
The clinicopathological characteristics and survival outcomes of primary expansile vs. infiltrative mucinous ovarian adenocarcinoma: a retrospective study sharing the experience of a tertiary centre
Highlight box
Key findings
• Our study adds to limited existing evidence in the literature comparing characteristics and outcomes of expansile vs. infiltrative primary mucinous ovarian carcinoma (MOC).
What is known and what is new?
• As reported before, infiltrative tumours present at a later age, tend to involve both ovaries and have an advanced International Federation of Gynaecology and Obstetrics stage at diagnosis. Primary MOCs are known to be chemo-resistant to carboplatin-paclitaxel. In our study, patients who received this regime were more likely to relapse.
• Three years progression-free survival was significantly worse in the infiltrative group (94.7% vs. 65.6%). We found a possible association between paired-box gene 8 (PAX8) and expansile MOC.
What is the implication, and what should change now?
• Biomarker-driven therapies are currently being investigated for rare ovarian tumours.
• In the absence of good neoadjuvant chemotherapy or adjuvant treatment option, surgery with maximal cytoreductive effort remains essential in the management of primary MOCs.
• The possible association between PAX8 and expansile MOC may warrant further investigation.
Introduction
Mucinous ovarian carcinomas (MOCs) are rare ovarian tumours accounting for approx. 3% of all epithelial ovarian carcinomas (EOCs) (1). They have a distinct molecular profile, natural history, chemo-sensitivity, and prognosis in comparison to high-grade serous carcinoma (HGSC) and other EOCs (2).
MOC is the most common histological subtype of EOC in women under the age of 40 years (3) and appears to be correlated with tobacco smoking (4) but not with known risk-factors for HGSC such as breast cancer gene (BRCA) mutation, early menarche, late menopause, nulliparity, lack of breastfeeding (2).
Primary MOC is diagnosed at stage 1 in over 80% of cases and early-stage MOC has an excellent prognosis, with more than 90% 5-year overall survival (OS) (5). Mucinous metastatic carcinomas (MMCs) account for approx. 80% of all mucinous ovarian tumours (2) and, in contrast with primary MOCs, have a dismal prognosis with median OS of 11–31 months, depending on the origin of the primary tumour (6).
Primary MOCs have a distinct genetic and molecular profile from other EOCs (7,8). While TP53 mutations are invariably seen in HGCS (9), they are frequent but not ubiquitous in primary MOCs (8). HGSCs lack KRAS mutations and harbour high levels of copy number alterations. MOCs frequently harbour KRAS mutations and fewer gene copy number changes (8). This, as well as the different risk factor profile of the two tumours, suggest that MOC has a different etiology from other epithelial ovarian tumours.
The diagnosis of an invasive mucinous carcinoma requires the detection of stromal invasion of more than 5 mm or more than 10 mm2. Invasion less than these measurements is classified as “micro-invasion” within a borderline mucinous tumour (2). Primary MOCs usually show a continuum of architectural features including benign, borderline, and malignant areas. This heterogeneous aspect indicates a stepwise progression to carcinoma. This histogenesis may be similar to that of primary peritoneal mucinous cystadenocarcinomas (10).
Lee and Scully (11) divided the type of stromal invasion in primary MOC into expansile (non-destructive) and infiltrative (destructive), classification which was adopted by the World Health Organisation (WHO) in 2014 (12). The expansile subtype has no destructive stromal invasion but exhibits confluent and architecturally complex malignant glands with round, convex outer outlines. These glands have a “back-to-back” appearance due to absent or minimal intervening stroma, which does not surround individual glands entirely. The infiltrative subtype is defined by destructive stromal invasion. Typical features are glands with irregular contours, often associated with stromal dysplasia, non-gland forming tumour in solid sheets, small cell clusters, or individual cells, unsystematically infiltrating the stroma (13,14). Figure 1 illustrates histology findings in expansile and infiltrative primary MOC.

Immunohistochemistry (IHC) has been used in distinguishing between primary MOCs and MMCs, as well as in the identification of potential primary sources of an MMC. Unfortunately, IHC does not provide any definitive answers as typically IHC staining is exhibited by multiple tumour types (15). There is no single antibody that can identify the primary source of a tumour with absolute certainty, therefore a panel of various antibodies is usually employed to aid differential diagnosis (16).
There is limited evidence in the literature describing IHC differences between expansile and infiltrative tumours. Hada et al. [2021] found CK 5/6 (P=0.01), CD 24 (P=0.02), and epithelial growth factor receptor (EGFR) (P<0.01) statistically related to infiltrative invasion. The progression-free survival (PFS) (P=0.04) and OS (P=0.02) of EGFR-positive primary MOC were worse than those of EGFR-negative MOC (17).
Division of primary MOC into expansile and infiltrative subtypes allows a better understanding of tumour biology, appropriate therapeutic regimens, and prognosis (13).
Given the rarity of this tumour, few studies to date have compared clinicopathological particularities and outcomes of these two histological types. Our paper adds to the limited existing evidence on this topic.
The aim of this study was to describe patient and tumour characteristics, as well as survival outcomes of expansile and infiltrative primary MOCs. We specifically looked at patient age at diagnosis, tumour size and laterality, IHC markers, International Federation of Gynaecology and Obstetrics (FIGO) stage at diagnosis, PFS and OS. We present this article in accordance with the STROBE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-863/rc).
Methods
This was a descriptive, retrospective cohort study conducted at a tertiary cancer centre (Churchill Hospital, Oxford). Patients had surgery for primary MOC at one of our four regional hospitals (Churchill Hospital, Stoke Mandeville Hospital, Royal Berkshire Hospital, Great Western Hospital) between Jul 1, 2010 and Oct 28, 2022. Their care was discussed at the Gynaecology Oncology multidisciplinary team meeting (MDT) at the Churchill Hospital. All participating hospitals were informed and agreed the study. All histology results were reviewed at the tertiary centre. Patient information was obtained from electronic patient records. This service evaluation protocol was registered in accordance with the Oxford University Hospitals Trust requirements (registration number 7049). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The data collected were anonymised. Informed consent was taken from all patients to allow data collection and analysis for research purposes. No remuneration was offered to the patients enrolled in this study.
Inclusion criteria
Consecutive patients with a diagnosis of MOC, discussed at the Oxford MDT between Jul 2010 and Oct 2022 were included.
Exclusion criteria
We excluded patients who were found to have MMC, patients with a dual histological diagnosis, patients who died before treatment could be initiated, patients where follow-up information could not be obtained.
Data collection
For each patient, the following variables were collected: age, FIGO stage at diagnosis, histological pattern of invasion (expansile vs. infiltrative), laterality (unilateral vs. bilateral tumours), tumour size, IHC, surgical procedure performed, R0 status, adjuvant treatment, recurrence, date of death, cause of death. Tumours were staged using the FIGO 2014 ovarian tumour staging system (18). The following information was obtained from histopathology reports: type of invasion, tumour size, laterality, IHC. The following IHC markers have been employed: CK20, CK7, CK8/18, CEA, CA125, CA19.9, paired-box gene 8 (PAX8), P16, CD-X2. IHC markers were considered “positive” where “patchy”, “focal”, “diffuse” or “strong” positivity were described in the IHC report. The WHO 2014 histological classification of ovarian tumours (12) was used for all tumors. For cases where surgery was performed prior to 2014, the stage of disease and histological type were classified retrospectively based on surgical and pathological assessment. Patients were followed up every 3 months for the first 2 years and then every 6 months up to 5 years after end of treatment. Patients who had adjuvant chemotherapy had alternate appointments with the Gynaecology Oncology and Medical Oncology teams. Recurrence was documented by histological evidence of disease in tumour biopsy or and/or the appearance of new lesions on imaging examination.
Our outcome variables were: patient age, tumour size and laterality, FIGO stage at diagnosis, IHC markers, type of surgery, adjuvant treatment, PFS, and OS. PFS was defined as the time from cytoreductive surgery to the date of recurrence. OS was defined as the time from cytoreductive surgery to the date of death, or to the last follow-up date, if still alive. Any-cause OS was reported.
Statistical analysis
Baseline demographic and clinical characteristics were summarised by continuous and categorical variables. Categorical variables were compared with the Chi-square test. When the assumptions required for Chi-square test were not met, Fisher’s exact test was employed. Differences between continuous variables were analysed with the Independent Student’s t-test. Ordinal variables were analysed using the Kruskall-Wallis non-parametric test. A value of P<0.05 was considered statistically significant. Median follow-up time was calculated using the reversed Kaplan-Meier method. Patient survival was calculated in univariable analysis by the log-rank test and in multivariable analysis by logistic regression (Cox model). Hazard ratios (HR) were reported with their 95% confidence intervals (95% CIs). Survival curves were constructed using the Kaplan-Meier method. SPSS v29.0 was used for statistical analysis.
Results
A total of 47 patients were identified. Fourteen of them were excluded: eight patients were found to have MMC, four patients were lost to follow-up, one patient had exploratory surgery but did not meet the criteria for upfront debulking surgery (UDS) and died before neoadjuvant chemotherapy (NACT) was started. Finally, we excluded one patient who was found to have a dual histological diagnosis of anaplastic carcinoma and primary MOC. This aggressive tumour has been described by our team in a case report (19).
Thirty-three patients with primary MOC and complete records were identified. Twenty-three (70.6%) had an expansile pattern of invasion, while 10 (30.4%) had an infiltrative pattern of invasion.
Patient and tumour characteristics
In Table 1, we have compared patient and tumour characteristics in the expansile vs. infiltrative and no relapse vs. relapse groups.
Table 1
| Variables | Expansile vs. infiltrative groups | No relapse vs. relapse groups | |||||
|---|---|---|---|---|---|---|---|
| Expansile | Infiltrative | P value | No relapse | Relapse | P value | ||
| Patients, n (%) | 23 (69.7) | 10 (30.3) | 29 (87.9) | 4 (12.1) | |||
| Age, years, median [range] | 55 [17–76] | 62 [42–79] | 0.049* | 58 [17–79] | 54 [48–68] | 0.404* | |
| FIGO stage, n (%) | 0.002** | <0.001** | |||||
| Stage I | 22 (95.7) | 5 (50.0) | 27 (93.2) | 0 | |||
| Stage II | 1 (4.3) | 3 (30.0) | 1 (3.4) | 3 (75.0) | |||
| Stage III | 0 | 2 (20.0) | 1 (3.4) | 1 (25.0) | |||
| Laterality | 0.212*** | ||||||
| Unilateral | 22 (95.7) | 8 (80.0) | 28 (96.6) | 2 (50.0) | |||
| Bilateral | 1 (4.3) | 2 (20.0) | 1 (3.4) | 2 (50.0) | 0.033*** | ||
| Tumour size, cm, mean [range] | 19 [10–36] | 16 [4.5–28] | 0.137* | 18.1 [4.5–36] | 16.2 [6–28] | 0.303* | |
| Histology type, n (%) | |||||||
| Expansile | 22 (75.9) | 1 (25.0) | |||||
| Infiltrative | 7 (24.1) | 3 (75.0) | 0.073*** | ||||
*, independent t-test; **, Kruskal-Wallis test; ***, Fisher exact test. FIGO, International Federation of Gynaecology and Obstetrics.
We found that patients with infiltrative tumours were older than those with expansile tumours, with a median age of 62 vs. 55 years (P=0.049). Infiltrative tumours were diagnosed at a more advanced FIGO stage compared to expansile tumours: 4.3% were FIGO stage II and III in the expansile group compared to 50% in the infiltrative group (P=0.002).
Patients who relapsed had a higher FIGO stage at diagnosis (P<0.001). Relapse was more likely to occur when tumours were infiltrative (75.0% in the relapse vs. 24.1% in the no relapse group, P=0.073) or bilateral ( 50% in the relapse vs. 3.4% in the no relapse group, P=0.033).
IHC
We found PAX8 more frequently expressed in tumours with expansile pattern of invasion, although this association was not statistically-significant (75% vs. 37.5%, P=0.099).
We did not identify any statistically significant difference between IHC results of patients with expansile vs. infiltrative disease and those with vs. without relapse and without relapse (Table 2).
Table 2
| IHC markers | Expansile vs. infiltrative groups | No relapse vs. relapse groups | |||||
|---|---|---|---|---|---|---|---|
| Expansile | Infiltrative | P* | No relapse | Relapse | P* | ||
| CK20 | 17/21 (81%) | 9/9 (100%) | 0.287 | 22/26 (84.6%) | 4/4 (100%) | 1.0 | |
| CK7 | 22/22 (100%) | 9/9 (100%) | NA | 27/27 (100%) | 4/4 (100%) | NA | |
| CK8/18 | 7/7 (100%) | 4/4 (100%) | NA | 9/9 (100%) | 2/2 (100%) | NA | |
| CEA | 15/15 (100%) | 6/7 (85.7%) | 0.318 | 18/19 (94.7%) | 3/3 (100%) | 1.0 | |
| CA125 | 5/13 (38.5%) | 4/7 (57.1%) | 0.642 | 7/17 (41.2%) | 2/3 (66.7%) | 0.566 | |
| CA19.9 | 8/10 (80%) | 5/5 (100%) | 0.524 | 10/12 (83.3%) | 3/3 (100%) | 1.0 | |
| PAX8 | 12/16 (75%) | 3/8 (37.5%) | 0.099 | 14/21 (66.7%) | 1/3 (33.3%) | 0.533 | |
| P16 | 3/8 (37.5%) | 2/5 (40%) | 1.0 | 4/11 (36.4%) | 1/2 (50%) | 1.0 | |
| CD-X2 | 16/20 (80%) | 7/9 (77.8%) | 1.0 | 19/25 (76%) | 4/4 (100%) | 0.553 | |
*, Fisher exact test. IHC, immunohistochemistry; CK, cytokeratin; CEA, carcinoembryonic antigen; CA, cancer antigen; PAX8, paired-box gene 8.
We had some incomplete IHC data as not all IHC markers were employed for each patient. The total numbers of patients in which each IHC marker was tested are highlighted in Table 2.
Treatment
None of our patients had NACT. All 33 patients had UDS and R0 was achieved in all cases. Seven (21%) patients had fertility-sparing surgery (FSS), consisting of unilateral salpingo-oophorectomy and infracolic omentectomy. Omentectomy was not performed in 1/7 FSS patients who presented with a ruptured cyst and underwent unilateral salpingo-oophorectomy in an emergency setting. This was a FIGO IC expansile tumour and the MDT supported the patient’s wish to not undergo further surgery prior to fertility treatment. All FSS cases were expansile tumours. Out of these seven patients, one was FIGO stage IA, six were FIGO stage IC. Two of seven patients had adjuvant chemotherapy. None of the patients who had FSS experienced relapse. In keeping with the BGCS recommendations, pelvic and para-aortic lymphadenectomy was not routinely performed. One of our patients had pelvic and para-aortic lymph node dissection, while three other patients had removal of enlarged lymph nodes. All the lymph node samples were negative.
Adjuvant treatment (carboplatin/paclitaxel regime) was administered to 50% of patients with infiltrative disease, compared to only 13% of those with expansile disease (P=0.036). A proportion of 75% of patients who have relapsed had received adjuvant chemotherapy, compared to 17.2% of patients without relapse (P=0.036). This data is summarised in Table 3.
Table 3
| Treatment | Expansile vs. infiltrative groups | No relapse vs. relapse groups | |||||
|---|---|---|---|---|---|---|---|
| Expansile (n=23) | Infiltrative (n=10) | P | No relapse (n=29) | Relapse (n=4) | P | ||
| NACT | 0 | 0 | 0 | 0 | |||
| Surgery, n (%) | |||||||
| Hysterectomy | 0.143* | >0.99* | |||||
| Yes | 15 (65.2) | 8 (80.0) | 20 (69.0) | 3 (75.0) | |||
| No | 7 (30.4) | 0 | 7 (24.1) | 0 | |||
| Prev. hysterectomy | 1 (4.3) | 2 (20.0) | 2 (6.9) | 1 (25.0) | |||
| BSO/USO | 0.073* | 0.555* | |||||
| BSO | 16 (69.6) | 10 (100.0) | 22 (75.9) | 4 (100.0) | |||
| USO | 7 (30.4) | 0 | 7 (24.1) | 0 | |||
| Appendicectomy | 0.245* | >0.99* | |||||
| Yes | 11 (47.8) | 2 (20.0) | 12 (41.4) | 1 (25.0) | |||
| No | 12 (52.2) | 8 (80.0) | 17 (58.6) | 3 (75.0) | |||
| Omentectomy | 0.675** | 0.717** | |||||
| Yes | 20 (87.0) | 9 (90.0) | 25 (86.2) | 4 (100.0) | |||
| No | 1 (4.3) | 0 | 1 (3.5) | 0 | |||
| Biopsy | 2 (8.7) | 1 (10.0) | 3 (10.3) | 0 | |||
| Visceral/parietal peritonectomy | 0.085* | 0.231* | |||||
| Yes | 0 | 2 (20.0) | 1 (3.4) | 1 (25.0) | |||
| No | 23 (100.0) | 8 (80.0) | 28 (96.6) | 3 (75.0) | |||
| FSS | 0.073* | 0.555* | |||||
| Yes | 7 (30.4) | 0 | 7 (24.1) | 0 | |||
| No | 16 (69.6) | 10 (100.0) | 22 (75.9) | 4 (100.0) | |||
| LN dissection | 0.121* | ||||||
| Yes | 0 | 1 (10.0) | 0.303* | 0 | 1 (25.0) | ||
| No | 23 (100.0) | 9 (90.0) | 29 (100.0) | 3 (75.0) | |||
| Removal of enlarged LN | >0.99* | >0.99* | |||||
| Yes | 2 (8.7) | 1 (10.0) | 3 (10.3) | 0 | |||
| No | 21 (91.3) | 9 (90.0) | 26 (89.7) | 4 (100.0) | |||
| Adjuvant treatment | 0.036* | 0.036* | |||||
| Yes | 3 (13.0) | 5 (50.0) | 5 (17.2) | 3 (75.0) | |||
| No | 20 (87.0) | 5 (50.0) | 24 (82.8) | 1 (25.0) | |||
*, Fisher exact test; **, ANOVA test. NACT, neoadjuvant chemotherapy; BSO, bilateral salpingo-oophorectomy; USO, unilateral salpingo-oophorectomy; FSS, fertility-sparing surgery; LN, pelvic/para-aortic lymph nodes.
Survival
The median follow-up was 37 months (95% CI: 14.1–69.8), calculated using the reversed Kaplan-Meier method.
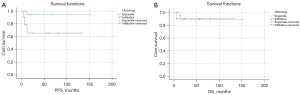
Survival outcomes are reported through Kaplan-Meier curves. At 3 years, there was a statistically significant difference in PFS (94.7% vs. 65.6%, P=0.02 log-rank) between the expansile and infiltrative groups (Figure 2A), but no difference in any-cause OS (88.8% vs. 90%, P=0.875 log-rank) (Figure 2B). The OS results cannot be interpreted due to the very small number of patients. In our retrospective cohort of 33 patients, three patients died (9%). Two deaths were a result of relapse: one patient had expansile MOC, FIGO stage IIA, the other one had infiltrative MOC, FIGO stage IIIA2. A third patient, with an expansile tumour FIGO stage IC, died of an unrelated cause, having had a CT chest, abdomen pelvis performed before death which excluded relapse.
Univariable Cox proportional hazards analysis of PFS and OS showed that FIGO stage and recurrence were prognostic factors for OS, while laterality was prognostic factor for PFS. These results are summarised in Table 4. Some of the HRs cannot be interpreted given the small sample size. Multivariable analysis did not identify any statistically significant association.
Table 4
| Variables | OS | PFS | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| Histology | 1.21 (0.11–13.38) | 0.87 | 8.38 (0.86–80.83) | 0.06 | |
| Age | 1.03 (0.95–1.26) | 0.39 | 1.009 (0.95–1.07) | 0.76 | |
| Size | 1.09 (0.95–1.26) | 0.19 | 0.96 (0.82–1.13) | 0.67 | |
| Laterality | 0.38 (0.11–1.29) | 0.12 | 0.26 (0.10–0.72) | 0.009 | |
| FIGO | 11.31 (1.31–97.45) | 0.02 | 11,442.5 (0.0–4.437E+21) | 0.65 | |
| Adjuvant treatment | 0.80 (0.24–2.66) | 0.71 | 0.31 (0.10–0.98) | 0.046 | |
| Recurrence | 16.78 (1.51–186.47) | 0.02 | – | – | |
OS, overall survival; PFS, progression-free survival; HR, hazards ratio; CI, confidence interval; FIGO, International Federation of Gynaecology and Obstetrics.
Discussion
We found that patients with infiltrative tumours were older, more likely to present with an advanced FIGO stage and more likely to have bilateral tumours. A possible association was identified between PAX8 IHC marker and expansile tumours, although this was not statistically significant. All our patients had primary surgery and R0 was achieved. Adjuvant treatment was more likely to be administered to patients who relapsed. Our study identified a statistically significant difference in PFS between the expansile and infiltrative groups.
Patient and tumour characteristics
Patients with infiltrative MOC were older than those with expansile MOC (mean age 62 vs. 55 years, P=0.047). Khunamornpong et al., in their retrospective analysis of 46 patients, reported similar findings, although their cohort of patients was younger overall: mean age of 53 years in the infiltrative group vs. 42 years in the expansile group (20).
Patients with infiltrative MOC were more likely to present with an advanced FIGO stage (FIGO II/III) at diagnosis (50% vs. 4.2%, P<0.001) and an advanced FIGO stage at diagnosis correlated with relapse (100% vs. 6.8%, P<0.001). This is in keeping with Muyldermans et al. (13).
Bilateral tumours were more likely to be infiltrative (20% vs. 4.3%, P=0.212) and more likely to relapse (50% vs. 3.4%, P=0.033). Huin et al. [2022] also reported a higher incidence of bilateral tumours in the infiltrative group (20% vs. 12%) (21).
We identified a possible association between the PAX8 IHC marker and the expansile pattern of invasion, although this was not statistically significant (P=0.099). This association has not been described before. We suggest two possible explanations. As PAX8 is typically used as a marker favouring a tumour origin in the genital tract, it may be that some of the PAX8 negative tumours in our study are metastases where the primary source could not be identified, rather than primary infiltrative MOCs. If these tumours are true primary MOCs, both the loss of PAX8 expression and the acquisition of an infiltrative pattern of invasion may be features of a tumour that is moving along the pathway from normal gene expression and behaviour to a more aggressive malignancy. Our numbers are too small to draw any conclusions, but this association warrants further investigation.
Treatment
All 33 patients had primary surgery and R0 was achieved in all cases. The standard surgical treatment of ovarian cancer FIGO stages I and II is total abdominal hysterectomy via a midline laparotomy, bilateral salpingo-oophorectomy, infracolic omentectomy, assessment of the appendix +/− appendicectomy, peritoneal cytology. In advanced EOC, UDS is offered when complete surgery with no macroscopic visible disease appears feasible, considering both the spread of disease and the general condition of the patient (22-29). Older age should not deter clinicians from offering radical surgery if pre-operative cardiopulmonary exercise testing (CPET) assessment is employed for patient selection (30).
Seven patients had FSS. This management is safe in patients with expansile tumours FIGO stage IA or IC, where fertility is a priority (23,25). None of the patients who underwent FSS experienced relapse or died.
Adjuvant treatment was more commonly administered to patients with infiltrative tumours (50% vs. 14%, P=0.036), reflecting the more advanced stage at diagnosis in the infiltrative group. 75% of patients who relapsed had received adjuvant treatment, compared to 17% of those who did not relapse (P=0.036). Similar findings were reported by Hada et al. (17). In their retrospective study of 49 patients with primary MOC, cases with infiltrative invasion were more frequently treated with adjuvant chemotherapy (P=0.02) more often recurred (P<0.01) than those with expansile invasion. Administration of adjuvant chemotherapy to patients with advanced MOC, therefore, does not seem to reduce their risk of relapse.
MOCs are known to be chemo-resistant to the Carboplatin-Paclitaxel regime. Alexandre et al. [2010] reviewed data from four randomized clinical trials (31), including a total of 786 patients with HGSC and 54 (5%) with primary MOC. His study found that, compared with HGSC, primary MOC was associated with lower response rate to Carboplatin-Paclitaxel based chemotherapy and shorter PFS and OS. For patients with FIGO stage IIB–IV, respective median PFS and OS were 11.4 months (95% CI: 8.3–14.5) and 21.6 months (95% CI: 11.7–31.6) for primary MOC patients versus 17.5 months (95% CI: 16.2–18.8, P=0.002) and 47.2 months (95% CI: 42.6–51.9, P<0.0001) for HGSC.
While there is an urgent need to develop new treatment options for this subtype of EOC, the rarity of this tumour has unfortunately been an obstacle in investigating alternative therapies. The mEOC/GOG 0241 randomised trial (32) set out to compare carboplatin/paclitaxel with oxaliplatin/capecitabine +/− bevacizumab for primary MOC FIGO stage II–IV, or recurrence after stage I disease. The trial stopped early due to slow accrual.
The Bouquet trial (NCT04931342, WO42178, GOG-3051, ENGOT-GYN2) is a phase II, multicentre study evaluating biomarker-driven therapies for patients with persistent or recurrent rare EOTs, including primary MOCs. This trial is currently running in 14 countries including the UK and is recruiting patients who are platinum-resistant and not amenable to curative surgery.
Two prospective randomised control trials (33,34) showed that, in selected patients with FIGO stage IIIC/IV ovarian cancer, NACT followed by interval debulking surgery is non-inferior to UDS. However, most patients enrolled in these two trials had HGSC. Less than 3% of patients had MOC in both the EORTC trial (19/670) and the CHORUS trial (6/474).
In the absence of an effective NACT or adjuvant chemotherapy option, maximal cytoreductive effort is of crucial importance in the management of primary MOCs.
Survival
At 3 years, PFS was 94.7% in the expansile group vs. 65.6% in the infiltrative group (P=0.02 log-rank). Huin et al. [2022] reported similar results in their study which included 35 expansile and 59 infiltrative primary MOCs (disease-free survival at 5 years was 90% for expansile tumours and 60% for infiltrative) (21).
Limitations
Main limitations of this study are the small number of patients in our cohort and the retrospective study design, with potential selection and information bias. Some of our IHC data was missing as not all 9 IHC markers in the panel were used for all patients. The HRs need to be interpreted with caution because of the wide confidence intervals secondary to the small sample size. OS data cannot be interpreted given there were only two disease-related deaths in our cohort, one in the expansile and one in the infiltrative group. The relatively short follow-up period (37 months median follow-up) limited our ability to evaluate long-term survival.
Conclusions
Our study adds to the limited existing evidence in the literature comparing characteristics and outcomes of expansile and infiltrative subtypes of primary MOC (17,20,21). Infiltrative tumours seem to present at a later age and are more likely to involve both ovaries. Patients with infiltrative tumours present with a more advanced FIGO stage and have a significantly worse PFS at 3 years, compared to those with expansile tumours (94.7% vs. 65.6%). In our study, patients who received adjuvant chemotherapy (carboplatin/paclitaxel) were more likely to relapse. Novel, biomarker-driven therapies are currently being investigated for rare ovarian tumours and may represent a better treatment option in the future. In the absence of a good NACT or adjuvant treatment option, surgery with maximal cytoreductive effort remains of critical importance in the management of primary MOCs. We found a possible association between PAX8 and the expansile MOC subtype which may warrant further investigation.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-863/rc
Data Sharing Statement: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-863/dss
Peer Review File: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-863/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-863/coif). AA is the founder, director and consultant of Singula Bio. SK is on the Advisory Board of Truscreen Ltd. and is Head of Medical Advisory Board and Trustee of OVACOME [Charity for ovarian cancer]. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Seidman JD, Kurman RJ, Ronnett BM. Primary and metastatic mucinous adenocarcinomas in the ovaries: incidence in routine practice with a new approach to improve intraoperative diagnosis. Am J Surg Pathol 2003;27:985-93. [Crossref] [PubMed]
- Babaier A, Ghatage P. Mucinous Cancer of the Ovary: Overview and Current Status. Diagnostics (Basel) 2020;10:52. [Crossref] [PubMed]
- Yoshikawa N, Kajiyama H, Mizuno M, et al. Clinicopathologic features of epithelial ovarian carcinoma in younger vs. older patients: analysis in Japanese women. J Gynecol Oncol 2014;25:118-23. [Crossref] [PubMed]
- Gates MA, Rosner BA, Hecht JL, et al. Risk factors for epithelial ovarian cancer by histologic subtype. Am J Epidemiol 2010;171:45-53. [Crossref] [PubMed]
- Morice P, Gouy S, Leary A. Mucinous Ovarian Carcinoma. N Engl J Med 2019;380:1256-66. [Crossref] [PubMed]
- Wu F, Zhao X, Mi B, et al. Clinical characteristics and prognostic analysis of Krukenberg tumor. Mol Clin Oncol 2015;3:1323-8. [Crossref] [PubMed]
- Cheasley D, Wakefield MJ, Ryland GL, et al. The molecular origin and taxonomy of mucinous ovarian carcinoma. Nat Commun 2019;10:3935. [Crossref] [PubMed]
- Mueller JJ, Schlappe BA, Kumar R, et al. Massively parallel sequencing analysis of mucinous ovarian carcinomas: genomic profiling and differential diagnoses. Gynecol Oncol 2018;150:127-35. [Crossref] [PubMed]
- Ahmed AA, Etemadmoghadam D, Temple J, et al. Driver mutations in TP53 are ubiquitous in high grade serous carcinoma of the ovary. J Pathol 2010;221:49-56. [Crossref] [PubMed]
- Filippini C, Smyth S, Soleymani Majd H, et al. Primary peritoneal mucinous cystadenocarcinoma mimicking possible recurrent ovarian mucinous cystadenoma: coincidental pathology or a spectrum of disease? BMJ Case Rep 2021;14:e242478. [Crossref] [PubMed]
- Lee KR, Scully RE. Mucinous tumors of the ovary: a clinicopathologic study of 196 borderline tumors (of intestinal type) and carcinomas, including an evaluation of 11 cases with 'pseudomyxoma peritonei'. Am J Surg Pathol 2000;24:1447-64. [Crossref] [PubMed]
- Kurman RJ, World Health Organization. WHO classification of tumours of female reproductive organs: [this book reflects the views of a working group that convened for a consensus and editorial meeting at the International Agency for Research on Cancer, Lyon, 13-15 June 2013]. Lyon: Internat. Agency For Re-search On Cancer; 2014.
- Muyldermans K, Moerman P, Amant F, et al. Primary invasive mucinous ovarian carcinoma of the intestinal type: importance of the expansile versus infiltrative type in predicting recurrence and lymph node metastases. Eur J Cancer 2013;49:1600-8. [Crossref] [PubMed]
- Talia KL, Parra-Herran C, McCluggage WG. Ovarian mucinous and seromucinous neoplasms: problematic aspects and modern diagnostic approach. Histopathology 2022;80:255-78. [Crossref] [PubMed]
- McCluggage WG, Wilkinson N. Metastatic neoplasms involving the ovary: a review with an emphasis on morphological and immunohistochemical features. Histopathology 2005;47:231-47. [Crossref] [PubMed]
- Dundr P, Singh N, Nožičková B, et al. Primary mucinous ovarian tumors vs. ovarian metastases from gastrointestinal tract, pancreas and biliary tree: a review of current problematics. Diagn Pathol 2021;16:20. [Crossref] [PubMed]
- Hada T, Miyamoto M, Ishibashi H, et al. Survival and biomarker analysis for ovarian mucinous carcinoma according to invasive patterns: retrospective analysis and review literature. J Ovarian Res 2021;14:33. [Crossref] [PubMed]
- Mutch DG, Prat J. 2014 FIGO staging for ovarian, fallopian tube and peritoneal cancer. Gynecol Oncol 2014;133:401-4. [Crossref] [PubMed]
- Hunter A, Addley S, Soleymani Majd H. Aggressive anaplastic ovarian carcinoma in a young nulliparous patient. BMJ Case Rep 2021;14:e241461. [Crossref] [PubMed]
- Khunamornpong S, Settakorn J, Sukpan K, et al. Primary ovarian mucinous adenocarcinoma of intestinal type: a clinicopathologic study of 46 cases. Int J Gynecol Pathol 2014;33:176-85. [Crossref] [PubMed]
- Huin M, Lorenzini J, Arbion F, et al. Presentation and Prognosis of Primary Expansile and Infiltrative Mucinous Carcinomas of the Ovary. J Clin Med 2022;11:6120. [Crossref] [PubMed]
- Berek JS, Renz M, Kehoe S, et al. Cancer of the ovary, fallopian tube, and peritoneum: 2021 update. Int J Gynaecol Obstet 2021;155:61-85. [Crossref] [PubMed]
- Fotopoulou C, Hall M, Cruickshank D, et al. British Gynaecological Cancer Society (BGCS) epithelial ovarian/fallopian tube/primary peritoneal cancer guidelines: recommendations for practice. Eur J Obstet Gynecol Reprod Biol 2017;213:123-39. [Crossref] [PubMed]
- Armstrong DK, Alvarez RD, Backes FJ, et al. NCCN Guidelines® Insights: Ovarian Cancer, Version 3.2022. J Natl Compr Canc Netw 2022;20:972-80. [Crossref] [PubMed]
- Colombo N, Sessa C, du Bois A, et al. ESMO-ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Int J Gynecol Cancer 2019;29:728-60. [Crossref] [PubMed]
- Querleu D, Planchamp F, Chiva L, et al. European Society of Gynaecological Oncology (ESGO) Guidelines for Ovarian Cancer Surgery. Int J Gynecol Cancer 2017;27:1534-42. [Crossref] [PubMed]
- Soleymani Majd H, Ferrari F, Manek S, et al. Diaphragmatic peritonectomy vs. full thickness resection with pleurectomy during Visceral-Peritoneal Debulking (VPD) in 100 consecutive patients with stage IIIC-IV ovarian cancer: A surgical-histological analysis. Gynecol Oncol 2016;140:430-5. [Crossref] [PubMed]
- Tozzi R, Giannice R, Cianci S, et al. Neo-adjuvant chemotherapy does not increase the rate of complete resection and does not significantly reduce the morbidity of Visceral-Peritoneal Debulking (VPD) in patients with stage IIIC-IV ovarian cancer. Gynecol Oncol 2015;138:252-8. [Crossref] [PubMed]
- Tozzi R, Hardern K, Gubbala K, et al. En-bloc resection of the pelvis (EnBRP) in patients with stage IIIC-IV ovarian cancer: A 10 steps standardised technique. Surgical and survival outcomes of primary vs. interval surgery. Gynecol Oncol 2017;144:564-70. [Crossref] [PubMed]
- Pinelli C, Morotti M, Casarin J, et al. Interval Debulking Surgery for Advanced Ovarian Cancer in Elderly Patients (≥70 y): Does the Age Matter? J Invest Surg 2021;34:1023-30. [Crossref] [PubMed]
- Alexandre J, Ray-Coquard I, Selle F, et al. Mucinous advanced epithelial ovarian carcinoma: clinical presentation and sensitivity to platinum-paclitaxel-based chemotherapy, the GINECO experience. Ann Oncol 2010;21:2377-81. [Crossref] [PubMed]
- Gore M, Hackshaw A, Brady WE, et al. An international, phase III randomized trial in patients with mucinous epithelial ovarian cancer (mEOC/GOG 0241) with long-term follow-up: and experience of conducting a clinical trial in a rare gynecological tumor. Gynecol Oncol 2019;153:541-8. [Crossref] [PubMed]
- Vergote I, Tropé CG, Amant F, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med 2010;363:943-53. [Crossref] [PubMed]
- Kehoe S, Hook J, Nankivell M, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet 2015;386:249-57. [Crossref] [PubMed]


