
Conservative treatment for residual lung congestion after left upper trisegmentectomy: a case report
Highlight box
Key findings
• We report a case of isolated area and residual pulmonary congestion after segmentectomy for lung cancer that was relieved by conservative treatment.
What is known and what is new?
• Although pulmonary torsion is a typical complication of segmentectomy, complications with isolated area and residual lung congestion are rare. Some cases can be treated with conservative treatment.
What is the implication, and what should change now?
• The identification of the intersegmental line using the inflation-deflation line is not sufficient to evaluate blood flow and should be evaluated with the use of ICG.
Introduction
Lung cancer is the most common cancer that causes the most deaths among all types of cancer (1). Currently, the standard treatment for lung cancer surgery is lobectomy. In lobectomy, one or more lung lobes and the surrounding lymph nodes are removed depending on the location and the size of the tumor. In Japan, segmentectomy is chosen in 10.3% of lung cancer surgeries and is a relatively frequently performed procedure (2). However, segmentectomy is relatively difficult compared with lobectomy, and it sometimes causes serious complications because only the vessels leading to the segment need to be selected for resection (3). In particular, left upper trisegmentectomy (LUTS) is one of the most common and well-known procedures performed by thoracic surgeons. Residual pulmonary congestion after LUTS often leads to surgical intervention (4). Differentiating between pulmonary torsion and residual pulmonary congestion is difficult, and in the case of torsion, surgery might be required. We report a case of improvement of congestion in the residual lung after LUTS with conservative treatment and careful follow-up by computed tomography (CT). We present the following article in accordance with the CARE reporting checklist (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2104/rc).
Case presentation
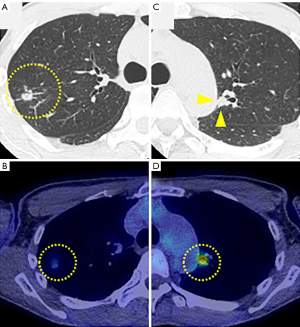
The patient was a 65-year-old male current smoker. CT showed bilateral nodular lesions in the lungs. The left lesion was a solid nodule measuring 10 mm in the area of S1+2b, and fluorodeoxyglucose-positron emission-CT showed abnormal [18F]-fluorodeoxyglucose (FDG) uptake (maximum standardized uptake value: 5.2). The right-sided lesion was an 8-mm partly solid nodule in S3a with mild FDG uptake (maximum standardized uptake value: 2.0) (Figure 1A-1D). The diagnosis was suspected bilateral lung cancer (T1aN0M0, stage IA1). Resection of bilateral lesions was planned. Taking into consideration that the lesion in the left side had a higher maximum standardized uptake value and a solid nodule, we initially performed LUTS (ND1b) for the partially solid ground-glass nodule in the left side. We decided to perform LUTS including S3 in order to dissect the hilar lymph node. Intraoperatively, there was no anomaly in the location or branching of the pulmonary vessels or the bronchi. V1–3, A1+2, A3, and B1–3 were divided and cut using automatic sutures, and A4+5 (mediastinal type) was preserved. We identified the intersegmental line using the inflation-deflation line. The intersegmental line was cut using automatic sutures. There were no intraoperative complications.
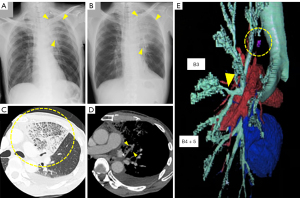
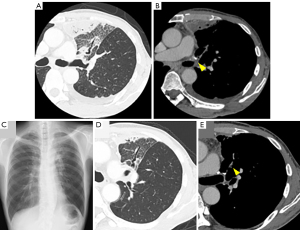
On the next day after surgery, blood sputum was observed. On the fourth postoperative day, the patient had a fever, and laboratory tests showed the presence of an inflammatory reaction (white blood cell count: 11.4×109/L, C-reactive protein concentration: 15.7 mg/dL), although the saturation of oxygen was maintained. A chest X-ray showed an infiltrative shadow in the left upper lung field (Figure 2A,2B). Contrast-enhanced chest CT on the same day showed extensive frosted shadows in the lingual area and thickening of the interlobular septa (Figure 2C,2D). Additionally, the left S3 remained and the S3 segment was an isolated segment. Retrospectively, we found that B3 branched from B4+5 in a preoperative three-dimensional-CT (3DCT) scan (Figure 2E). Additionally, A4+5 was preserved, but V4+5 was thin with poor flow, which might have caused the congestion in the lingular segment. Bronchoscopy showed no findings of pulmonary torsion. Because the patient was well oxygenated and had few subjective symptoms, conservative treatment with antibiotics (PIPC/TAZ 4.5 g × 3/day) was started. Contrast-enhanced chest CT was performed on postoperative days 5 and 13 to confirm that there was no progression of congestion and poor flow of V4+5 (Figure 3A,3B). The findings of pulmonary congestion by chest X-ray and an inflammatory reaction gradually improved. The patient was treated with antibiotics until the 27th postoperative day and discharged home on the same day. Follow-up CT 2 months after surgery showed no recurrence of the congestion (Figure 3C-3E). Three months after surgery, we performed a partial resection of the right-sided lesion, and the postoperative course was uneventful.
All procedures performed in this study were in accordance with the ethical standards of the institutional and with the Helsinki Declaration (as revised in 2013). This study was approved by institutional review board of Kyushu University (No. 2019-232). Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Increasingly, segmentectomy is indicated not only for patients with a poor lung condition or multiple primary lesions, but also when less invasive lung cancer is detected at an early stage. The advantage of segmentectomy is that respiratory function is maintained postoperatively. However, complications after segmentectomy have been reported. A previous report showed that complications were significantly higher in patients who underwent LUTS and lingular segmentectomy (4).
Koike et al. described the four complications of atelectasis, pulmonary torsion, an isolated segment, and a hematoma after LUTS (4). Among them, an isolated segment is a rare complication that occurs after lung resection. In an isolated segment, the pulmonary arterioles and bronchial arteries of the remaining lung are separated and isolated, resulting in inadequate flow, congestion, and necrosis. The cause of an isolated segment may be anomalies of the pulmonary artery and bronchi, or an inaccurate segment dissection line. In the present case, two complications occurred simultaneously. Firstly, the part of S3 was isolated because B3 branched off from B4+5, and the major feeding vessels and drainage veins, A3 and V3, were dissected. Secondly, the trisegmentectomy caused a slight displacement of the residual lung, which flexed V4+5, resulting in poor flow and congestion in S4+5 segment. Although the isolated segment lacks a major drainage vein, it may be possible to compensate with a small drainage vein to the adjacent segment. In this case, V4+5 drainage vein was slightly open, suggesting that the isolated area was drained through it. If there is a possibility of necrosis in the isolated segment due to interruption of flow, resection of the remaining lung should be considered. Conservative treatment of residual lung congestion is also an option if the drainage vein is not obstructed. Careful follow-up, including contrast-enhanced CT, as well as monitoring vital signs and blood sampling, is necessary. In this case, during the conservative treatment, CT was performed twice to confirm that there was no exacerbation in the imaging findings. In this case, A3 and V3 were resected without resection of B3, which resulted in congestion and an isolated area of S3. However, because follow-up CT showed no necrosis or abscess in the isolated area and the inflammatory findings were improving, surgery was not performed.
An important complication after LUTS is axial torsion of the residual lung, which is difficult to differentiate from an isolated segment (5,6). Axial torsion of the residual lung is a serious complication that usually requires re-operation, and differentiating between this complication and an isolated segment is difficult. However, the clinical presentation of axial torsion and an isolated segment is similar. In both cases, a chest X-ray shows decreased air content in the affected area, vital abnormalities, and inflammatory findings, and there may be complaints such as blood sputum and chest pain. A diagnosis by bronchoscopy alone is difficult, and contrast-enhanced CT is considered to be required, including an evaluation of blood flow.
Accurate recognition of abnormalities of vessels and bronchi by a CT scan of thin slices and 3DCT before segmentectomy may help clinicians to prevent these complications with an isolated segment (7-9). With regard to the surgical technique, it is likely that the use of ICG would have allowed for a more precise incision line without leaving an S3 area. It is important to use ICG to identify the intersegmental plane to prevent isolated segment in segmentectomies (10,11).
Conclusions
In conclusion, we experienced a case of residual pulmonary congestion after LUTS that resolved with conservative treatment. Careful follow-up of the patient’s general condition and imaging studies are considered to be important.
Acknowledgments
We thank Ellen Knapp, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2104/rc
Peer Review File: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2104/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-22-2104/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and with the Helsinki Declaration (as revised in 2013). This study was approved by institutional review board of Kyushu University (No. 2019-232). Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70:7-30. [Crossref] [PubMed]
- Committee for Scientific Affairs. Thoracic and cardiovascular surgery in Japan in 2016: Annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2019;67:377-411. [Crossref] [PubMed]
- Miyasaka Y, Oh S, Takahashi N, et al. Postoperative complications and respiratory function following segmentectomy of the lung - comparison of the methods of making an inter-segmental plane. Interact Cardiovasc Thorac Surg 2011;12:426-9. [Crossref] [PubMed]
- Koike Y, Hattori A, Matsunaga T, et al. Postsurgical residual lung complications following left upper trisegmentectomy. Eur J Cardiothorac Surg 2020;57:472-7. [PubMed]
- Mariolo AV, Seguin-Givelet A, Gossot D. Fatal Stroke After Reoperation for Lobar Torsion. Ann Thorac Surg 2020;110:e51-3. [Crossref] [PubMed]
- Taira N, Kawasaki H, Takahara S, et al. Lingular segment torsion following a left upper division segmentectomy. Int J Surg Case Rep 2017;39:77-9. [Crossref] [PubMed]
- Shimizu K, Nagashima T, Ohtaki Y, et al. Analysis of the variation pattern in right upper pulmonary veins and establishment of simplified vein models for anatomical segmentectomy. Gen Thorac Cardiovasc Surg 2016;64:604-11. [Crossref] [PubMed]
- Maki R, Miyajima M, Ogura K, et al. Anatomy of the left subsuperior segment for segmentectomy. Surg Today 2022;52:1054-62. [Crossref] [PubMed]
- Zhang M, Liu D, Wu W, et al. Preoperative 3D-CT bronchography and angiography facilitates single-direction uniportal thoracoscopic anatomic lobectomy. Ann Transl Med 2019;7:526. [Crossref] [PubMed]
- Sun Y, Zhang Q, Wang Z, et al. Is the near-infrared fluorescence imaging with intravenous indocyanine green method for identifying the intersegmental plane concordant with the modified inflation-deflation method in lung segmentectomy? Thorac Cancer 2019;10:2013-21. [Crossref] [PubMed]
- Yotsukura M, Okubo Y, Yoshida Y, et al. Indocyanine green imaging for pulmonary segmentectomy. JTCVS Tech 2021;6:151-8. [Crossref] [PubMed]


