery for spinal metastases.
In this study, patients with spinal metastases who underwent posterior separation were retrospectively analyzed and divided into two groups according to the application of CAPS or CPS during operation. The clinical, imaging, and pathological data, duration of operation, the amount of bleeding and complications, pain, and neurological function before and after surgery were compared between the two groups. In addition, the local control and progression-free survival (PFS) time of the patients after surgery were followed up. Therefore, the main goals of the study were to (I) identify the efficacy of CAPS in the separation surgery of spinal metastases; (II) evaluate the safety of CAPS, and (III) provide a reference for the clinical application of CAPS. We present the following article in accordance with the STROBE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2631/rc).
Methods
Participants
A retrospective study was conducted to investigate the efficacy and safety of cement-augmented fenestrated pedicle screws in the posterior approach for spinal metastases. Patients with spinal metastases who underwent posterior separation surgery and pedicle screw internal fixation in the Department of Orthopedics of The Fourth Hospital of Hebei Medical University from January 2017 to August 2019 were enrolled. A total of 52 cases were collected, including 25 males and 27 females, with an average age of 57.9±8.9 (range, 36–72) years. There were 19 cases of primary lung cancer, 12 renal carcinoma, 8 esophageal cancer, 4 colorectal cancer, 3 gastric cancer, 3 breast cancer, 2 liver cancer, 1 ovarian cancer; 24 thoracic vertebrae, and 28 lumbar vertebrae; 23 cases of a single segment and 29 cases of adjacent 2 or more segments. Patients were divided into the CAPS group (28 cases) and the CPS group (24 cases). The CAPS group comprised 13 males and 15 females. The CPS group comprised 12 males and 12 females. This study was approved by the Ethics Committee of The Fourth Hospital of Hebei Medical University (No. 2021KY339), and all the patients signed the informed consent form. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
The inclusion criteria were as follows: (I) patients with spinal metastasis of malignant tumor confirmed by puncture pathology preoperatively; (II) an expected survival time more than 3 months; (III) treated with posterior separation surgery combined with CAPS or CAPS for internal fixation; (IV) patients with varying degrees of pain, neurological dysfunction, and spinal instability. The endpoint for observation was a local progression, loss of follow-up, or death.
The exclusion criteria were as follows: (I) patients without pathological diagnosis before surgery, pain or neurological injury, spinal instability, or bone metastasis which caused severe destruction of adjacent multi-segmental bone, and the inability to implant screws; (II) poor general condition to tolerate the surgery; (III) the postoperative follow-up time was less than 3 months.
Surgical indications
Patients with preoperative systemic and local imaging evaluation showing that there were multiple metastatic bone metastases or other treatable visceral metastases, obvious spinal cord compression and spinal instability, and palliative decompression and spinal stability reconstruction were deemed suitable for this intervention.
Preoperative preparation
The general condition and cardiopulmonary function were routinely evaluated before surgery. The expected bleeding volume was assessed according to the conditions of primary tumors, and 2–4 units of red blood cells and 200–400 mL of plasma were selectively prepared.
Surgical methods
All surgeries were performed by the same surgical team in the Department of Orthopedics, The Fourth Hospital of Hebei Medical University. The posterior median approach was used to expose the spinous process and lamina of the affected vertebrae and 1–2 segments above and below the affected vertebrae. Pedicle screws were implanted through the pedicles of 1–2 segments above and below the affected vertebrae. A total of 28 patients were treated with CAPS (CEOXEN, WEGO, Weihai, China), and 24 patients were treated with CPS (UPASS5.5, WEGO). The diameters of pedicle screws in both groups were 5.5, 6.0, and 6.5 mm, and the lengths were 4.0 and 4.5 cm. The separation surgery was performed as follows: the posterior structures such as spinous process, ligament, and lamina were removed, and the lateral and anterior compression tissues of the dura mater were removed by entering the bilateral pedicles of the affected vertebrae. Circumferential decompression was fully performed for the spinal cord so that there was a 2–3 mm interval between the spinal cord and the anterior residual vertebrae. Of all the patients, 22 patients (39.3%) used dural patches for obstruction, and 21 patients (40.4%) underwent combined affected segmental vertebroplasty before circumferential decompression. For patients in the CAPS group, bone cement was injected into the tail of the screw, and the process was monitored by C-arm X-ray fluoroscopy.
Postoperative treatment
Patients were placed in the routine supine position after the operation. The drainage tube was removed when the daily drainage volume was less than 50 mL, the brace was used for the activity to get out of bed 24–48 hours after removal, and computed tomography (CT) was conducted to reexamine the operative segments. All patients were treated with standard bisphosphate drugs after the operation, and appropriate chemotherapy, endocrine therapy, or targeted drug therapy were selected according to different primary lesions. After surgery, 73.1% of the patients received radiotherapy for the operative segments of the affected vertebrae.
Evaluation indicators
Tomita score and Tokuhashi score were used to evaluate the expected survival time of patients in the two groups. A visual analog scale (VAS) was used to evaluate the pain of the patients, in which 1–3 points indicated mild pain, 4–6 points indicated moderate pain, and 7–10 points indicated severe pain. The neurological function injury was evaluated by Frankel grading, which included grades A to E. The degree of spinal instability was evaluated by the SINS score according to the preoperative imaging.
Efficacy
The VAS score and Frankel grade of the two groups were recorded before and 3 months after the operation, and the differences between the two groups were compared to evaluate the efficacy of the surgery.
Safety
The operation time, the amount of intraoperative blood loss, the amount of bone cement injected in the pedicle screw group, and the complications of the surgery were recorded to evaluate the safety of CAPS.
Follow-up evaluation
All patients were followed up by outpatient reexamination. The first follow-up was performed 3 months after surgery and was repeated every 3 months. The contents of the reexamination included an X-ray of the surgical site, spinal CT, and magnetic resonance imaging (MRI). A whole-body bone scan was performed every 6 months, and the metastasis was evaluated according to the CT or MRI reexamination of corresponding organs. The endpoint was tumor progression in local and adjacent segments or the death of patients. According to the manifestations of X-ray and CT, as well as the corresponding clinical symptoms, the internal fixation failure (loosening, fracture, or pullout) was evaluated. If the translucent zone around the screw on the CT or screw displacement or fracture compared with that on the first postoperative CT, accompanied by activity pain due to the corresponding segment, it was identified as internal fixation failure. The failure rate of internal fixation was compared between the two groups of patients with different pedicle screws to analyze the efficacy of CAPSs. For the evaluation of local tumors, according to the re-examination of X-ray, CT, and MRI, the increase of local soft-tissue shadow, bone destruction, or aggravation of pathological fracture in the operative segment was identified as local tumor progression. The new abnormal signal, new bone destruction, or aggravation of the original bone destruction in the adjacent segments were identified as the tumor progression in the adjacent segments. When the tumor progression occurred in the surgical or adjacent segment, it was regarded as local progression, that is, the endpoint of observation. The time of loss of follow-up, death, and local progression was recorded. The differences in local PFS time between the two groups were compared, and the effect of different pedicle screws on the local control rate was analyzed.
Statistical analysis
The software SPSS 21.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. The measurement data were tested for normality at first, the data with normal distribution were expressed by mean ± standard deviation (SD), and the paired t-test was used for comparison between groups. The data that did not conform to the normal distribution was represented by the median (interquartile range), and the comparison between groups was performed by the nonparametric Mann-Whitney U test. The counting data were expressed by percentage, and the chi-square test was used for comparison between groups. The difference in local PFS between the two groups was calculated by the Kaplan-Meier (K-M) survival curve. A two-sides P value <0.05 was accepted as a statistically significant difference.
Results
General data of the two groups
There were no significant differences in sex, age, surgical sites, surgical segments, and Tomita classification between the CAPS group and CPS group (all P>0.05, Table 1). The 52 patients had a Tomita score of 5–8 points and a Tokuhashi score of 5–9 points. According to the preoperative imaging, all the patients had different degrees of spinal instability, and the SINS scores were 9–14 points. Therefore, there were no significant differences in the Tomita score, Tokuhashi score, and SINS score between the two groups (all P>0.05, Table 1).
Table 1
| Index | CAPS group (n=28) | CPS group (n=24) | P value |
|---|---|---|---|
| Sex, n | 0.797 | ||
| Male | 13 | 12 | |
| Female | 15 | 12 | |
| Age (years), n | 0.862 | ||
| >60 | 17 | 14 | |
| ≤60 | 11 | 10 | |
| Surgical sites, n | 0.103 | ||
| Thoracic vertebra | 10 | 14 | |
| Lumbar vertebra | 18 | 10 | |
| Surgical segments, n | 0.730 | ||
| Single segment | 13 | 10 | |
| ≥2 segments | 15 | 14 | |
| Tomita classification, n | 0.904 | ||
| IV | 6 | 4 | |
| V | 7 | 6 | |
| VI | 8 | 9 | |
| VII | 7 | 5 | |
| Tomita score, mean ± SD | 6.96±0.84 | 6.88±0.80 | 0.697 |
| Tokuhashi score, mean ± SD | 7.43±0.92 | 7.79±1.06 | 0.193 |
| SINS score, mean ± SD | 11.36±1.52 | 10.75±1.15 | 0.116 |
CAPS, cement-augmented pedicle screw; CPS, conventional pedicle screw; SD, standard deviation; SINS, spinal instability neoplastic score.
Surgical conditions, complications, and postoperative treatment in the two groups
All the surgeries were performed successfully. The average operation time was 163±20 minutes in the CAPS group and 138±18 minutes in the CPS group, with a statistically significant difference (P<0.001, Table 2). The combined intraoperative vertebroplasty was performed in 21 patients (40.4%), which were 12 patients in the CAPS group and 9 patients in the CPS group (P=0.695). The average blood loss was 623±185 mL in the CAPS group and 733±163 mL in the CPS group (P=0.027, Table 2). For the 28 patients in the CAPS group, a total of 218 screws were implanted, with an average of 1.3±0.4 mL bone cement injected into each screw.
Table 2
| Indicator | CAPS group (n=28) | CPS group (n=24) | P value |
|---|---|---|---|
| Operation time (min), mean ± SD | 163±20 | 138±18 | <0.001 |
| Intraoperative blood loss (mL), mean ± SD | 733±163 | 623±185 | 0.027 |
| Postoperative hospital stays, mean ± SD | 8.3±1.4 | 7.7±1.0 | 0.086 |
| Intraoperative vertebroplasty, n | 0.695 | ||
| Yes | 12 | 9 | |
| No | 16 | 15 | |
| Postoperative cerebrospinal fluid leakage, n | 0.935 | ||
| Yes | 1 | 1 | |
| No | 27 | 24 | |
| Postoperative radiotherapy, n | 0.772 | ||
| Yes | 20 | 18 | |
| No | 8 | 6 |
CAPS, cement-augmented pedicle screw; CPS, conventional pedicle screw; SD, standard deviation.
The occurrence rate of postoperative cerebrospinal fluid leakage in the CAPS group, and CPS group was 3.6% (1 to 28) and 4.2% (1 to 24), respectively (P=0.935, Table 2). Prone position, intermittent clamping, and drainage were applied, and the incisions achieved primary healing without hematoma formation, infection, and other complications. There was no significant difference in the occurrence rate of postoperative complications between the two groups. No symptomatic pulmonary cement embolism (PCE) occurred in the CAPS group. The average postoperative hospital stay was 8.3±1.4 days in the CAPS group and 7.7±1.0 days in the CPS group, with no significant difference (P=0.086, Table 2). The postoperative radiotherapy was performed in 20, and 18 patients in the CAPS group and CPS group, respectively, with no significant difference between the two groups (P=0.772, Table 2).
Efficacy and follow-up of CAPS treatment
The preoperative VAS scores of the two groups were 5.79±1.81 and 6.00±2.04, respectively, with no significant difference between the two groups (P=0.704, Table 3). At 3 months after surgery, the VAS scores of the CAPS group and CPS group were 2.93±1.33 and 4.17±1.34, respectively, and the difference between the two groups was statistically significant (P=0.002, Table 3). In addition, the postoperative VAS scores in the two groups were significantly lower than those before the operation (both P<0.001, Table 3).
Table 3
| Indicator | CAPS group (n=28) | CPS group (n=24) | P value |
|---|---|---|---|
| Preoperative VAS score, mean ± SD | 5.79±1.81 | 6.00±2.04 | 0.704 |
| Postoperative VAS score, mean ± SD | 2.93±1.33* | 4.17±1.34* | 0.002 |
| Preoperative Frankel grade, n | 0.796 | ||
| A, B | 12 | 11 | |
| C, D | 16 | 13 | |
| Postoperative Frankel grade, n | 0.752 | ||
| A, B | 3 | 3 | |
| C, D | 18 | 13 | |
| E | 7 | 8 | |
| Failure of internal fixation, n | 0.011 | ||
| Yes | 1 | 7 | |
| No | 27 | 17 | |
| Adjacent segmental metastasis, n | 0.017 | ||
| Yes | 2 | 8 | |
| No | 26 | 16 |
*, compared with preoperative VAS score, P<0.001. CAPS, cement-augmented pedicle screw; CPS, conventional pedicle screw; VAS, visual analogue scale; SD, standard deviation.
As for the recovery of neurological function injury, the Frankel grading in 84.6% (22/52) of patients recovered at least 1 grade 3 months after the operation, but there was no significant difference in Frankel grades between the two groups before and after the operation (all P>0.05, Table 3).
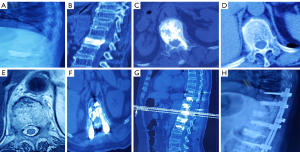
Postoperative imaging of all patients showed that the position of pedicle screws was satisfactory (Figure 1). Bone cement leakage occurred in 2 patients (7.1%) in the CAPS group, all leaked into the anterior vertebral venous plexus, and no leakage into the posterior spinal canal. During the follow-up period, the failure rate of internal fixation for all patients was 15.4% (8/52), including 1 case in the CAPS group and 7 cases in the CPS group, and the difference was statistically significant (P<0.05, Table 3). All patients were followed up for an average of 15.9±5.2 (range, 6–24) months. During the follow-up period, there were 16 cases of local progression (10 cases of adjacent segmental metastasis or progression, 6 cases of tumor progression in situ, Table 3); 4 cases were lost for follow-up. The 6-month local control rate was 98.1% (51/52), and the 12-month local control rate was 65.4% (34/52). There was a significant difference in local PFS between the two groups (P<0.05, Figure 2).

Discussion
Ensuring long-term and effective spinal stability is an important method to evaluate the curative effect of spinal metastases separation surgery, and it is of great clinical significance to explore the application of cement-reinforced pedicle screw in spinal metastasis separation surgery. In this study, we confirmed that CAPSs are effective in reducing the pain and adjacent segmental metastasis of spinal malignancy, the failure rate of internal fixation, as well as prolonging the local PFS time of patients.
Efficacy and safety of CAPS
In previous studies, CAPS were widely used in spinal surgery in patients with osteoporosis to improve screw fixation strength and reduce the incidence of internal fixation failure. Ghermandi et al. (20) performed 53 operations on 52 patients, and 247 CAPS were implanted. The results showed that CAPS could be used in tumor patients, including revision surgery, osteoporosis, and bone destruction. Chandra et al. (21,22) applied CAPS combined with open transforaminal lumbar interbody fusion (O-TLIF) or minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) interbody fusion in patients with osteoporosis combined with lumbar spondylolisthesis, and achieved good results, satisfactory pain relief, and effective interbody fusion. Yuan et al. (23) treated 27 patients with continuous osteoporosis by CAPS fixation guided by 3D navigation, which included 8 cases of thoracolumbar fracture, 18 cases of spinal degeneration, and 1 case of revision. Except for 1 patient who died of postoperative pneumonia, the average improvement rate of the Japanese Orthopedic Association (JOA) score was 39.6%. Within 12 months, postoperative follow-up showed that 20 patients had bone fusion (bone fusion rate was 76.9%). No screw loosening was found, indicating that PMMA-enhanced thoracolumbar pedicle screw fixation guided by 3D navigation positively affected patients with osteoporosis. Karaca et al. followed up on 55 patients with CAPS fixation. Postoperative imaging showed bone cement leakage in 7 patients (12.7%), asymptomatic PCE in 3 patients (5.4%), and deep incision infection in 3 patients (5.4%) (24). Choy et al. (25) found, by CT scanning, in a patient with severe kyphosis after pedicle screw fixation that the augmentation of bone cement was limited to the end of the screw, and there was loosening and halo around the pedicle screw body. Moreover, there was evidence that the screw had pulled out, thus bringing the risks and benefits of spinal fusion with CAPS fixation into question. Although the occurrence rate of this phenomenon was low, the indications should be carefully considered in the application of CAPS fixation. In addition, due to the lack of a tap expansion channel and the process of balloon dilatation, the injection of bone cement into the vertebral body through a pedicle screw under high pressure may increase the probability of bone cement entering the blood, which leads to PCE. Ulusoy et al. (26) observed the application of CAPS in 281 patients with spinal deformity and found that the overall incidence of radiological PCE was 16.3%. The incidence of symptomatic PCE was 1.4%. When the number of screws was ≥7, the risk of symptomatic PCE increased significantly. When the number of screws was >14 and the dosage of cement was more than 20–25 cc, it may lead to increased pulmonary artery pressure and right ventricular dilatation. A recent retrospective study enrolled 69 patients who underwent open posterior surgery with a total of 502 cement-augmented screws, found that there was no screw loosening, pullout, or failure. The rate of cement extravasation was 28.9% (27). Also, they found that cement extravasation did not cause symptoms except in 1 patient who developed a symptomatic thoracic radiculopathy requiring decompression. There was 1 case of asymptomatic PCE.
This study found that the overall failure rate of internal fixation in the patients during the follow-up period was 15.4%. It was considered that with the progression of spinal metastases, the severe collapse of the vertebral body of the surgical segment led to the aggravation of kyphosis or metastasis of adjacent screw segments, eventually resulting in screw loosening. However, there was only one case of screw loosening caused by adjacent segmental metastasis in the CAPS group. Compared with the CPS group, the occurrence rate of internal fixation failure was significantly lower, and the difference was statistically significant. It is suggested that the CAPS have a good fixation effect. In this study, the patients in the CAPS group had no intraspinal cement leakage and no symptomatic cement embolism, suggesting good safety.
Analysis of the curative effect of CAPS fixation
At present, there are few reports on the application of CAPS in spinal metastases. Sussman et al. (28) treated a patient with bone metastasis with spinal canal decompression, and CAPS internal fixation, which effectively relieved the pain symptoms of the patient. Wu et al. (29) implanted CAPS fixation with the assistance of a spinal robot in a patient with multiple spinal metastases of the breast, which effectively improved the patient’s quality of life. Kim (30) used percutaneous CAPS fixation in 14 patients with spinal metastases. Their results showed that patients’ pain was effectively relieved, which showed that CAPS fixation could provide obvious pain relief and improve the quality of life for some patients with spinal metastases. A recent study revealed that percutaneous cement-augmented carbon fiber reinforced poly-ether-ether-ketone pedicle screw instrumentation facilities artifact-reduced postoperative imaging, while maintaining a risk profile and implant failure rates comparable to those of conventional metallic instrumentation (31).
There were no significant differences in sex, age, surgical sites, and segments between the two groups. The preoperative Tomita classifications were typed IV–VII, Tomita scores were 6–8 points, Tokuhashi scores were 5–9 points, SINS scores were 9–13 points, VAS scores were 2–10 points, and Frankel grading was grade A–D. These parameters were not significantly different between the two groups, indicating that the clinical data of the two groups were consistent with each grading system, and the curative effect can be compared. The expected survival time was shorter, and the stability of the spine was poor, so it was suitable for palliative decompression combined with spinal internal fixation. There was no significant difference in the proportion of patients who underwent vertebroplasty, as well as the amount of bleeding during the operation. However, the operation time was longer in the CAPS group, which was related to the need for multiple fluoroscopies during the injection of cement into the pedicle screw. Patients in both groups were treated with bisphosphate after the operation, and there was no significant difference in the proportion of patients who received postoperative radiotherapy. Pain and neurological function were evaluated 3 months after the operation, and it was found that neurological function was recovered in 84.6% of the patients. There was no statistical difference in Frankel grade between the two groups. The VAS scores were decreased after surgery in the two groups, and it was lower in the CAPS group than that in the CPS group. The difference was statistically significant, suggesting that the surgical decompression in the two groups was effective. The postoperative treatment was standardized, and the recovery of spinal function was good. The patients in the CAPS group had better spinal stability after reconstruction. As a result, there were fewer patients with persistent pain due to spinal instability after the operation.
Effect of CAPS on local control rate
In one study, postoperative additional radiotherapy for patients with spinal metastases was shown to help improve the local control rate of the tumor, but patients with spinal metastases were often complicated with spinal cord compression, and it was difficult to reach the effective radiation dose near the spinal cord lesions (32). In addition, pedicle screws have been shown to interfere with the radiation dose distribution of the vertebral body, resulting in insufficient radiation dose near the vertebral segment of spinal metastases (33). Through the thermal and chemical effects in the process of solidification, bone cement can inhibit the invasion of bone metastases (34).
Cyteval et al. (35) treated 49 patients with vertebral compression fractures by conservative treatment or vertebroplasty with a small amount of bone cement injection, respectively. It was found that there was no significant difference in the new fracture rate 3 months after operation between the two groups, suggesting that a small amount of cement cannot prevent the fracture of adjacent vertebrae. However, for spinal metastases, the dispersion and distribution of bone cement may affect the probability of local recurrence or progression. The bone cement was injected into the vertebral body through the tail of CAPS and dispersed into the vertebral body through the window hole on the side of the screw, which limited the distribution and dispersion of bone cement to a certain extent, and the amount of bone cement injection was limited. In this study, the average amount of cement injected into each screw in the CAPS group was 1.3±0.4 mL. Compared with the CPS group, the adjacent segment metastasis rate was lower, and the local PFS time was significantly prolonged during the follow-up period. It is suggested that CAPS fixation can effectively reduce the incidence of adjacent segment metastasis.
This study also had some limitations. Firstly, it was a retrospective study in a single center. Large-scale, multi-center randomized controlled studies are needed to further confirm the conclusions in this study in the future. Secondly, the sample size of patients was relatively small. We will collect more cases to expand the sample size of patients with spinal metastases treated with CAPS in our center. Thirdly, due to the hollow design, the screws are easy to break. Currently, the application of CAPS that are 5.0 mm or less in diameter is relatively rare, so there is a lack of reports and studies on the application in upper thoracic and cervical vertebrae. In addition, due to the increased times of fluoroscopy in the process of bone cement injection and the relative prolongation of the operation time, we still need to be cautious about complications such as bone cement leakage and PCE.
Conclusions
In conclusion, the application of CAPS in the surgical operation of spinal metastatic tumors has a good effect, which can effectively reduce screw loosening and pull-out, reduce the failure rate of internal fixation, may prevent the occurrence of adjacent segment vertebral metastasis, or possibly improve the local control rate.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2631/rc
Data Sharing Statement: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2631/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2631/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of The Fourth Hospital of Hebei Medical University (No. 2021KY339) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Perez-Garcia J, Muñoz-Couselo E, Cortes J. Bone metastases: Causes, consequences and therapeutic opportunities. EJC Suppl 2013;11:254-6. [Crossref] [PubMed]
- Expert Panel on Radiation Oncology-Bone Metastases. ACR Appropriateness Criteria ® spinal bone metastases. J Palliat Med 2013;16:9-19. [Crossref] [PubMed]
- Siegel GW, Biermann JS, Calinescu AA, et al. Surgical Approach to Bone Metastases. Curr Osteoporos Rep 2018;16:512-8. [Crossref] [PubMed]
- Zhang C, Liu Y. Combined pedicle screw fixation at the fracture vertebrae versus conventional method for thoracolumbar fractures: A meta-analysis. Int J Surg. 2018;53:38-47. [Crossref] [PubMed]
- Elder BD, Lo SF, Holmes C, et al. The biomechanics of pedicle screw augmentation with cement. Spine J 2015;15:1432-45. [Crossref] [PubMed]
- Depreitere B, Ricciardi F, Arts M, et al. Loss of Local Tumor Control After Index Surgery for Spinal Metastases: A Prospective Cohort Study. World Neurosurg 2018;117:e8-e16. [Crossref] [PubMed]
- Westermann L, Olivier AC, Samel C, et al. Analysis of seven prognostic scores in patients with surgically treated epidural metastatic spine disease. Acta Neurochir (Wien) 2020;162:109-19. [Crossref] [PubMed]
- Kwon YM, Kim KS, Kuh SU, et al. Survival rate and neurological outcome after operation for advanced spinal metastasis (Tomita's classification > or = type 4). Yonsei Med J 2009;50:689-96. [Crossref] [PubMed]
- Halm H, Richter A, Lerner T, et al. En-bloc spondylectomy and reconstruction for primary tumors and solitary metastasis of the spine. Orthopade 2008;37:356-66. [Crossref] [PubMed]
- Arana E, Kovacs FM, Royuela A, et al. Spine Instability Neoplastic Score: agreement across different medical and surgical specialties. Spine J 2016;16:591-9. [Crossref] [PubMed]
- Laufer I, Bilsky MH. Advances in the treatment of metastatic spine tumors: the future is not what it used to be. J Neurosurg Spine 2019;30:299-307. [Crossref] [PubMed]
- Davarski AN, Kitov BD, Zhelyazkov CB, et al. Surgical management of metastatic tumors of the cervical spine. Folia Med (Plovdiv) 2013;55:39-45. [Crossref] [PubMed]
- Charest-Morin R, Flexman AM, Srinivas S, et al. Perioperative adverse events following surgery for primary bone tumors of the spine and en bloc resection for metastases. J Neurosurg Spine 2019; Epub ahead of print. [Crossref] [PubMed]
- Cofano F, Di Perna G, Marengo N, et al. Transpedicular 3D endoscope-assisted thoracic corpectomy for separation surgery in spinal metastases: feasibility of the technique and preliminary results of a promising experience. Neurosurg Rev 2020;43:351-60. [Crossref] [PubMed]
- Moon BJ, Cho BY, Choi EY, et al. Polymethylmethacrylate-augmented screw fixation for stabilization of the osteoporotic spine: a three-year follow-up of 37 patients. J Korean Neurosurg Soc 2009;46:305-11. [Crossref] [PubMed]
- Bludau F, Welzel G, Reis T, et al. Phase I/II trial of combined kyphoplasty and intraoperative radiotherapy in spinal metastases. Spine J 2018;18:776-81. [Crossref] [PubMed]
- Zajączkowska R, Kocot-Kępska M, Leppert W, et al. Bone Pain in Cancer Patients: Mechanisms and Current Treatment. Int J Mol Sci 2019;20:6047. [Crossref] [PubMed]
- Hariri O, Takayanagi A, Miulli DE, et al. Minimally Invasive Surgical Techniques for Management of Painful Metastatic and Primary Spinal Tumors. Cureus 2017;9:e1114. [Crossref] [PubMed]
- Patel S, Parola R, Rosinski CL, et al. Fenestrated Pedicle Screws in Spinal Oncology: Technique and Comparative Retrospective Analysis. Int J Spine Surg 2021;15:113-8. [Crossref] [PubMed]
- Ghermandi R, Pipola V, Colangeli S, et al. Polymethylmethacrylate-augmented fenestreted pedicle-screw fixation in low bone quality patients: a case series and literature review. J Biol Regul Homeost Agents 2018;32:71-6. [PubMed]
- Chandra VV, Prasad BC, Jagadeesh MA, et al. Segmental polymethylmethacrylate-augmented fenestrated pedicle screw fixation for lumbar spondylolisthesis in patients with osteoporosis - A case series and review of literature. Neurol India 2017;65:89-95. [PubMed]
- Chandra Vemula VR, Prasad BC, Jagadeesh MA, et al. Minimally invasive transforaminal lumbar interbody fusion using bone cement-augmented pedicle screws for lumbar spondylolisthesis in patients with osteoporosis. Case series and review of literature. Neurol India 2018;66:118-25. [Crossref] [PubMed]
- Yuan Q, Zhang G, Wu J, et al. Clinical evaluation of the polymethylmethacrylate-augmented thoracic and lumbar pedicle screw fixation guided by the three-dimensional navigation for the osteoporosis patients. Eur Spine J 2015;24:1043-50. [Crossref] [PubMed]
- Karaca S, Enercan M, Levent Ulusoy O, et al. Radiologic and clinical outcome of the cement augmented pedicle screws after a minimum 2-year follow-up. Acta Orthop Belg 2019;85:247-52. [PubMed]
- Choy WJ, Walsh WR, Phan K, et al. Technical Note: Pedicle Cement Augmentation with Proximal Screw Toggle and Loosening. Orthop Surg 2019;11:510-5. [Crossref] [PubMed]
- Ulusoy OL, Kahraman S, Karalok I, et al. Pulmonary cement embolism following cement-augmented fenestrated pedicle screw fixation in adult spinal deformity patients with severe osteoporosis (analysis of 2978 fenestrated screws). Eur Spine J 2018;27:2348-56. [Crossref] [PubMed]
- Massaad E, Rolle M, Hadzipasic M, et al. Safety and efficacy of cement augmentation with fenestrated pedicle screws for tumor-related spinal instability. Neurosurg Focus 2021;50:E12. [Crossref] [PubMed]
- Sussman ES, Ho A, Pendharkar AV, et al. Image-guided Percutaneous Polymethylmethacrylate-augmented Spondylodesis for Painful Metastasis in the Veteran Population. Cureus 2019;11:e4509. [Crossref] [PubMed]
- Wu C, Lee CY, Huang TJ, et al. Cement-augmented pedicle screw insertion assisted by spinal robotic systems for widespread spinal metastases. J Robot Surg 2019;13:595-8. [Crossref] [PubMed]
- Kim P, Kim SW. Bone Cement-Augmented Percutaneous Screw Fixation for Malignant Spinal Metastases: Is It Feasible? J Korean Neurosurg Soc 2017;60:189-94. [Crossref] [PubMed]
- Wagner A, Haag E, Joerger AK, et al. Cement-Augmented Carbon Fiber-Reinforced Pedicle Screw Instrumentation for Spinal Metastases: Safety and Efficacy. World Neurosurg 2021;154:e536-46. [Crossref] [PubMed]
- Barragán-Montero AM, Nguyen D, Lu W, et al. Three-dimensional dose prediction for lung IMRT patients with deep neural networks: robust learning from heterogeneous beam configurations. Med Phys 2019;46:3679-91. [Crossref] [PubMed]
- Kim YJ, Kim JH, Kim K, et al. The Feasibility of Spinal Stereotactic Radiosurgery for Spinal Metastasis with Epidural Cord Compression. Cancer Res Treat 2019;51:1324-35. [Crossref] [PubMed]
- Sadeghi-Naini M, Aarabi S, Shokraneh F, et al. Vertebroplasty and Kyphoplasty for Metastatic Spinal Lesions: A Systematic Review. Clin Spine Surg 2018;31:203-10. [Crossref] [PubMed]
- Cyteval C, Thomas E, Solignac D, et al. Prospective evaluation of fracture risk in osteoporotic patients after low cement volume vertebroplasty. J Radiol 2008;89:797-801. [Crossref] [PubMed]
(English Language Editor: J. Jones)


