Development and validation of nomogram-based models for personalized survival assessment in pediatric hepatoblastoma patients
Highlight box
Key findings
• The first nomogram for cancer-specific survival of hepatoblastoma was derived using commonly available clinicopathological factors.
What is known and what is new?
• Hepatoblastoma (HB) is the predominant hepatic cancer observed in pediatric patients. Previous studies have identified various factors associated with HB prognosis, including age, α-fetoprotein levels at diagnosis, pathological subtype, and the presence of distant metastases.
• We combined the specific clinicopathologic factors to create the first prediction model to evaluate the cancer-specific survival of HB patients.
What is the implication, and what should change now?
• The nomogram-based models exhibited innovation and have undergone rigorous validation, showcasing remarkable prediction accuracy. These models evaluate personalized cancer-specific survival and overall survival in individuals diagnosed with HB. The aforementioned technologies exhibit a high degree of user-friendly interface and provide considerable promise in computing individualized survival probability, facilitating risk classification, and enhancing the clinical decision-making process.
Introduction
Hepatoblastoma (HB) is the predominant hepatic cancer observed in pediatric patients, accounting for around 1% of all malignancies in those below 15 years. It represents a substantial 80% of primary liver malignancies, with a notable predisposition for children aged under 3 years (1,2). The annual incidence rate of HB is around 1.5 cases per one million individuals and has exhibited a consistent annual increase of 4.3% (3,4). Recent advancements in therapy have resulted in notable enhancements in the prognosis of pediatric patients diagnosed with HB. Integrating surgical and chemotherapeutic interventions has yielded noteworthy 5-year overall survival (OS) and disease-free survival rates, attaining 88.9% and 80.8%, respectively (5,6). The achievement of total elimination of liver tumors is of utmost importance in ensuring the efficacy of the treatment (7). To enhance the potential of attaining this significant goal, medical practitioners commonly employ preoperative or postoperative chemotherapy, diminishing the probability of tumor reoccurrence (8,9).
The prognosis of HB is connected with several parameters, including age, levels of α-fetoprotein (AFP) upon diagnosis, clinical subtype, and the occurrence of distant metastases (10-13). Nevertheless, despite the acknowledgment of these characteristics, a widely acknowledged risk categorization method for HB is yet to be established. The Children’s Oncology Group (COG) in North America introduced the postoperative COG Evans staging system. This staging approach emphasizes the prognostic importance of postoperative tumor residue and histopathological type. The pretreatment extent of disease (PRETEXT) staging method, created by the International Childhood Liver Tumor Strategy Group, evaluates the extent of pediatric liver tumors before initiating therapy. This takes into account the presence of tumors and examines the influence of distant metastasis on the overall prognosis. The establishment of the Children’s Hepatic Tumors International Collaboration-Hepatoblastoma Stratification (CHIC-HS) occurred in 2016 through a collaborative effort, including many research institutions operating under the auspices of CHIC (14). The current state of knowledge on the predictive efficacy of this risk stratification method for children with HB is still uncertain. A study by Huang et al. showed a comparative analysis of the COG and CHIC-HS risk stratification methods, and their findings led them to conclude that the CHIC-HS method has more accuracy in predicting survival outcomes (15). In contrast, Hsu et al. observed no statistically significant variation in survival rates between children classified as intermediate-risk and high-risk when using the CHIC-HS risk stratification method (16). Despite the endeavors mentioned above, the established prognostic variables and the generally recognized staging methods need to offer an ideal framework for accurately evaluating individual patient survival probability.
To address this gap, the utilization of nomograms emerges as a potentially beneficial strategy. Nomograms, regarded as robust statistical tools, effectively incorporate all independent prognostic variables into a graphical representation for predicting event rates. Nomograms have demonstrated clinical utility in several cancer types, including neuroblastoma, pancreatic cancer, and lung cancer, has been shown in earlier research (17-19). Nomograms are renowned for their capacity to offer precise, personalized prognostic estimates, exceeding conventional tumor staging standards. Nevertheless, previous studies have only conducted limited investigations to explore the potential of developing a nomogram-based prediction model for precise forecasts of the OS of patients with HB (20,21). In addition, previous studies have not shown specially tailored nomograms to forecast cancer-specific survival (CSS) within patients with HB.
As HB is relatively uncommon, there is a lack of availability of prospective data and large-scale clinical trials. Given the current situation, the Surveillance, Epidemiology, and End Results (SEER) program was employed, offering an extensive dataset encompassing various cancer types within the American population to address this limitation. Employing this useful source, the treatment outcomes, clinical characteristics, and prognostic factors of HB in the pediatric population were investigated. The present investigation accurately identified independent prognostic parameters for CSS and OS in HB patients. Furthermore, a nomogram was developed while incorporating these characteristics to facilitate the prognostication of CSS and OS. The prediction accuracy of this nomogram was systematically and thoroughly assessed. We present this article in accordance with the TRIPOD reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-1786/rc).
Methods
Selection of patients and study design
The research employed the SEER database from the National Cancer Institute (NCI). The data collected encompassed the baseline characteristics and clinicopathologic parameters, including gender (male or female), age, race (White or others), the North American Association of Central Cancer Registries Hispanic Identification Algorithm (NHIA) (Non-Spanish-Hispanic-Latino or Spanish-Hispanic-Latino), summary stage (localized, regional or distant), tumor size, surgery of the tumor (yes or no surgery), chemotherapy of the tumor (yes or no radiotherapy), systemic therapy of tumor (yes or no systemic therapy), lung metastasis (yes or no), OS, and CSS. In this study, systemic therapy is defined as the administration of chemotherapy combined with surgical treatment, irrespective of the order in which they were given. The SEER* Stat 8.4.1 program was utilized for data analysis. The individuals who satisfied the predetermined criteria for eligibility were clinically diagnosed with HB via a thorough examination of histological samples. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As per the ethics guidelines, since public and anonymous data were utilized, neither informed consent nor approval of an ethics committee was necessary.
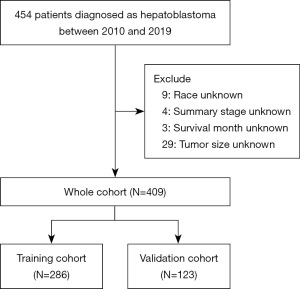
This led to the inclusion of a total of 409 individuals who had complete data and follow-up information between 2004 and 2019. A random partitioning approach was employed to achieve dataset balance, with a 7:3 ratio. This approach resulted in forming two distinct cohorts: a training cohort comprising 286 patients and a separate validation cohort comprising 123 patients. The development of nomograms for predicting CSS and OS was undertaken using training data. These nomograms were subsequently subjected to a rigorous validation process using an independent validation cohort. To stratify patients based on age and tumor size, we relied on the X-tile program, a tool from Yale University. The program accurately determined the precise cutoff points, leading to the classification of age into two distinct groups: those under 2 years old and those aged 2 years or older. Similarly, tumor size was categorized into two groups: tumors measuring less than 123 mm and those measuring 123 mm or larger (Figure 1). This systematic approach improved our analysis, ultimately increasing the precision of our results.

Study outcomes and nomogram construction
The investigation was primarily focused on CSS and OS. The CSS was defined as the duration between the initial diagnosis of HB and HB-specific mortality. In contrast, OS was described as the duration between the initial diagnosis of HB to the mortality from any reason or the date of the patient’s last follow-up.
In order to validate and assess the precision of the nomogram, we initially identified predictors associated with both OS and CSS by the implementation of multivariate and univariate Cox proportional hazard regression models. Subsequently, a thorough and detailed construction of a survival outcomes nomogram was conducted, utilizing the insights from the multivariate Cox regression models. The validity of the nomogram was confirmed by employing a bootstrap resampling technique, and its prediction accuracy was assessed using the concordance index (C-index). Calibration plots were employed to contrast predicted survival estimates with actual probabilities. In addition, the model’s effectiveness was determined by computing the area under the receiver operating characteristic curve (AUC-ROC). Moreover, decision curve analysis (DCA) was utilized to evaluate the prediction model’s clinical usefulness by quantifying the benefits of including the nomogram in the decision-making process.
Statistical analysis
Statistical methods such as Fisher exact tests or Chi-square tests were utilized to compare the training and validation cohorts in relation to categorical clinicopathologic variables. The evaluation of continuous variables was conducted by the utilization of t-tests or Mann-Whitney U-tests. The examination of survival disparities between subgroups was performed using Kaplan-Meier analysis and log-rank testing. The statistical analyses were executed using IBM SPSS version 26.0 and R software version 4.2.0 (www.r-project.org). A P<0.05 was considered as statistical significance.
Results
Baseline characteristics of HB patients
The present retrospective analysis examined the clinicopathological and demographic characteristics of 409 patients with HB according to the predefined inclusion criteria (Figure 2). The patients were randomly distributed into two groups: a training group comprising 286 patients and a validation group comprising 123 patients. The random allocation was done at a ratio of 7:3 between the years 2010 and 2019. Table 1 provides an overview of the baseline patient characteristics for both cohorts. Notably, the clinical characteristics had a consistent uniform distribution and were comparable across both groups. In the total cohort, a significant proportion of patients were under the age of 2 (61.6%), identified as male (60.6%), belonged to the White ethnic group (73.6%), and were classified as Non-Spanish-Hispanic-Latino (66.7%). The study yielded promising results, indicating that a significant proportion of patients, around 89.5%, had surgical intervention. Additionally, it was observed that a substantial majority, around 92.9%, of individuals diagnosed with HB received adjuvant chemotherapy. The investigation included a cohort of pediatric patients with HB, having a median duration of follow-up of 54 months. The OS rates at 1, 3, and 5 years were 92.1%, 88.0%, and 85.8%, respectively. Similarly, the corresponding CSS rates were 94.3%, 90.4%, and 88.8%, respectively. Among the pediatric cohort, a notable proportion of individuals, around 15.6%, presented with distant metastases, with the lungs being the primary site of metastasis. In this subset, the one-year OS and CSS rates were 75.8% and 77.2%, respectively. Figure 3 presents a graphical representation of the survival curves, which explored the impact of variables such as age, summary stage, surgery, chemotherapy, systemic therapy, tumor size, and lung metastasis on the prognosis of HB. This study was conducted via the Kaplan-Meier method and the P<0.05 was considered statistically significant.
Table 1
| Characteristics | Whole cohort (N=409) | Training cohort (N=286) | Validation cohort (N=123) | P |
|---|---|---|---|---|
| Age (years) | >0.99 | |||
| <2 | 252 (61.6) | 176 (61.5) | 76 (61.8) | |
| ≥2 | 157 (38.4) | 110 (38.5) | 47 (38.2) | |
| Gender | >0.99 | |||
| Male | 248 (60.6) | 173 (60.5) | 75 (61.0) | |
| Female | 161 (39.4) | 113 (39.5) | 48 (39.0) | |
| Race | 0.903 | |||
| White | 301 (73.6) | 211 (73.8) | 90 (73.2) | |
| Others | 108 (26.4) | 75 (26.2) | 33 (26.8) | |
| NHIA | >0.99 | |||
| Non-Spanish-Hispanic-Latino | 273 (66.7) | 191 (66.8) | 82 (66.7) | |
| Spanish-Hispanic-Latino | 136 (33.3) | 95 (33.2) | 41 (33.3) | |
| Summary stage | 0.204 | |||
| Localized | 224 (54.8) | 163 (57.0) | 61 (49.6) | |
| Regional | 121 (29.6) | 77 (26.9) | 44 (35.8) | |
| Distant | 64 (15.6) | 46 (16.1) | 18 (14.6) | |
| Surgery | 0.727 | |||
| No | 43 (10.5) | 29 (10.1) | 14 (11.4) | |
| Yes | 366 (89.5) | 257 (89.9) | 109 (88.6) | |
| Chemotherapy | >0.99 | |||
| No/unknown | 29 (7.1) | 20 (7.0) | 9 (7.3) | |
| Yes | 380 (92.9) | 266 (93.0) | 114 (92.7) | |
| Systemic therapy | 0.766 | |||
| No | 63 (15.4) | 43 (15.0) | 20 (16.3) | |
| Yes | 346 (84.6) | 243 (85.0) | 103 (83.7) | |
| Tumor size (mm) | 0.307 | |||
| <123 | 315 (77.0) | 216 (75.5) | 99 (80.5) | |
| ≥123 | 94 (23.0) | 70 (24.5) | 24 (19.5) | |
| Lung metastasis | >0.99 | |||
| No | 352 (86.1) | 246 (86.0) | 106 (86.2) | |
| Yes | 57 (13.9) | 40 (14.0) | 17 (13.8) |
Data are presented as n (%). NHIA, North American Association of Central Cancer Registries Hispanic Identification Algorithm.

Predictor selection
Multivariate and univariate Cox regression analyses were performed to ascertain independent prognostic markers for CSS and OS. The entire findings from these studies are presented in Tables 2,3. The final multivariate analysis solely included the prognostic variables deemed relevant based on the prior univariate study. A multivariate study demonstrated that patient age, surgery, chemotherapy, and tumor size (Table 2) significantly influenced OS in individuals diagnosed with HB. Furthermore, the research revealed that age, surgery, and chemotherapy were significant predictors of CSS, as indicated in Table 3.
Table 2
| Characteristics | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | ||
| Age (years) | |||||||
| <2 | Reference | Reference | |||||
| ≥2 | 3.237 | 1.505–6.962 | 0.003 | 2.973 | 1.215–7.273 | 0.017 | |
| Gender | |||||||
| Male | Reference | ||||||
| Female | 1.470 | 0.710–3.046 | 0.300 | ||||
| Race | |||||||
| White | Reference | ||||||
| Others | 1.819 | 0.859–3.851 | 0.118 | ||||
| NHIA | |||||||
| Non-Spanish-Hispanic-Latino | Reference | ||||||
| Spanish-Hispanic-Latino | 0.769 | 0.341–1.736 | 0.527 | ||||
| Summary Stage | |||||||
| Localized | Reference | Reference | |||||
| Regional | 3.103 | 1.203–8.005 | 0.019 | 1.260 | 0.430–3.691 | 0.674 | |
| Distant | 6.172 | 2.392–15.926 | <0.001 | 1.133 | 0.132–9.726 | 0.909 | |
| Surgery | |||||||
| No | Reference | Reference | |||||
| Yes | 0.070 | 0.034–0.146 | <0.001 | 0.025 | 0.004–0.165 | <0.001 | |
| Chemotherapy | |||||||
| No/unknown | Reference | Reference | |||||
| Yes | 0.265 | 0.101–0.695 | <0.001 | 0.052 | 0.011–0.255 | <0.001 | |
| Systemic therapy | |||||||
| No | Reference | Reference | |||||
| Yes | 0.108 | 0.052–0.224 | <0.001 | 4.702 | 0.679–32.566 | 0.117 | |
| Tumor size (mm) | |||||||
| <123 | Reference | Reference | |||||
| ≥123 | 5.550 | 2.643–11.650 | <0.001 | 4.649 | 1.677–12.891 | 0.003 | |
| Lung metastasis | |||||||
| No | Reference | Reference | |||||
| Yes | 3.909 | 1.815–8.416 | <0.001 | 1.226 | 0.139–10.800 | 0.854 | |
HR, hazard ratio; CI, confidence interval; NHIA, North American Association of Central Cancer Registries Hispanic Identification Algorithm.
Table 3
| Characteristics | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | ||
| Age (years) | |||||||
| <2 | Reference | Reference | |||||
| ≥2 | 4.145 | 1.718–9.998 | 0.002 | 3.995 | 2.418–7.768 | 0.011 | |
| Gender | |||||||
| Male | Reference | ||||||
| Female | 1.127 | 0.501–2.537 | 0.773 | ||||
| Race | |||||||
| White | Reference | Reference | |||||
| Others | 2.524 | 1.130–5.635 | 0.024 | 2.210 | 0.708–1.971 | 0.080 | |
| NHIA | |||||||
| Non-Spanish-Hispanic-Latino | Reference | ||||||
| Spanish-Hispanic-Latino | 0.675 | 0.268–1.701 | 0.850 | ||||
| Summary stage | |||||||
| Localized | Reference | Reference | |||||
| Regional | 3.147 | 1.029–9.622 | 0.044 | 1.453 | 0.420–2.482 | 0.567 | |
| Distant | 8.627 | 2.996–24.837 | <0.001 | 1.867 | 1.572–8.126 | 0.590 | |
| Surgery | |||||||
| No | Reference | Reference | |||||
| Yes | 0.064 | 0.028–0.143 | <0.001 | 0.056 | 1.061–2.404 | 0.017 | |
| Chemotherapy | |||||||
| No/unknown | Reference | Reference | |||||
| Yes | 0.278 | 0.095–0.814 | 0.020 | 0.123 | 0.138–0.772 | 0.027 | |
| Systemic therapy | |||||||
| No | Reference | Reference | |||||
| Yes | 0.095 | 0.042–0.213 | <0.001 | 1.959 | 0.835–1.577 | 0.596 | |
| Tumor size (mm) | |||||||
| <123 | Reference | Reference | |||||
| ≥123 | 5.539 | 2.453–12.510 | <0.001 | 3.004 | 1.035–1.961 | 0.068 | |
| Lung metastasis | |||||||
| No | Reference | Reference | |||||
| Yes | 5.308 | 2.354–11.970 | <0.001 | 1.539 | 1.035–1.961 | 0.707 | |
HR, hazard ratio; CI, confidence interval; NHIA, North American Association of Central Cancer Registries Hispanic Identification Algorithm.
Construction of nomograms
The nomograms were developed for CSS and OS based on multivariate Cox analysis by incorporating the independent prognostic variables into the assessment. Nomograms are presented in Figure 4, where they provided predictions for 1-, 3-, and 5-year intervals. Combining the scores associated with each selected variable was necessary to determine the likelihood of an HB patient’s survival. As an example, a patient of age three, diagnosed with a tumor measuring 15 cm and possessing a medical background involving chemotherapy and surgical procedures, would obtain a cumulative score of 102 and 52 in the OS and CSS nomograms, respectively. These findings provided projected 1-, 3-, and 5-year OS rates of 90%, 81%, and 77%, respectively; in addition to this, the corresponding CSS rates of 1-, 3-, and 5-year were about 96%, 93%, and 91%, respectively.

Validation of nomograms
The training set yielded C-index values of 0.864 for OS and 0.836 for CSS, indicating a strong discriminative capacity. The results obtained in the validation set were also strong, as evidenced by the C-index values of 0.762 for OS and 0.791 for CSS. The predictive ability of the nomograms was further validated using the ROC curves. The training set exhibited exceptional performance regarding 1-, 3-, and 5-year OS, as evidenced by the area AUC values of 0.915, 0.846, and 0.847, respectively (Figure 5A). The AUC of the validation set were 0.795, 0.713, and 0.666 (Figure 5B). Figure 5C-5H for OS provided additional evidence between the predicted and observed survival probabilities in the training and validation datasets. Similarly, the AUC for 1-, 3-, and 5-year CSS were found to be 0.871, 0.814, and 0.825 in the training set, as depicted in Figure 6A. In the validation set, the corresponding AUCs were 0.914, 0.734, and 0.710, as illustrated in Figure 6B. Figure 6C-6H for CSS provided additional evidence between the predicted and observed survival probabilities in the training and validation datasets. The clinical utility of the nomogram-based models for predicting survival at different time intervals (1 year, 3 years, and 5 years) was proven by the DCA presented in Figure 7.



Web-based survival rate calculator
To enhance accessibility, a web-based survival rate calculator (https://nbnomogram.shinyapps.io/NBnomo/) incorporating the nomogram was constructed. This tool enables healthcare professionals and individuals receiving medical care to estimate long-term OS. For example, a scenario involving a 6-month-old boy with HB and a tumor size of less than 123 mm is illustrated. The 3-year OS rate is approximately 26.6% without chemotherapy and surgical resection. However, with chemotherapy and surgical resection, the 3-year OS rate significantly improves to approximately 99.0% (Figure 8).

Discussion
In this extensive retrospective investigation, novel nomograms were designed and validated for the prediction of the CSS and OS in a larger group of pediatric patients with HB. Nomograms can provide individualized long-term prognosis prediction, hence offering improved decision-making for clinical decisions. The construction of the nomogram was done by the utilization of multivariate Cox regression to identify prognostic markers. Moreover, the differentiation, calibration, and utility assessments conducted in our work have revealed the robust prediction capabilities of the nomograms.
Primary liver tumors in pediatric patients account for around 1% of all tumors in children and 5–6% in the abdominal region. Among these tumors, HB is the most frequently occurring tumor (22,23). HB includes various tumors arising from various hepatic precursor cells, exhibiting marked heterogeneity and varying clinical outcomes (5,24). Accurate risk stratification is essential for treatment planning, requiring the identification of prognostic risk factors. Multiple investigations have found many indicators associated with an unfavorable prognosis, including PRETEXT stages, metastasis, AFP levels ranging from 100–999 ng/L, tumor multifocality, vascular invasion, extrahepatic invasion, and older age of disease onset (25-28). The study determined that the independent predictive variables were age, chemotherapy, and surgery.
According to the nomograms, chemotherapeutic treatments are the most significant prognostic indicators for both OS and CSS after surgical procedures in both point axes. Combining radical surgery and chemotherapy significantly enhances the survival rates of children diagnosed with HB. Despite the need for chemotherapy due to insufficient resection after diagnosis, surgery continues to be the primary treatment for HB (29,30). Surgery timing is still debatable, as COG recommends surgery for very-low-risk and low-risk groups (PRETEXT stages I and II) without major vessel invasion, while International Childhood Liver Tumors Strategy Group (SIOPEL) suggests chemotherapy for all patients. Therefore, timing remains a clinical concern, with some studies supporting direct surgery for very low-risk cases (31,32). For unresectable tumors at diagnosis, standard treatment involves preoperative chemotherapy, surgical resection, and postoperative chemotherapy (33). The efficacy of neoadjuvant chemotherapy in reducing tumor growth and preventing concealed metastases has been demonstrated. Furthermore, the integration of delayed surgery has notably augmented the survival percentage among pediatric patients diagnosed with HB (34).
The evaluation of chemotherapy effectiveness for solid tumors heavily relies on the measurement of tumor size, commonly represented by the maximum diameter. The assessment of therapy efficacy predominantly hinges upon alterations in tumor dimensions. The research conducted in our study revealed that around 23% of tumors had a maximum diameter ≥123 mm. The use of multifactorial Cox regression analysis revealed that children with tumors of bigger size (≥123 mm) had less favorable prognoses. Distant metastases occur in around 20% of cases of HB, with the lungs being the most commonly affected site. As a result, the OS rates for patients with HB ranged from 25% to 50% (35,36). In the current study, it was seen that a total of 64 individuals out of the 409 participants, accounting for 15.6% of the sample, experienced the development of distant metastases. These metastases were predominantly found in the lungs, and their presence had a notable and statistically significant influence on the long-term prognosis of the affected individuals. The customary approach for managing HB with lung metastasis normally entails the administration of chemotherapy as the first treatment, with subsequent resection if residual tumors persist (37). The age of the patient significantly influences the prognosis of HB. Young children under the age of 3 generally have more positive results. Comparatively, the 8 years old or older exhibit fewer favorable prognoses. The prognostic significance of parameters such as metastatic disease, AFP levels, and tumor rupture is also influenced by age, which in turn affects chemotherapy intensity recommendations (10,27). In this study, the age of the children was classified into two groups using the X-tile tool: under two years old and two years old or older. The study’s results indicated that infants under two years had more favorable survival rates.
The presence of HB poses a substantial risk to the well-being of pediatric patients, underscoring the critical need for accurate prognostic assessment of survival outcomes. Unfortunately, the existing models for this particular purpose are insufficient. The present study aims to address this knowledge deficit by proposing nomograms for OS and CSS that apply to all individuals diagnosed with HB. Their robust discriminatory and calibration capabilities evidence the efficacy of these nomograms. The research conducted in our study demonstrated a high level of reliability and dependability since it incorporated a significant sample size consisting of 409 patients. These nomograms utilized all available clinical datasets, enabling personalized survival predictions for survival outcomes of HB patients. However, the effective application of these nomograms in actual scenarios is impeded by the requirement of human computations. To tackle this matter, a user-friendly online application has been developed to forecast the survival probabilities of individuals diagnosed with HB at different points in time.
Nevertheless, it is crucial to acknowledge that this research possesses certain limitations. The retrospective analysis may be susceptible to bias. Furthermore, it should be noted that the SEER database exhibits several limitations in its inclusion of prognostic indicators. Notably, the database needs to incorporate significant variables such as tumor markers, treatment specifics, and the number of masses. The absence of these elements may hinder the precision of survival prognoses. Furthermore, it is essential to conduct a prospective validation of the process of developing and validating the nomogram in a separate dataset to establish its reliability. This is crucial since relying just on a single database has inherent limits. Notwithstanding these constraints, our research offers significant contributions and should be viewed with prudence.
Conclusions
To conclude, the nomogram-based models exhibit innovation and have undergone rigorous validation, showcasing remarkable prediction accuracy. These models evaluate personalized CSS and OS in individuals diagnosed with HB. The aforementioned technologies exhibit a high degree of user-friendly interface and provide considerable promise in computing individualized survival probability, facilitating risk classification, and enhancing the clinical decision-making process.
Acknowledgments
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the TRIPOD reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-1786/rc
Peer Review File: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-1786/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-1786/coif). All authors report that this work was supported by the Startup Fund for scientific research, Fujian Medical University (No. 2020QH1200). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As per the ethics guidelines, since public and anonymous data were utilized, neither informed consent nor approval of an ethics committee was necessary.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Czauderna P, Lopez-Terrada D, Hiyama E, et al. Hepatoblastoma state of the art: pathology, genetics, risk stratification, and chemotherapy. Curr Opin Pediatr 2014;26:19-28. [Crossref] [PubMed]
- Ranganathan S, Lopez-Terrada D, Alaggio R. Hepatoblastoma and Pediatric Hepatocellular Carcinoma: An Update. Pediatr Dev Pathol 2020;23:79-95. [Crossref] [PubMed]
- Li P, Kong Y, Guo J, et al. Incidence and trends of hepatic cancer among children and adolescents in the United States from 2000 to 2017: Evidence from the Surveillance, Epidemiology, and End Results registry data. Cancer Causes Control 2023;34:69-79. [Crossref] [PubMed]
- Spector LG, Birch J. The epidemiology of hepatoblastoma. Pediatr Blood Cancer 2012;59:776-9. [Crossref] [PubMed]
- Lim IIP, Bondoc AJ, Geller JI, et al. Hepatoblastoma-The Evolution of Biology, Surgery, and Transplantation. Children (Basel) 2018;6:1. [Crossref] [PubMed]
- Tayfun Küpesiz F, Akınel AN, Akbaş H, et al. Multidisciplinary Management of Pediatric Hepatoblastoma: A 20-Year Single-Center Experience. Turk J Gastroenterol 2022;33:1069-78. [Crossref] [PubMed]
- Malogolowkin MH, Katzenstein HM, Meyers RL, et al. Complete surgical resection is curative for children with hepatoblastoma with pure fetal histology: a report from the Children's Oncology Group. J Clin Oncol 2011;29:3301-6. [Crossref] [PubMed]
- Hirakawa M, Nishie A, Asayama Y, et al. Efficacy of preoperative transcatheter arterial chemoembolization combined with systemic chemotherapy for treatment of unresectable hepatoblastoma in children. Jpn J Radiol 2014;32:529-36. [Crossref] [PubMed]
- Tian Y, Chen X, Yu F, et al. Neoadjuvant chemotherapy or upfront surgery in hepatoblastoma: A multicenter retrospective study. Pediatr Blood Cancer 2023; Epub ahead of print. [Crossref]
- Haeberle B, Rangaswami A, Krailo M, et al. The importance of age as prognostic factor for the outcome of patients with hepatoblastoma: Analysis from the Children's Hepatic tumors International Collaboration (CHIC) database. Pediatr Blood Cancer 2020;67:e28350. [Crossref] [PubMed]
- Koh KN, Park M, Kim BE, et al. Prognostic implications of serum alpha-fetoprotein response during treatment of hepatoblastoma. Pediatr Blood Cancer 2011;57:554-60. [Crossref] [PubMed]
- Qiao GL, Chen Z, Wang C, et al. Pure fetal histology subtype was associated with better prognosis of children with hepatoblastoma: A Chinese population-based study. J Gastroenterol Hepatol 2016;31:621-7. [Crossref] [PubMed]
- Wanaguru D, Shun A, Price N, et al. Outcomes of pulmonary metastases in hepatoblastoma--is the prognosis always poor? J Pediatr Surg 2013;48:2474-8. [Crossref] [PubMed]
- Czauderna P, Haeberle B, Hiyama E, et al. The Children's Hepatic tumors International Collaboration (CHIC): Novel global rare tumor database yields new prognostic factors in hepatoblastoma and becomes a research model. Eur J Cancer 2016;52:92-101. [Crossref] [PubMed]
- Huang J, Hu Y, Jiang H, et al. CHIC Risk Stratification System for Predicting the Survival of Children With Hepatoblastoma: Data From Children With Hepatoblastoma in China. Front Oncol 2020;10:552079. [Crossref] [PubMed]
- Hsu WY, Chang HH, Lu MY, et al. Clinical risk stratification of children with SIOPEL high-risk hepatoblastoma in Taiwan. Pediatr Neonatol 2020;61:393-8. [Crossref] [PubMed]
- Chen W, Lin P, Bai J, et al. Establishment and validation of a nomogram to predict cancer-specific survival in pediatric neuroblastoma patients. Front Pediatr 2023;11:1105922. [Crossref] [PubMed]
- Yang Z, Shi G, Zhang P. Development and Validation of Nomograms to Predict Overall Survival and Cancer-Specific Survival in Patients With Pancreatic Adenosquamous Carcinoma. Front Oncol 2022;12:831649. [Crossref] [PubMed]
- Yu X, Wang F, Yang L, et al. Development and validation of web-based dynamic nomograms predictive of disease-free and overall survival in patients who underwent pneumonectomy for primary lung cancer. PeerJ 2023;11:e15938. [Crossref] [PubMed]
- Feng J, Polychronidis G, Heger U, et al. Incidence trends and survival prediction of hepatoblastoma in children: a population-based study. Cancer Commun (Lond) 2019;39:62. [Crossref] [PubMed]
- Ge B, Zhuo C, Tang Q, et al. Clinical features and a prognostic nomogram based on the SEER database for hepatoblastoma, hepatocellular carcinoma, and embryonal sarcoma among children and adolescents. Transl Pediatr 2023;12:172-84. [Crossref] [PubMed]
- Lucas B, Ravishankar S, Pateva I. Pediatric Primary Hepatic Tumors: Diagnostic Considerations. Diagnostics (Basel) 2021;11:333. [Crossref] [PubMed]
- Meyers R, Hiyama E, Czauderna P, et al. Liver Tumors in Pediatric Patients. Surg Oncol Clin N Am 2021;30:253-74. [Crossref] [PubMed]
- Zhou S, Malvar J, Chi YY, et al. Independent Assessment of the Children's Hepatic Tumors International Collaboration Risk Stratification for Hepatoblastoma and the Association of Tumor Histological Characteristics With Prognosis. JAMA Netw Open 2022;5:e2148013. [Crossref] [PubMed]
- Boster JM, Superina R, Mazariegos GV, et al. Predictors of survival following liver transplantation for pediatric hepatoblastoma and hepatocellular carcinoma: Experience from the Society of Pediatric Liver Transplantation (SPLIT). Am J Transplant 2022;22:1396-408. [Crossref] [PubMed]
- Hu H, Zhang W, Wang Y, et al. Prognostic analysis for children with hepatoblastoma with lung metastasis: A single-center analysis of 98 cases. Asia Pac J Clin Oncol 2021;17:e191-200. [Crossref] [PubMed]
- Meyers RL, Maibach R, Hiyama E, et al. Risk-stratified staging in paediatric hepatoblastoma: a unified analysis from the Children's Hepatic tumors International Collaboration. Lancet Oncol 2017;18:122-31. [Crossref] [PubMed]
- Trobaugh-Lotrario AD, Maibach R, Aronson DC, et al. Outcomes of Patients Treated for Hepatoblastoma with Low Alpha-Fetoprotein and/or Small Cell Undifferentiated Histology: A Report from the Children's Hepatic Tumors International Collaboration (CHIC). Cancers (Basel) 2023;15:467. [Crossref] [PubMed]
- Honda M, Uchida K, Irie T, et al. Recent advances in surgical strategies and liver transplantation for hepatoblastoma. Cancer Med 2023;12:3909-18. [Crossref] [PubMed]
- Wu X, Wang J, Duan Y, et al. Surgical resection of pediatric PRETEXT III and IV hepatoblastoma: A retrospective study investigating the need for preoperative chemotherapy. Front Pediatr 2022;10:878095. [Crossref] [PubMed]
- Hiyama E, Hishiki T, Watanabe K, et al. Mortality and morbidity in primarily resected hepatoblastomas in Japan: Experience of the JPLT (Japanese Study Group for Pediatric Liver Tumor) trials. J Pediatr Surg 2015;50:2098-101. [Crossref] [PubMed]
- Yuan XJ, Wang HM, Jiang H, et al. Multidisciplinary effort in treating children with hepatoblastoma in China. Cancer Lett 2016;375:39-46. [Crossref] [PubMed]
- Hiyama E. Current therapeutic strategies for childhood hepatic malignant tumors. Int J Clin Oncol 2013;18:943-5. [Crossref] [PubMed]
- Nguyen R, McCarville MB, Sykes A, et al. Rapid decrease of serum alpha-fetoprotein and tumor volume predicts outcome in children with hepatoblastoma treated with neoadjuvant chemotherapy. Int J Clin Oncol 2018;23:900-7. [Crossref] [PubMed]
- Angelico R, Grimaldi C, Gazia C, et al. How Do Synchronous Lung Metastases Influence the Surgical Management of Children with Hepatoblastoma? An Update and Systematic Review of the Literature. Cancers (Basel) 2019;11:1693. [Crossref] [PubMed]
- Trobaugh-Lotrario AD, Meyers RL, Feusner JH. Outcomes of Patients With Relapsed Hepatoblastoma Enrolled on Children's Oncology Group (COG) Phase I and II Studies. J Pediatr Hematol Oncol 2016;38:187-90. [Crossref] [PubMed]
- Hishiki T, Watanabe K, Ida K, et al. The role of pulmonary metastasectomy for hepatoblastoma in children with metastasis at diagnosis: Results from the JPLT-2 study. J Pediatr Surg 2017;52:2051-5. [Crossref] [PubMed]