Transoral endoscopic thyroidectomy: current state of the art—a systematic literature review and results of a bi-center study
Introduction
For the past 90 years, since its introduction in 1906, the thyroidectomy has remained a standardized surgical procedure in line with the experiences and developments of Emil Theodor Kocher (1). Intraoperative neuromonitoring and the use of optical aids have assisted in developing the procedure into a safe and successful operation (2-4). The rates of transient and permanent recurrent laryngeal never (RLN) palsy have dropped down to 2.7% and 0.8% respectively (5).
Nevertheless, complication rates in thyroid surgery remain high: in an Italian multicenter study of 14,934 patients, Rosato and colleagues found transient complications in 17.4% of patients and permanent complications in 7.1% (6). Patients are most affected by swallowing disorders, dysphonia and dyspnea, wrinkling, and the visible scars. Therefore, in the mid-nineties of the last century, first attempts were made to apply the very effective laparoendoscopic technique, then used in general surgery, to the surgery of thyroid and parathyroid glands. Gagner from Cleveland, US, Hüscher from Esine, Italy, and Yeung from Hong Kong, China were the protagonists of this new approach, using small cervical incisions and laparoendoscopic instruments as well as endoscopes for this purpose (7-9).
At that time, endoscopic thyroid surgery developed in different directions in Europe, the United States and Asia. In Italy, Miccoli adopted the idea of the laparoendoscopic technique and developed his minimally invasive video-assisted thyroidectomy (MIVAT: minimized incision length in the classical position) which has since become wide spread in Europe and America (10,11); Terris stated in 2008 “that MIVAT now represents state-of-the-art management of carefully selected patients when performed in the hands of appropriately trained surgeons” (12). Moreover, MIVAT demonstrated superiority to the conventional thyroidectomy in regard to postoperative pain, patient satisfaction, voice function, and swallowing outcomes (13).
Extra cervical approaches (axillary, breast, chest, and combined approaches) were developed in Asia due to cultural and religious differences in the perception of scars on the visible neck region (14-16). However, the extensive dissection necessary to reach the target region means these approaches do not comply with the term minimally invasive, even though they have reached the goal of invisibility in the neck approach for thyroidectomy. Astonishingly, the postoperative pain in these extra-cervical approaches does not differ significantly to standard or minimized incision length (MIVAT) thyroidectomies (17-21). Ultimately, all extra-cervical approaches leave visible scars, even when not located in the anterior neck region.
Consequently, minimally invasive approaches located closer to the thyroid were sought. In 2008, Witzel reported a transoral, single port approach for thyroid surgery which had proved feasible in an animal study (22). This approach was further elaborated on by Karakas et al. and applied clinically to two patients (23,24) with serious complications in one patient. The group finally terminated the ongoing study due to the rate of serious complications and declared the single-port approach to be “nonsense” at that time (25).
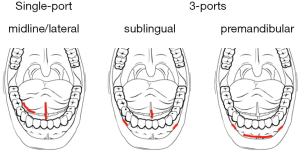
At the same time, our group developed a 3-port transoral approach for endoscopic minimally invasive thyroidectomy (eMIT), which overcame the limitations of the principal communication of Witzel and Karakas (Figure 1); eMIT was proved feasible and safe in anatomical, ultrasound, and animal studies (26-28). On the 18th of March 2009, prior to the Karakas group, this approach was successfully applied clinically for the first time ever in a 53-year-old male (29) and was followed up by a proof-of-concept study (30).
In November 2011 the principal author was invited to Xiamen, China to attend a conference on thyroid surgery and to present the method. During this stay, the first Asian patient underwent a thyroidectomy via the transoral route (31). Subsequent to this successful start, we conducted a prospective cohort study in Xiamen, China and Borna, Germany, which will be reported on later.
Following the scope of the conference in China, a rapid upcoming interest in this challenging new approach was seen in the Asia-Pacific region (32-38). Most recently, Anuwong from Bangkok, Thailand published his experiences in the first 60 patients treated by transoral thyroidectomy (39): a hemi thyroidectomy (single nodules) was performed in 42 patients and a total thyroidectomy or Hartley-Dunhill procedure in 22 patients (multinodular goiters, Graves’ disease). Two cases displayed a papillary carcinoma, and a total thyroidectomy with central neck dissection (level VII) was performed. Median cut-suture-time was 115.5 min and the median blood loss was 30 mL. Two patients complained of a 2-month long transient hoarseness. No mental nerve injury or infections were found. Anuwong concluded the transoral endoscopic thyroidectomy (TOET) to be safe and feasible, and resulting in no visible scarring leading to ideal cosmetic results.
Based on the published data and the results of a prospective cohort study performed in China and Germany, we want to outline the current state of the art of TOET.
Methods
A systematic literature search was performed in PubMed and the results of anatomical, animal, and other published studies regarding the transoral approach (single- or 3-port) were analyzed (Figure 2). Additionally, the results of studies on TOET from different centers, which were presented at the 1st International Thyroid NOTES Conference on the 3rd and 4th of February 2016 at the Police General Hospital in Bangkok, Thailand, were analyzed together with the published data.

After the first successful TOET procedure in Asia (11/12/2011), G. Wu from Xiamen, China also started a prospective cohort study according to the principles of the ongoing study by the principal author. The data was therefore pooled and analyzed together. The surgical method of the eMIT procedure (3-port sublingual) had already been presented elsewhere (30). Indications for surgery, cut-suture-times, intraoperative blood loss, resected specimen volumes, histopathologic findings, and complications were recorded.
Results
Systematic literature review
The systematic search for related publications in PubMed (11/01/2016) revealed 25 eligible studies describing results of cadaver, animal and ultrasound studies as well as human applications; an additional 11 publications dealing with TOET were identified in different databases (Embase, grey literature).
There were only six suitable publications regarding the single-port approach proposed by Witzel et al. (22), three of which dealt with human applications (Table 1). Seven patients were treated by the approach and the group most familiar with it terminated an ongoing study due to serious complications (25).

Full table
The 3-port-approach (26,42), as developed and proposed by our group, gained more interest worldwide. The method proved feasible in 12 studies on 85 cadavers from Germany, China, Korea, and the USA (Table 2). Additional animal studies in Germany and Korea were able to demonstrate the safety of the TOET in pigs (28,35,50).

Full table
On the 3rd and 4th of February 2016, the 1st International Thyroid NOTES Conference took place at the Police General Hospital in Bangkok, Thailand and all centers performing TOET worldwide (Germany, China, Japan, Korea, Thailand, and India) presented their experiences. Together with the published studies (Table 3) at this time, 477 patients had undergone transoral thyroidectomies worldwide. The complication rates were comparable or even better than the rates reported in conventional, MIVAT, endoscopic or robotic approaches and the postoperative course regarding pain and swallowing function seemed favorable for the TOET-procedures.

Full table
The German-Sino bi-center study
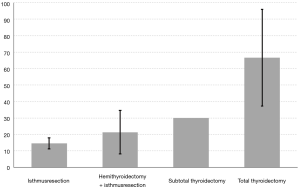
A prospective cohort study was performed between March 2009 and January 2016 in Xiamen, China and Borna, Germany (authors T Wilhelm and G Wu). A total of 96 patients [92 females with a mean age of 36±10 years (standard deviation) and 4 males aged 48±4 years] were treated by TOET using the 3-port bi-vestibular and sublingual approach. Ten (11%) thyroid isthmus resections, 66 (71%) hemi thyroidectomy and isthmus resections, 10 (11%) subtotal thyroidectomies, and 7 (8%) total thyroidectomies were performed due to existing thyroid nodules or cervical masses. Three cases had to be converted to open surgery due to specimen volume. Therefore 93 cases were eligible for analysis. Cut-suture-times differed depending on the procedure performed (Figure 3) but a decrease in cut-suture-times was noted in all surgical procedures: 78 to 38 minutes in isthmus resection, 283 to 49 minutes in hemi thyroidectomy +/− isthmus resection, 258 to 88 minutes in subtotal thyroidectomy, and 305 to 126 minutes in total thyroidectomy. This was comparable to the study of Yang et al. (51).
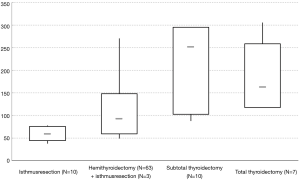
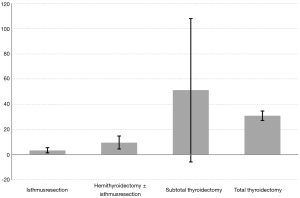
As expected, the average blood loss also depended on the type of surgical procedure but it was considerably low (Figure 4). The same was true of the resected volumes (Figure 5).
In the histopathologic examination: 12 adenomas, 1 cystic lesion, 66 uninodulars, and 14 multinodular changes were described. Additionally a Hashimoto thyroiditis was diagnosed in 11 specimens and a micro papillary carcinoma in two cases.
In the analyzed 93 patients, one permanent recurrent laryngeal nerve palsy (RLNP) (1.1%) as well as 15 cases of transient mental paraesthesia (16.1%) were noted. The mental paraesthesia resolved in all patients within three to four weeks. One local intra oral (1.1%) and 5 neck site infections (5.4%) were noted which could easily be cured by antibiotic treatment and puncture. Three CO2-embolism and in 1 case (1.1%) mediastinal emphysema following raised CO2-pressure above 10 mmHg intraoperative was noted. These side effects also resolved spontaneously within a few days.
Discussion
Thyroidectomy is one of the most common procedures performed in developed countries. It is a safe procedure due to the advancements in surgical techniques, the development of intraoperative neuromonitoring, and the aid of optical magnifying devices (2,4,5). Despite the fact that serious side effects (recurrent laryngeal nerve palsies, hypoparathyroidism) have been able to be minimized over the decades, the procedure leaves a high percentage of patients with unpleasant consequences such as the visible scar and swallowing disorders (6).
During the last two decades therefore, endoscopic procedures have been developed to overcome these after effects. The establishment of the minimal invasive video-assisted thyroidectomy was a first step to minimize the visible consequences of the procedure (10) and this approach became widespread in Europe and the USA. At that time in Asia, more and more centers were attracted to the endoscopic approach from extracervical access points, which led to a rapid development of this approach. Different access points (breast, chest, and axilla) have been established and growing numbers of procedures have been performed in the Asia-Pacific region.
Ultimately however, these endoscopic approaches have not complied with the idea of a minimally invasive approach since the extensive dissection areas have led them to be maximally invasive. A novel concept in modern surgery emerged through the development of natural orifice surgery, first to be performed in a flexible endoscopic manner by Kalloo and colleagues (52). The idea of reaching preformed anatomical layers with a minimal risk of injuries to adjacent nerves and blood vessels seemed very promising. The rapid development of endoscopic instruments and the corresponding video technology have opened a window to apply this approach outside the indications described by Kalloo.
In 2008, Witzel et al. published a single-port approach for transoral thyroidectomy utilizing an axilloscope measuring 20 mm in diameter and their first results in an animal study (22). However, this approach was not purely endoscopic but rather a hybrid one, since they needed an additional skin incision above the larynx. Karakas and colleagues followed this initial idea and also performed cadaver and animal studies prior to their first clinical applications (23,24). The group finally aborted the single-port approach due to serious complications (permanent hypoglossal palsy) in their first patients (25).
In January 2008, inspired by the initial communication of Witzel, a new 3-port approach for TOET was developed (43) and further studied in cadavers and pigs (26,28). An ultrasound study on the distances to reach the target area via the transoral route showed that, when compared to conventional open thyroidectomy approaches, there was no significant difference (27).
Following the presentation of the technique at a conference of thyroid surgeons in Xiamen, China in November 2011, a widespread interest emerged in the Asia-Pacific region and many centers published their experiences of the new approach. Subsequently, a variety of colleagues claimed having developed the transoral approach by publishing new acronyms for the method. It was named TOVANS 2013 (transoral video assisted neck surgery), TOET 2013, ETOVA 2014 (endoscopic thyroidectomy vestibular approach), premandibular approach 2014, TOPOT 2014 (transoral periosteal thyroidectomy), TET 2015 (transoral endoscopic thyroidectomy), and finally TOETVA 2016 (TOET vestibular approach) by different authors (33,36-39,47,50). This has led to a Babylonian linguistic confusion since all approaches are based on the originally described approach. In principal, transoral approaches for thyroidectomy should be classified as single- or 3-port approaches where the latter can be divided into the bi-vestibular/sublingual and the bi-vestibular/premandibular approach (Figure 6).
Nevertheless, the published and most recently (Bangkok, February 2016) communicated results of clinical studies have shown very promising results regarding the TOET. Complication rates are the same or superior to open or endoscopic/robotic assisted procedures and the patients have significant advantages: the procedure results in no visible scar even at the access points in the mouth, swallowing disorders are not communicated by the patients, and postoperative pain levels are significantly lower than in open and extracervical access procedures (51,53).
Therefore TOET has left its state of infancy and is a considerable alternative approach for thyroidectomy. Even in cases of thyroid malignancies, the procedure has proven suitable with or without central neck dissection (33,35,39,40,51) and the implementation of robotic assistance has already been demonstrated (19,44,48).
To further evaluate the transoral approach—including prospective randomized trials—we recommend an internet-based registry to obtain comparable data and establish a consented protocol for pre- and post-operative evaluation of serious complications, swallowing complaints, postoperative pain levels, and cosmetic outcomes. This could possibly be inaugurated by the new Transoral Thyroidectomy Association (TOTA), which was founded on the 4th of February 2016 during the 1st International Thyroid NOTES Conference in Bangkok, Thailand.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Chengzhong Cai (National Center for Toxicological Research, Food and Drug Administration, USA; Shanghai 10th People’s Hospital, Tongji University, Shanghai, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.12.62). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hannan SA. The magnificent seven: a history of modern thyroid surgery. Int J Surg 2006;4:187-91. [Crossref] [PubMed]
- Flisberg K, Lindholm T. Electrical stimulation of the human recurrent laryngeal nerve during thyroid operation. Acta Otolaryngol Suppl 1969;263:63-7. [PubMed]
- Canino V, Massaglia F, Remonda G, et al. La tiroidectomia totale nelle recidive di gozzo (osservazioni anatomo-chirurgiche con l'ausilio del microscopio operatorio). Chir Ital 1992;44:223-9. [PubMed]
- Nielsen TR, Andreassen UK, Brown CL, et al. Microsurgical technique in thyroid surgery—a 10-year experience. J Laryngol Otol 1998;112:556-60. [Crossref] [PubMed]
- Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 2004;136:1310-22. [Crossref] [PubMed]
- Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 2004;28:271-6. [Crossref] [PubMed]
- Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 1996;83:875. [Crossref] [PubMed]
- Hüscher CS, Chiodini S, Napolitano C, et al. Endoscopic right thyroid lobectomy. Surg Endosc 1997;11:877. [Crossref] [PubMed]
- Yeung HC, Ng WT, Kong CK. Endoscopic thyroid and parathyroid surgery. Surg Endosc 1997;11:1135. [Crossref] [PubMed]
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [Crossref] [PubMed]
- Miccoli P, Biricotti M, Matteucci V, et al. Minimally invasive video-assisted thyroidectomy: reflections after more than 2400 cases performed. Surg Endosc 2016;30:2489-95. [Crossref] [PubMed]
- Terris DJ. Effect of video-assisted thyroidectomy on the risk of early postthyroidectomy voice and swallowing symptoms. World J Surg 2008;32:701. [Crossref] [PubMed]
- Lombardi CP, Raffaelli M, D'Alatri L, et al. Video-assisted thyroidectomy significantly reduces the risk of early postthyroidectomy voice and swallowing symptoms. World J Surg 2008;32:693-700. [Crossref] [PubMed]
- Ikeda Y, Takami H, Sasaki Y, et al. Endoscopic neck surgery by the axillary approach. J Am Coll Surg 2000;191:336-40. [Crossref] [PubMed]
- Ohgami M, Ishii S, Arisawa Y, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 2000;10:1-4. [Crossref] [PubMed]
- Shimazu K, Shiba E, Tamaki Y, et al. Endoscopic thyroid surgery through the axillo-bilateral-breast approach. Surg Laparosc Endosc Percutan Tech 2003;13:196-201. [Crossref] [PubMed]
- Alesina PF, Rolfs T, Ruhland K, et al. Evaluation of postoperative pain after minimally invasive video-assisted and conventional thyroidectomy: results of a prospective study. ESES Vienna presentation. Langenbecks Arch Surg 2010;395:845-9. [Crossref] [PubMed]
- Tae K, Ji YB, Jeong JH, et al. Comparative study of robotic versus endoscopic thyroidectomy by a gasless unilateral axillo-breast or axillary approach. Head Neck 2013;35:477-84. [Crossref] [PubMed]
- Kiriakopoulos A, Linos D. Gasless transaxillary robotic versus endoscopic thyroidectomy: exploring the frontiers of scarless thyroidectomy through a preliminary comparison study. Surg Endosc 2012;26:2797-801. [Crossref] [PubMed]
- He QQ, Zhu J, Zhuang DY, et al. Comparative study between robotic total thyroidectomy with central lymph node dissection via bilateral axillo-breast approach and conventional open procedure for papillary thyroid microcarcinoma. Chin Med J (Engl) 2016;129:2160-6. [Crossref] [PubMed]
- Zhang W, Wu QH, Jiang ZG, et al. Subcutaneous dissection area contributes less to endoscopic thyroidectomy-related invasiveness. Surg Endosc 2016;30:4272-8. [Crossref] [PubMed]
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery. Surg Endosc 2010;24:1261-7. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery--development of a new transoral technique. Surgery 2011;150:108-15. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral parathyroid surgery—a new alternative or nonsense? Langenbecks Arch Surg 2014;399:741-5. [Crossref] [PubMed]
- Wilhelm T, Harlaar JJ, Kerver A, et al. Surgical anatomy of the floor of the oral cavity and the cervical spaces as a rationale for trans-oral, minimal-invasive endoscopic surgical procedures: results of anatomical studies. Eur Arch Otorhinolaryngol 2010;267:1285-90. [Crossref] [PubMed]
- Wilhelm T, Krüger J. Ultrasound studies on the shift of cervical tissues in different head and neck positions--impact on transoral endoscopic, minimally invasive and conventional thyroid surgery. Ultrasound Med Biol 2011;37:1430-5. [Crossref] [PubMed]
- Wilhelm T, Benhidjeb T. Transoral endoscopic neck surgery: feasibility and safety in a porcine model based on the example of thymectomy. Surg Endosc 2011;25:1741-6. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Video. Endoscopic minimally invasive thyroidectomy: first clinical experience. Surg Endosc 2010;24:1757-8. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Fu JB, Chen QG, Luo YZ, et al. Transoral laparoscopic thyroidectomy: an experience of 5 cases. Chin J Gen Surg 2012;27:279-81.
- Guo PY, Tang ZP, Ding ZH, et al. Surgical anatomy of totally trans-oral video-assisted thyroidectomy. Zhonghua Wai Ke Za Zhi 2011;49:934-7. [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Park JO, Kim CS, Song JN, et al. Transoral endoscopic thyroidectomy via the tri-vestibular routes: results of a preclinical cadaver feasibility study. Eur Arch Otorhinolaryngol 2014;271:3269-75. [Crossref] [PubMed]
- Lee HY, You JY, Woo SU, et al. Transoral periosteal thyroidectomy: cadaver to human. Surg Endosc 2015;29:898-904. [Crossref] [PubMed]
- Wang C, Zhai H, Liu W, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 2014;155:33-8. [Crossref] [PubMed]
- Ng WT. Transoral endoscopic thyroidectomy. Surgical Practice 2013;17:77-8. [Crossref]
- Pai VM, Muthukumar P, Prathap A, et al. Transoral endoscopic thyroidectomy: a case report. Int J Surg Case Rep 2015;12:99-101. [Crossref] [PubMed]
- Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Woo SH. Endoscope-assisted transoralö thyroidectomy using a frenotomy incision. J Laparoendosc Adv Surg Tech A 2014;24:345-9. [Crossref] [PubMed]
- Witzel K, Hellinger A, Kaminski C, et al. Endoscopic thyroidectomy: the transoral approach. Gland Surg 2016;5:336-41. [Crossref] [PubMed]
- Benhidjeb T, Wilhelm T, Harlaar J, et al. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc 2009;23:1119-20. [Crossref] [PubMed]
- Wilhelm T, Harlaar J, Kerver A, et al. Transorale endoskopische Thyreoidektomie. Teil 1: Rationale und anatomische Studien. Chirurg 2010;81:50-5. [Crossref] [PubMed]
- Richmon JD, Holsinger FC, Kandil E, et al. Transoral robotic-assisted thyroidectomy with central neck dissection: preclinical cadaver feasibility study and proposed surgical technique. J Robot Surg 2011;5:279-82. [Crossref] [PubMed]
- Richmon JD, Pattani KM, Benhidjeb T, et al. Transoral robotic-assisted thyroiedectomy: a preclinical feasibilty study in 2 cadavers. Head Neck 2011;33:330-3. [PubMed]
- Su YH, Tang ZP, Ding ZH, et al. Total trans-oral endoscopic thyroidectomy and cervical lymphadenectomy: a human cadavers surgery study. Zhonghua Wai Ke Za Zhi 2013;51:552-5. [PubMed]
- Guo P, Tang Z, Ding Z, et al. Transoral endoscopic thyroidectomy with central neck dissection: experimental studies on human cadavers. Chin Med J (Engl) 2014;127:1067-70. [PubMed]
- Lee HY, Richmon JD, Walvekar RR, et al. Robotic transoral periosteal thyroidectomy (TOPOT): experience in two cadavers. J Laparoendosc Adv Surg Tech A 2015;25:139-42. [Crossref] [PubMed]
- Cai C, Huang Y, Zhang T, et al. Anatomical study of surgical approaches for minimally invasive transoral thyroidectomy: eMIT and TOPP. Minim Invasive Ther Allied Technol 2015;24:340-4. [Crossref] [PubMed]
- Lee HY, Hwang SB, Ahn K-M, et al. The safety of transoral periosteal thyroidectomy—results of swine models. J Laparoendosc Adv Surg Tech A 2014;24:312-7. [Crossref] [PubMed]
- Yang J, Wang C, Li J, et al. Complete endoscopic thyroidectomy via oral vestibular approach versus areola approach for treatment of thyroid disease. J Laparoendosc Adv Surg Tech A 2015;25:470-6. [Crossref] [PubMed]
- Kalloo AN, Singh VK, Jagannath SB, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc 2004;60:114-7. [Crossref] [PubMed]
- Miccoli P, Rago R, Massi M, et al. Standard versus video-assisted thyroidectomy: objective postoperative pain evaluation. Surg Endosc 2010;24:2415-7. [Crossref] [PubMed]