
Synchronous mucinous cystadenoma of the appendix in a patient with colon cancer
Introduction
Appendiceal mucocele is an unusual lesion that is characterized by an appendiceal lumen distended with mucus (1). Mucoceles less than 2 cm in diameter are usually simple retention cysts, while hyperplastic epithelium, cystadenoma, and cystadenocarcinoma are more likely to be greater than 2 cm. Mucinous cystadenoma, a type of appendiceal mucocele, is a rare oncological entity belonging to the benign lesion; however, it can lead to complications of rupture, invasion to adjacent organs or recurrence (2). Mucinous cystadenocarcinoma is a malignant disease and pseudomyxoma peritonei is its most severe complication (3). Accordingly, detection of an appendiceal mucocele prior to operation can help avoid iatrogenic rupture during surgery and reduce the possible risk of mucocele-induced intra-abdominal tumors.
Case presentation
An 82-year-old man was admitted to our hospital with 3 months’ history of abdominal pain associated with hematochezia, and loss of appetite and body weight. He had only a history of hypertensive problems, and there was no history of malignance in his family. Physical examination revealed anemia and slight tenderness in the lower abdominal region. Laboratory investigations showed a hematocrit value of 34.3% and a hemoglobulin value of 11.5 g/dL. Serum level of CA19-9 was within the normal range, but serum level of carcinoembryonic antigen was 10.7 ng/mL. The parameters of other serum biochemistry, chest X-ray, and sonography were also shown with normal values. Colonoscopy examination indicated one tumor at the sigmoid colon, and the entire colon was unobtainable due to bowel obstruction by the tumor. The biopsy specimen showed moderately-differentiated adenocarcinoma.
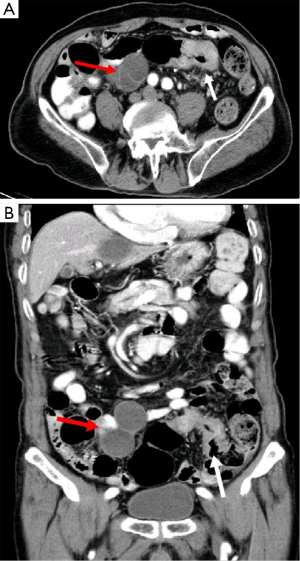
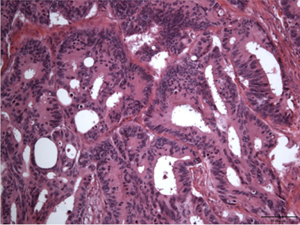
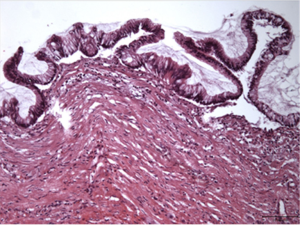
Computed tomography (CT) of the abdomen revealed bowel wall thickness and mesentery inflammation change of sigmoid colon, as well as a cystic mass about 4 cm × 8 cm, lying at the anterior aspect of the cecum. The lesion had smooth walls without surrounding inflammation (Figure 1). After appropriate discussion and consent, the operation of an exploratory laparotomy was done. From the opened wound, a tumor was observed with a diameter of 4 cm at the sigmoidal colon with regional lymph nodes enlargement, and it was radically resected by sigmoidectomy. We found another firm and well-encapsulated tumor with an approximate diameter of 8 cm at the tip of the appendix (Figure 2). It was easily mobilized from adjacent structures. The lesion was removed intact by appendectomy. No metastasis could be palpated or observed in the abdominal cavity. The gross histopathological examination of the resected colon demonstrated an irregular ulcerative and infiltrative tumor measured 4 cm × 4 cm with deep muscular invasion. The appendix showed diffuse globular enlargement measured 4 cm × 8 cm. On cut surfaces of appendiceal tumor, the lumen displayed marked dilations with a thinned walled-cystic luminal filled with thick viscid mucus and involved the proximal half of the appendix. The cystic wall measured 0.4 cm of the maximal thickness. There was no protruded solid part on sections. Total specimens submitted were serially sectioned and the representative parts were embedded in five blocks for section. Microscopically, the section of sigmoid colon showed moderately differentiated colon adenocarcinoma (Figure 3) (stage III-A, grade 2, T2N1M0) according to the American Joint Committee on Cancer tumor-node-metastasis system, composed of marked ulcerative mucosa with necrosis, and the neoplastic cells displayed solid patterns and obvious villoglandular, micropapillary structures with secreting variable amount of mucin. The tumor showed extended through muscularis propria layer, and the focal perineural invasion was also found. The pericolonic regional lymph nodes showed metastatic adenocarcinoma. The sections of the appendiceal tumor demonstrated large amount of glare mucin in a cavity. The inner wall of the fibrotic cyst showed extensive ulcerative mucosa, and lined by a proliferative intestinal type epithelium. The epithelium showed crowded tall columnar cells with basal, elongated, hyperchromatic nuclei, micropapillary configuration with large amounts of apical mucin with low-grade dysplastic changes (Figure 4). No direct invasion of fibromuscular wall by neoplastic glands was found. There was also accompanied by moderately atrophy, fibrosis, and mild inflammation of the underlying cystic wall. No evidence of proximal margin of appendix was involved.

Discussion
The incidence of synchronous primary appendiceal tumor with colorectal cancer in patients is approximately 4 percent (4). These have been observed in high-risk patients with inflammatory bowel disease such as ulcerative colitis (5). Appendiceal mucocele is a tumor that secretes viscid mucus within the lumen and distends the appendix to produce a mucocele. Mucinous cystadenoma, a type of appendiceal mucocele, is defined as a dilated and mucus-filled appendix containing hyperplastic adenomatous mucosa. The disease is rare, and presents in less than 0.3 percent of appendectomies and 8 percent of appendiceal tumors (6-8). It is more frequent in female patients and usually occurs in patients older than 50 years (9). Clinical manifestations can range from asymptomatic to acute abdomen-like symptoms such as abdominal pain, gastrointestinal bleeding, or palpable abdominal mass. It is generally discovered incidentally with radiological study or at the time of laparotomy performed for other reasons.
Appendiceal mucoceles are divided into four groups on the basis of their lining epithelium (2,8). The first group is simple retention mucoceles that result from obstruction of the appendiceal outflow, usually by a fecalith or inflammation change, and are characterized by normal epithelium and mild lumen dilatation that rarely exceeds 2 cm in diameter. The second group is defined by local or diffuse villous hyperplastic epithelium and the luminal dilatation is also mild. The third group is benign mucinous cystadenoma, the most common form, as in the case presented herein. These exhibit mostly epithelial villous adenomatous changes with some degree of epithelial atypia and are characterized by marked distention (up to 6 cm) of the lumen. The fourth group is malignant mucinous cystadenocarcinoma, which exhibits glandular stromal invasion or the presence of epithelial cells in the peritoneal implants. The luminal distention becomes severe. There is a high risk of rupture, either spontaneous or iatrogenic, with consequent development of pseudomyxoma peritonei, which may present with the worst complication.
The prognosis for benign forms of appendiceal mucoceles, including retention mucocels, mucosal hyperplasia, and mucinous cystadenoma is excellent following complete resection. The survival rate of 5 years is approximately 100 percent. For malignant forms, the survival rate correlates with the degree of extension of the tumor and varies between 30 and 80 percent. Once the perforation occurs, epithelial cells escape into the peritoneal cavity and cause a potential fatality for a patient (9,10).
Diagnosis of appendiceal mucocele is often difficult due to asymptomatic property of the disease. Most of the cases are incidental findings at the time of surgery (11,12). However, if the concept is kept in mind, preoperative diagnosis can be of great value particularly in planning of surgery. The diagnostic modalities include ultrasound, barium enema, colonoscopy, and CT scan. On ultrasound images the mucocele appears anechoic or hypoechogenic relative to the mucus component. In some cases, multiple echogenic layers along a dilated appendix are observed as being a specific ‘The Onion Skin Sign’ (13). CT studies have been invaluable in the diagnosis of appendiceal mucocele. It usually reveals a low-attenuation, well-encapsulating, cystic mass with smooth walls located at the base of the cecum, sometimes with mural calcification (13-15). Notably, mucoceles with a diameter of less than 2 cm are rarely malignant but larger mucoceles with a diameter of 6 cm or more are usually associated with cystadenoma or cystadenocarcinoma and a higher perforation rate (20%) (16). Colonoscopy may show the volcano sign, the appendiceal orifice seen in the center of a firm mound covered by normal mucosa or lipoma-like submucosal mass. Colonoscopy is also important for the diagnosis of synchronous colon tumors (17). Double-contrast barium enema may complement colonoscopy in diagnosis of submucosal lesions. However, the diagnosis is usually made intraoperatively or postoperatively on histopathological examination.
Definitive management of an appendiceal mucocele is surgical resection. Margins of the resection should be considered according to the type of mucocele. Perforation of the mucocele is an important factor for recurrence and prognosis. We must pay attention to keep a mucocele intact during operation and avoid dissemination of mucoid material into the peritoneum. Appendectomy is used for simple mucocele or cystadenoma that has negative margins of resection without perforation. Cecal resection is suggested for cystadenoma with a large base, and right hemicolectomy is recommended for cystadenocarcinoma (18). In general, the surgical approach is laparotomy, but laparoscopic surgery may be chosen for simple or non-ruptured mucoceles (19).
Mucocele of the appendix has been shown to be associated with synchronous colonic malignancies. This may result from the embryological derivation of the appendix from the cecum and histologically similarities to the colorectum (20). Thus, patients with this tumor should be systematically checked for other colonic lesions. In our patient, sigmoid colon cancer was diagnosed firstly from colonoscopic examination. Study of the entire colon was not possible because of lumen narrowing due to the colon tumor. From routine CT examination, a cystic mass about 4 cm × 8 cm, lying at the anterior aspect to the cecum was noted. During the operation, we checked this region carefully and found a firm, well-encapsulated tumor located at the tip of the appendix. It was easily mobilized from adjacent structures and resected completely by appendectomy. The frozen histopathological examination result was mucinous cystadenoma of the appendix.
In this case report, we focused on the patient’s colon cancer first, then the cecal tumor was found by routine CT study. An appendiceal mucocele was suspected at that time, so a thorough investigation and the mild mobilization were done during surgical intervention. Such procedures help us prevent iatrogenic perforation and further pseudomyxoma peritonei, as well as providing a good prognosis for the patient.
Synchronous appendiceal mucocele may occur in patients with colon cancer. Histologic differences of the two entities support the synchronous tumors. We are the first to report the case in Taiwan. This is a rare condition of which all clinicians should be made aware. Early recognition of the disease and resection of mucocele can help prevent iatrogenic perforation and further peritoneal contamination. An appendiceal mucocele is reported here synchronously with colon cancer suggesting a careful systemic screening may be necessary before operation.
Acknowledgments
The authors’ contributions were made in any of the following ways: C.-C.Y. wrote the main manuscript and performed the operation, J.-L.C. examined the histological pathology, and Y.-K.L., C.-P.C., and Y.-H.K. revised the manuscript for important intellectual content and provided the final approval for the version to be submitted for publication. All authors read and approved the final manuscript. We thank the patient for permission to use his sample.
Funding: This work was supported by the Ministry of Science and Technology, Taiwan [MOST-105-2311-B-008-003 to Y.-H.K]; the Taoyuan Armed Forces General Hospital [#10403 to C.-C.Y., and #10510 to Y.-H. K.]; and the Landseed Hospital and National Central University Joint Research Foundation [NCU-LSH-105-B-010 to Y.-H.K.]. The funding body has no role in study design; data collection, analysis, and interpretation; and manuscript writing and submission.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2016.12.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sierra-Montenegro E, Sierra-Luzuriaga G, Leone-Stay G, et al. Mucinous cystadenoma of the appendix. Case report. Cir Cir 2010;78:255-8. [PubMed]
- Yakan S, Caliskan C, Uguz A, et al. A Retrospective Study on Mucocele of the Appendix Presented with Acute Abdomen or Acute Appendicitis. Hong Kong Journal of Emergency Medicine 2011;18:144-9.
- Rampone B, Roviello F, Marrelli D, et al. Giant appendiceal mucocele: report of a case and brief review. World J Gastroenterol 2005;11:4761-3. [Crossref] [PubMed]
- Khan MN, Moran BJ. Four percent of patients undergoing colorectal cancer surgery may have synchronous appendiceal neoplasia. Dis Colon Rectum 2007;50:1856-9. [Crossref] [PubMed]
- Lyda MH, Noffsinger A, Belli J, et al. Multifocal neoplasia involving the colon and appendix in ulcerative colitis: pathological and molecular features. Gastroenterology 1998;115:1566-73. [Crossref] [PubMed]
- Ruiz-Tovar J, Teruel DG, et al. Mucocele of the appendix. World J Surg 2007;31:542-8. [Crossref] [PubMed]
- Higa E, Rosai J, Pizzimbono CA, et al. Mucosal hyperplasia, mucinous cystadenoma, and mucinous cystadenocarcinoma of the appendix. A re-evaluation of appendiceal "mucocele". Cancer 1973;32:1525-41. [Crossref] [PubMed]
- Pai RK, Longacre TA. Appendiceal mucinous tumors and pseudomyxoma peritonei: histologic features, diagnostic problems, and proposed classification. Adv Anat Pathol 2005;12:291-311. [Crossref] [PubMed]
- Aho AJ, Heinonen R, Laurén P. Benign and malignant mucocele of the appendix. Histological types and prognosis. Acta Chir Scand 1973;139:392-400. [PubMed]
- Dhage-Ivatury S, Sugarbaker PH. Update on the surgical approach to mucocele of the appendix. J Am Coll Surg 2006;202:680-4. [Crossref] [PubMed]
- Aghahowa EJ, Bharati D, Al-Adwani M. Appendicular mucocele—a case report. Kuwait Med J 2008;40:78-80.
- Bartlett C, Manoharan M, Jackson A. Mucocele of the appendix - a diagnostic dilemma: a case report. J Med Case Rep 2007;1:183. [Crossref] [PubMed]
- Kim SH, Lim HK, Lee WJ, et al. Mucocele of the appendix: ultrasonographic and CT findings. Abdom Imaging 1998;23:292-6. [Crossref] [PubMed]
- Zissin R, Gayer G, Kots E, et al. Imaging of mucocoele of the appendix with emphasis on the CT findings: a report of 10 cases. Clin Radiol 1999;54:826-32. [Crossref] [PubMed]
- Madwed D, Mindelzun R, Jeffrey RB Jr. Mucocele of the appendix: imaging findings. AJR Am J Roentgenol 1992;159:69-72. [Crossref] [PubMed]
- Lau H, Yuen WK, Loong F, et al. Laparoscopic resection of an appendiceal mucocele. Surg Laparosc Endosc Percutan Tech 2002;12:367-70. [Crossref] [PubMed]
- Soweid AM, Clarkston WK, Andrus CH, et al. Diagnosis and management of appendiceal mucoceles. Dig Dis 1998;16:183-6. [Crossref] [PubMed]
- Khan MR, Ahmed R, Saleem T. Intricacies in the surgical management of appendiceal mucinous cystadenoma: a case report and review of the literature. J Med Case Rep 2010;4:129. [Crossref] [PubMed]
- Chiu CC, Wei PL, Huang MT, et al. Laparoscopic resection of appendiceal mucinous cystadenoma. J Laparoendosc Adv Surg Tech A 2005;15:325-8. [Crossref] [PubMed]
- Williams RA, Myers P. Pathology of the Appendix. New York, NY, USA. Chapman and Hall Medical; 1994.


