
Epigenetic profiling of tumor infiltrating lymphocytes
Blocking T cell inhibitory signals, or “checkpoint blockade”, has provided unprecedented clinical results for therapy of cancer (1). Antibodies that block negative interactions between programmed death-1 (PD-1) and programmed death-ligand 1 (PD-L1) allow activation of T cells that recognize tumor antigens and promote immune destruction of the tumor. To determine the activities of T cells of tumor infiltrating lymphocytes (TILs), and to determine which patients will most effectively respond to checkpoint blockade therapies, Schietinger and colleagues developed a novel inducible autochthonous tumor in AST × CreERT2 mice. In this system, they successfully analyzed TIL activity and chromatin remodeling during tumor development (2,3).
Chromatin state correlates with rescue of tumor infiltrating CD8+ T cell function
As a model for human hepatocellular carcinoma (HCC), Schietinger et al. engineered liver-specific expression of SV40 large T antigen (TAg) to initiate malignant transformation (2). In this tumor, TAg was both the tumor-specific antigen and the tumor driver. Using a lox-stop cassette, expression of TAg was activated when the mice were placed on tamoxifen. They reported morphologic alterations in the liver within 8–10 days, early pre-malignant tumors by 30 days, and frank tumors within 3–4 months (4). All mice succumb to HCC by 4–5 months. Thus, although the AST × CreERT2 tumors are initiated in response to one of the strongest oncogenes known, the tumor develops in vivo, a benefit lost in transplantable tumors used in many pre-clinical tumor immunology experiments.
To determine whether tumor-specific T cell dysfunction is reversible, monoclonal T cells from TCR transgenic mice specific the SV40-I epitope (5) were transferred into the AST × CreERT2 mice. Tumor-specific T cells were synchronized with respect to when they entered the tumor and were easily distinguished from the endogenous repertoire by a congenic marker. Naïve transgenic CD8+ T cells were injected into mice one day prior to inducing TAg expression with tamoxifen, so the T cells would differentiate as the tumor developed. The authors showed that T cell dysfunction was reversible until day 8 and by day 30 T cells could no longer be rescued by transfer into an antigen-free wild-type host or treatment with PD-1 blockade (2).
Next Schietinger’s group tested the hypothesis that this irreversible state of dysfunction is epigenetically imprinted in an elegant follow-up manuscript published in Nature (3). Epigenetic events are chromatin-based modifications that regulate DNA-templated processes such as transcription, DNA repair, and cellular replication. For decades now, the role of epigenetics in cancer has been investigated with the goal of identifying targets for therapies. The excitement in understanding how epigenetics plays a part in cancer biology has been renewed with the development of new techniques that incorporate next generation sequencing (6). Original methods to investigate epigenetic characteristics were only compatible with large numbers of homogeneous cells (typically cultured in vitro), but new technologies facilitate analysis of samples containing few primary cells (7), such as primary T cells found in the tumor microenvironment. Despite studies that have defined molecular programming of T cell activity (8-13), little is known regarding the chromatin and transcriptional dynamics that program TIL activity.
Using the powerful combination of epigenetic and transcriptional profiling to accurately identify the molecular programming defining T cell function, Schietinger’s group showed temporal changes in the chromatin state that define tumor-specific T cell dysfunction (3). Using the Assay for Transposase-Accessible Chromatin (ATAC-seq) in combination with RNA-sequencing (RNA-seq), they showed that tumor-specific T cells differentiated through two distinct chromatin states that correlate with the reversibility identified in their first manuscript (2). The earlier time points (day 7 and before) corresponded to a more plastic reversible state, and later time points (day 14 and after) corresponded to a fixed irreversible state. Notably, when comparing T cells in the tumor relative to T cells that were activated by Listeria monocytogenes expressing TAg, the enhancer peaks in the Ifng locus that were normally open during effector differentiation were inaccessible when the T cells were dysfunctional. Consistently, negative regulators such as Ctla4, Pdcd1, and Tigit had increased accessibility. The NFAT transcription factor family members C1 and C2, which regulate T cell function, were also accessible in the TILs.
To distinguish readily identifiable proteins that associate with the plastic or the fixed chromatin state in TILs, RNA sequencing was analyzed for cell surface proteins and confirmed by flow cytometry. CD38, CD101, and CD30L expression were up-regulated in the fixed T cells, and CD5 was up-regulated in the plastic cells. Intergenic and intronic peaks in the CD38 locus were uniquely accessible in the fixed state. The authors suggest that these markers may help identify patients who will respond to PD1 therapy as more plastic T cells are amenable to reprogramming before they convert to a dysfunctional state.
AST × CreERT2vs. B16-Ova study
Another group recently reported analyses of tumor-specific T cells from another tumor model using similar techniques (14). Mognol and colleagues performed ATAC- and RNA-seq on Ova-specific TILs from the transplantable B16-Ova melanoma. In these experiments, CD8+ Ova-specific TILs from OT-1 transgenic mice were stimulated in culture and injected into wild-type mice bearing established B16-Ova tumors. Eight days later, TILs were isolated and analyzed. The control in these experiments were transferred tumor nonreactive T cells from P14 transgenic mice. This study was designed to understand exhaustion and focused on finding NFAT and Nr4a as key transcription factors.
A number of similarities and differences were observed from results of both the AST × CreERT2 and B16-Ova experiments. Both studies analyzed TILs with an exhausted molecular signature (PD-1+, Tim-3+) and dysfunctional phenotypes were observed only in the tumor-reactive T cells. Specifically, both systems find expression of exhaustion genes on the tumor antigen-specific T cells, but not the irrelevant transferred T cells: OT-1 T cells were not exhausted in the AST × CreERT2 tumors (2), and P14 T cells were not exhausted in the B16-Ova tumors (14). In addition, anti-PD1/PD-L1 treatment led to reversal of dysfunction in both systems, depending on the conditions. Lastly, the role of NFAT transcription factor family members were revealed as an important promoter of T cell exhaustion. However, likely due to the differences in the tumor models and experimental methods from each study (Table 1), we found little overlap, just 5 genes overlapped between the RNA-seq and ATAC-seq datasets (Figure 1). The disparity between these two studies emphasizes the importance of carefully choosing the model and experimental methods to address the hypotheses in question.
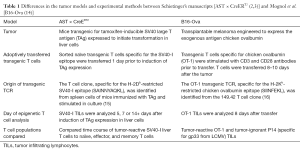
Full table

Summary
Schietinger’s group has developed an inducible autochthonous tumor model, the AST × CreERT2 model, which faithfully represents the pathogenesis of cancer. Genetic initiation of tumorigenesis and transfer of naïve T cell prior to tumorigenesis avoids the inflammation associated with transfer of large numbers of tumor cells (17) and allows in situ differentiation of cytotoxic T cells, respectively. Using the inducible SV40 model, Schietinger and colleagues have confirmed the power of combined chromatin and transcriptional profiling to accurately identify the molecular programing defining cancer-associated immune cell function. Their recent Nature paper convincingly shows two discrete chromatin states in TILs: a more plastic-reversible state, which they propose reflects TILs that can respond to checkpoint blockade therapies, and a fixed state, which is not reversible and is not expected to respond to such therapies. We eagerly await future publications suggesting whether the cell-surface markers identified in this study will distinguish these states and whether they predict responses to checkpoint blockade therapies in human cancer patients. The disparities observed in the molecular programming of TIL function between the different scientific groups may reflect differences in TIL programming in diverse human tumor microenvironments. Thus, we expect that studies designed to further our understanding of the programs that dictate tumor-type-specific T cell dysfunction will point to new targets and strategies that transform dysfunctional T cells into mediators of potent antitumor immunity in diverse tumor microenvironment settings.
Acknowledgments
Funding: The authors are grateful for funds from the Department of Immunology and Microbiology Pilot Award Program (University of Colorado, School of Medicine), which made this study possible.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by the Section Editor Chen Qian (Center for Inflammation & Epigenetics, Houston Methodist Hospital Research Institute, Houston, TX, USA).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tcr.2017.08.20). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 2012;366:2443-54. [Crossref] [PubMed]
- Schietinger A, Philip M, Krisnawan VE, et al. Tumor-Specific T Cell Dysfunction Is a Dynamic Antigen-Driven Differentiation Program Initiated Early during Tumorigenesis. Immunity 2016;45:389-401. [Crossref] [PubMed]
- Philip M, Fairchild L, Sun L, et al. Chromatin states define tumour-specific T cell dysfunction and reprogramming. Nature 2017;545:452-6. [Crossref] [PubMed]
- Cullen JM, Sandgren EP, Brinster RL, et al. Histologic characterization of hepatic carcinogenesis in transgenic mice expressing SV40 T-antigens. Vet Pathol 1993;30:111-8. [Crossref] [PubMed]
- Staveley-O'Carroll K, Schell TD, Jimenez M, et al. In vivo ligation of CD40 enhances priming against the endogenous tumor antigen and promotes CD8+ T cell effector function in SV40 T antigen transgenic mice. J Immunol 2003;171:697-707. [Crossref] [PubMed]
- Dawson MA, Kouzarides T. Cancer epigenetics: from mechanism to therapy. Cell 2012;150:12-27. [Crossref] [PubMed]
- Dirks RA, Stunnenberg HG, Marks H. Genome-wide epigenomic profiling for biomarker discovery. Clin Epigenetics 2016;8:122. [Crossref] [PubMed]
- Wei G, Wei L, Zhu J, et al. Global mapping of H3K4me3 and H3K27me3 reveals specificity and plasticity in lineage fate determination of differentiating CD4+ T cells. Immunity 2009;30:155-67. [Crossref] [PubMed]
- Ansel KM, Djuretic I, Tanasa B, et al. Regulation of Th2 differentiation and Il4 locus accessibility. Annu Rev Immunol 2006;24:607-56. [Crossref] [PubMed]
- Seumois G, Chavez L, Gerasimova A, et al. Epigenomic analysis of primary human T cells reveals enhancers associated with TH2 memory cell differentiation and asthma susceptibility. Nat Immunol 2014;15:777-88. [Crossref] [PubMed]
- Nicodemus-Johnson J, Naughton KA, Sudi J, et al. Genome-Wide Methylation Study Identifies an IL-13-induced Epigenetic Signature in Asthmatic Airways. Am J Respir Crit Care Med 2016;193:376-85. [Crossref] [PubMed]
- Bønnelykke K, Ober C. Leveraging gene-environment interactions and endotypes for asthma gene discovery. J Allergy Clin Immunol 2016;137:667-79. [Crossref] [PubMed]
- Moskowitz DM, Zhang DW, Hu B, et al. Epigenomics of human CD8 T cell differentiation and aging. Sci Immunol 2017;2. [PubMed]
- Mognol GP, Spreafico R, Wong V, et al. Exhaustion-associated regulatory regions in CD8+ tumor-infiltrating T cells. Proc Natl Acad Sci U S A 2017;114:E2776-85. [Crossref] [PubMed]
- Tanaka Y, Tevethia MJ, Kalderon D, et al. Clustering of antigenic sites recognized by cytotoxic T lymphocyte clones in the amino terminal half of SV40 T antigen. Virology 1988;162:427-36. [Crossref] [PubMed]
- Kelly JM, Sterry SJ, Cose S, et al. Identification of conserved T cell receptor CDR3 residues contacting known exposed peptide side chains from a major histocompatibility complex class I-bound determinant. Eur J Immunol 1993;23:3318-26. [Crossref] [PubMed]
- Dranoff G. Experimental mouse tumour models: what can be learnt about human cancer immunology? Nat Rev Immunol 2011;12:61-6. [PubMed]


